Recent Insights Into the Role of Vitamin B12 and Vitamin D Upon Cardiovascular Mortality: a Systematic Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Leaflet View the Patient Leaflet in PDF Format
Read all of this leaflet carefully before you are given this within the body usually caused by diseases of the gut, liver any other medicines. Driving and using machines medicine because it contains important information for or gall bladder. • Medicines for heart disease such as digoxin or verapamil as Ergocalciferol may cause drowsiness or your eyes to you. It is important that you have this medicine so that your these can cause high levels of calcium in the blood leading become very sensitive to light. If this happens to you, do bones and teeth form properly. • Keep this leaflet. You may need to read it again. to an irregular or fast heart beat. not drive or use machinery. • If you have any further questions, ask your doctor or nurse. 2. What you need to know before you are given • Antacids containing magnesium for indigestion. If you are 3. How you will be given Ergocalciferol • If you get any side effects, talk to your doctor or nurse. Ergocalciferol on kidney dialysis this can lead to high levels of Ergocalciferol will be given to you by your doctor or nurse. This includes any possible side effects not listed in this magnesium in the blood which causes muscle weakness, Important: Your doctor will choose the dose that is right leaflet. See section 4. You must not be given Ergocalciferol: low blood pressure, depression and coma. for you. In this leaflet, Ergocalciferol 300,000 IU Injection BP will • if you are allergic to ergocalciferol (vitamin D) or any of the other • Thiazide diuretics (‘water tablets’) to relieve water You will be given Ergocalciferol by your doctor or nurse as an injection into a muscle. -

Family Practice
THE JOURNAL OF FAMILY PRACTICE Emmanuel Andrès, MD, B12 deficiency: A look beyond Laure Federici, MD, Stéphan Affenberger, MD pernicious anemia Department of Internal Medicine, Diabetes and Metabolic Diseases, Food-B12 malabsorption—not pernicious anemia—is the Hôpitaux Universitaires de Strasbourg, leading cause of B12 malabsorption. It’s also very subtle Strasbourg, France emmanuel.andres @chru-strasbourg.fr Practice recommendations such as its link to Helicobacter pylori • Mild, preclinical B deficiency infection and long-term antacid and bi- Josep Vidal-Alaball, MD 12 Department of General is associated with food-B12 guanide use. It also requires that you Practice, Cardiff University, malabsorption more often than consider not only a patient’s serum B12 United Kingdom with pernicious anemia. (C) ® Dowdenlevels, but his Health homocysteine Media and meth - Noureddine Henoun ylmalonic acid levels, since they are con- Loukili, PhD • The classic treatment for B 12 Department of Hygiene and deficiency—particularly when the sidered more sensitive indicators of co- 6 Fight against Nosocomial cause is not a dietaryCopyright deficiency—isFor personalbalamin deficiency. use Keyingonly in on these Infections, Hôpital Calmette, 100 to 1000 mcg per month of indicators early will ensure prompt treat- CHRU de Lille, Lille, France cyanocobalamin, IM. (B) ment, which typically includes intramus- cular injections of the vitamin, but which Jacques Zimmer, MD, PhD • Oral crystalline cyanocobalamin could revolve around a more convenient Laboratoire is an effective treatment for food- d’Immunogénétique- option: oral B12. Allergologie, Centre de B12 malabsorption, though it’s Recherche Public de la Santé effectiveness in the long term has (CRP-Santé) de Luxembourg, not been demonstrated. -

Nutrition 102 – Class 3
Nutrition 102 – Class 3 Angel Woolever, RD, CD 1 Nutrition 102 “Introduction to Human Nutrition” second edition Edited by Michael J. Gibney, Susan A. Lanham-New, Aedin Cassidy, and Hester H. Vorster May be purchased online but is not required for the class. 2 Technical Difficulties Contact: Erin Deichman 574.753.1706 [email protected] 3 Questions You may raise your hand and type your question. All questions will be answered at the end of the webinar to save time. 4 Review from Last Week Vitamins E, K, and C What it is Source Function Requirement Absorption Deficiency Toxicity Non-essential compounds Bioflavonoids: Carnitine, Choline, Inositol, Taurine, and Ubiquinone Phytoceuticals 5 Priorities for Today’s Session B Vitamins What they are Source Function Requirement Absorption Deficiency Toxicity 6 7 What Is Vitamin B1 First B Vitamin to be discovered 8 Vitamin B1 Sources Pork – rich source Potatoes Whole-grain cereals Meat Fish 9 Functions of Vitamin B1 Converts carbohydrates into glucose for energy metabolism Strengthens immune system Improves body’s ability to withstand stressful conditions 10 Thiamine Requirements Groups: RDA (mg/day): Infants 0.4 Children 0.7-1.2 Males 1.5 Females 1 Pregnancy 2 Lactation 2 11 Thiamine Absorption Absorbed in the duodenum and proximal jejunum Alcoholics are especially susceptible to thiamine deficiency Excreted in urine, diuresis, and sweat Little storage of thiamine in the body 12 Barriers to Thiamine Absorption Lost into cooking water Unstable to light Exposure to sunlight Destroyed -

Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Vitamin B12 Vitamin D Iodine and Selenium
Frequently Asked Questions for VEG 1 General 1. Why has VEG 1 been developed? VEG 1 was developed to provide a convenient way of avoiding the most common weak points in a varied vegan diet: vitamin B12, iodine, vitamin D and selenium. Vitamin B12 Vitamin B12 is almost entirely absent from modern plant foods which are not contaminated by bacteria and insects. Even unwashed, organically grown plants do not contain a significant amount of B12. Vegans often have intakes of vitamin B12 well below recommended intakes. Low vitamin B12 intake by vegans routinely leads to reduced activity of some important enzymes and increased levels of homocysteine and methylmalonic acid (MMA). Even moderately elevated homocysteine is associated with increased risk of death, depression, stroke, dementia and birth defects, though it remains unclear how many of these associations reflect true cause and effect. Vegans who do not get vitamin B12 from fortified food or supplements are at increased risk of clinical deficiency symptoms such as anaemia and nervous system damage. The most common early symptoms of vitamin B12 deficiency are tiredness (from anaemia), numbness and tingling (from nervous system damage) and sore tongue. VEG 1 is designed to provide sufficient absorbed vitamin B12 to match national and international recommended intakes. It is designed to be chewed as this increases the reliability of vitamin B12 absorption by dispersing and dissolving the tablet. Vitamin D In the winter – whenever our shadows at midday are more than twice as long as we are – our skin cannot produce vitamin D effectively and even small dietary intakes may become important to avoid deficiency. -

Effects of Vitamin D Deficiency on the Improvement of Metabolic Disorders
www.nature.com/scientificreports OPEN Efects of vitamin D defciency on the improvement of metabolic disorders in obese mice after vertical sleeve gastrectomy Jie Zhang1,2,7, Min Feng3,7, Lisha Pan4,7, Feng Wang1,3, Pengfei Wu4, Yang You4, Meiyun Hua4, Tianci Zhang4, Zheng Wang5, Liang Zong6*, Yuanping Han4* & Wenxian Guan1,3* Vertical sleeve gastrectomy (VSG) is one of the most commonly performed clinical bariatric surgeries for the remission of obesity and diabetes. Its efects include weight loss, improved insulin resistance, and the improvement of hepatic steatosis. Epidemiologic studies demonstrated that vitamin D defciency (VDD) is associated with many diseases, including obesity. To explore the role of vitamin D in metabolic disorders for patients with obesity after VSG. We established a murine model of diet- induced obesity + VDD, and we performed VSGs to investigate VDD’s efects on the improvement of metabolic disorders present in post-VSG obese mice. We observed that in HFD mice, the concentration of VitD3 is four fold of HFD + VDD one. In the post-VSG obese mice, VDD attenuated the improvements of hepatic steatosis, insulin resistance, intestinal infammation and permeability, the maintenance of weight loss, the reduction of fat loss, and the restoration of intestinal fora that were weakened. Our results suggest that in post-VSG obese mice, maintaining a normal level of vitamin D plays an important role in maintaining the improvement of metabolic disorders. Obesity and its related comorbidities afect 2.1 billion people worldwide1. In last decade, bariatric surgery has emerged as an efective treatment for obese individuals because of its sustained ability to reduce body weight 2–4. -
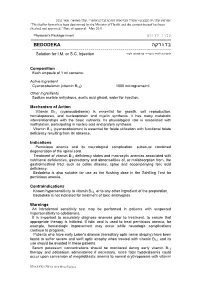
בדודקה BEDODEKA ------להזרקה לתוך השריר או מתחת לעור Solution for I.M
"פורמט עלון זה נקבע ע"י משרד הבריאות ותוכנו נבדק ואושר". עלון מאושר: מאי 2011. “This leaflet format has been determined by the Ministry of Health and the content thereof has been checked and approved.” Date of approval: May 2011. עלון לרופא Physician's Package Insert ========================================================================== בדודקה BEDODEKA --------------------------------------------------------------------- להזרקה לתוך השריר או מתחת לעור Solution for I.M. or S.C. Injection Composition Each ampoule of 1 ml contains: Active Ingredient Cyanocobalamin (vitamin B12) 1000 micrograms/ml Other Ingredients Sodium acetate anhydrous, acetic acid glacial, water for injection. Mechanism of Action Vitamin B12 (cyanocobalamin) is essential for growth, cell reproduction, hematopoiesis, and nucleoprotein and myelin synthesis. It has many metabolic interrelationships with the basic nutrients. Its physiological role is associated with methylation, participating in nucleic acid and protein synthesis. Vitamin B12 (cyanocobalamin) is essential for folate utilization with functional folate deficiency resulting from its absence. Indications Pernicious anemia and its neurological complication, subacute combined degeneration of the spinal cord. Treatment of vitamin B12 deficiency states and macrocytic anemias associated with nutritional deficiencies, gastrectomy and abnormalities of, or malabsorption from, the gastrointestinal tract such as celiac disease, sprue and accompanying folic acid deficiency. Bedodeka is also suitable for use as the flushing dose in the Schilling Test for pernicious anemia. Contraindications Known hypersensitivity to vitamin B12, or to any other ingredient of the preparation. Bedodeka is not indicated for treatment of toxic amblyopias. Warnings An intradermal sensitivity test may be performed in patients with suspected hypersensitivity to cobalamins. It is important to accurately diagnose anemias prior to treatment, to ensure that appropriate therapy is initiated. -

These Highlights Do Not Include All the Information Needed to Use M.V.I. Pediatric® Safely and Effectively
M.V.I. PEDIATRIC- ascorbic acid, retinol, ergocalciferol, thiamine hydrochloride, riboflavin 5- phosphate sodium, pyridoxine hydrochloride, niacinamide, dexpanthenol, .alpha.-tocopherol acetate, dl-, biotin, folic acid, cyanocobalamin, and phytonadione injection, powder, lyophilized, for solution Hospira, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use M.V.I. Pediatric® safely and effectively. See full prescribing information for M.V.I. Pediatric. M.V.I. Pediatric (multiple vitamins for injection), for intravenous use Initial U.S. Approval: 1983 RECENT MAJOR CHANGES Dosage And Administration, Dosage Information (2.2) 2/2019 INDICATIONS AND USAGE M.V.I. Pediatric is a combination of vitamins indicated for the prevention of vitamin deficiency in pediatric patients up to 11 years of age receiving parenteral nutrition (1) DOSAGE AND ADMINISTRATION M.V.I. Pediatric is a combination product that contains the following vitamins: ascorbic acid, vitamin A, vitamin D, thiamine, riboflavin, pyridoxine, niacinamide, dexpanthenol, vitamin E, vitamin K, folic acid, biotin, and vitamin B12 (2.1) Supplied as a single-dose vial of lyophilized powder for reconstitution intended for administration by intravenous infusion after dilution. (2.1) Recommended daily dosage is based on patient's actual weight (2.2) Less than 1 kg: The daily dose is 1.5 mL 1 kg to 3 kg: The daily dose is 3.25 mL 3 kg or more: The daily dose is 5 mL One daily dose of the reconstituted solution (1.5 mL, 3.25 mL or 5 mL) is then added directly to the intravenous fluid (2.2,2.3) See Full Prescribing Information for reconstitution instructions (2.3) Monitor blood vitamin concentrations (2.4) See Full Prescribing Information for drug incompatibilities (2.5) DOSAGE FORMS AND STRENGTHS M.V.I. -

A Clinical Update on Vitamin D Deficiency and Secondary
References 1. Mehrotra R, Kermah D, Budoff M, et al. Hypovitaminosis D in chronic 17. Ennis JL, Worcester EM, Coe FL, Sprague SM. Current recommended 32. Thimachai P, Supasyndh O, Chaiprasert A, Satirapoj B. Efficacy of High 38. Kramer H, Berns JS, Choi MJ, et al. 25-Hydroxyvitamin D testing and kidney disease. Clin J Am Soc Nephrol. 2008;3:1144-1151. 25-hydroxyvitamin D targets for chronic kidney disease management vs. Conventional Ergocalciferol Dose for Increasing 25-Hydroxyvitamin supplementation in CKD: an NKF-KDOQI controversies report. Am J may be too low. J Nephrol. 2016;29:63-70. D and Suppressing Parathyroid Hormone Levels in Stage III-IV CKD Kidney Dis. 2014;64:499-509. 2. Hollick MF. Vitamin D: importance in the prevention of cancers, type 1 with Vitamin D Deficiency/Insufficiency: A Randomized Controlled Trial. diabetes, heart disease, and osteoporosis. Am J Clin Nutr 18. OPKO. OPKO diagnostics point-of-care system. Available at: http:// J Med Assoc Thai. 2015;98:643-648. 39. Jetter A, Egli A, Dawson-Hughes B, et al. Pharmacokinetics of oral 2004;79:362-371. www.opko.com/products/point-of-care-diagnostics/. Accessed vitamin D(3) and calcifediol. Bone. 2014;59:14-19. September 2 2015. 33. Kovesdy CP, Lu JL, Malakauskas SM, et al. Paricalcitol versus 3. Giovannucci E, Liu Y, Rimm EB, et al. Prospective study of predictors ergocalciferol for secondary hyperparathyroidism in CKD stages 3 and 40. Petkovich M, Melnick J, White J, et al. Modified-release oral calcifediol of vitamin D status and cancer incidence and mortality in men. -

VITAMIN DEFICIENCIES in RELATION to the EYE* by MEKKI EL SHEIKH Sudan VITAMINS Are Essential Constituents Present in Minute Amounts in Natural Foods
Br J Ophthalmol: first published as 10.1136/bjo.44.7.406 on 1 July 1960. Downloaded from Brit. J. Ophthal. (1960) 44, 406. VITAMIN DEFICIENCIES IN RELATION TO THE EYE* BY MEKKI EL SHEIKH Sudan VITAMINS are essential constituents present in minute amounts in natural foods. If these constituents are removed or deficient such foods are unable to support nutrition and symptoms of deficiency or actual disease develop. Although vitamins are unconnected with energy and protein supplies, yet they are necessary for complete normal metabolism. They are, however, not invariably present in the diet under all circumstances. Childhood and periods of growth, heavy work, childbirth, and lactation all demand the supply of more vitamins, and under these conditions signs of deficiency may be present, although the average intake is not altered. The criteria for the fairly accurate diagnosis of vitamin deficiencies are evidence of deficiency, presence of signs and symptoms, and improvement on supplying the deficient vitamin. It is easy to discover signs and symptoms of vitamin deficiencies, but it is not easy to tell that this or that vitamin is actually deficient in the diet of a certain individual, unless one is able to assess the exact daily intake of food, a process which is neither simple nor practical. Another way of approach is the assessment of the vitamin content in the blood or the measurement of the course of dark adaptation which demon- strates a real deficiency of vitamin A (Adler, 1953). Both tests entail more or less tedious laboratory work which is not easy in a provincial hospital. -

VI.2 Elements for a Public Summary VI.2.1 Overview of Disease Epidemiology Vitamin B12 Deficiency Can Have a Number of Possible
VI.2 Elements for a public summary VI.2.1 Overview of disease epidemiology Vitamin B12 deficiency can have a number of possible causes. Typically it occurs in people whose digestive systems do not adequately absorb the vitamin from the foods they eat. This can be caused by: Pernicious anemia, a condition in where there is a lack of a protein called intrinsic factor. The protein, which is made in the stomach, is necessary for vitamin B12 absorption. Other causes can be gastritis, surgery in which part of the stomach and/or small intestine is removed or conditions affecting the small intestine. Vitamin B12 deficiency can also occur in pregnancy and with long- term use of acid-reducing drugs. VI.2.2 Summary of treatment benefits A deficiency of vitamin B12 (cobalamin) is manifested by fatigue, weakness, mood fluctuations, memory loss, limb weakness, difficulty walking, tingling, and paralysis. Drug treatment involves the administration of vitamin B12 by injection. If the deficiency of vitamin B12 (cobalamin) depends on the underlying disease being resolved, the vitamin supplementation continues until normal levels of vitamin B12 are achieved. If the deficiency state cannot be resolved (e.g. inadequate secretion of intrinsic factor, genetic abnormalities related to the site absorption, etc.) therapy should be continued for life. VI.2.3 Unknowns relating to treatment benefits None. VI.2.4 Summary of safety concerns Risk What is known Preventability Damage to the optic nerve Optic nerve atrophy/blindness The product should be used (atrophy)/blindness in is a risk associated with with caution. patients with Leber´s disease treatment with (a disease that affects the hydroxocobalamin in patients optic nerve and often causes with Leber´s disease. -

Niacin (Nicotinic Acid) in Non-Physiological Doses Causes Hyperhomocysteineaemia in Sprague–Dawley Rats
Downloaded from British Journal of Nutrition (2002), 87, 115–119 DOI: 10.1079/BJN2001486 q The Authors 2002 https://www.cambridge.org/core Niacin (nicotinic acid) in non-physiological doses causes hyperhomocysteineaemia in Sprague–Dawley rats Tapan K. Basu*, Neelam Makhani and Gary Sedgwick . IP address: Department of Agricultural, Food and Nutritional Science, University of Alberta, Edmonton, Alberta, T6G 2P5 Canada (Received 22 September 2000 – Revised 17 July 2001 – Accepted 6 August 2001) 170.106.35.93 Niacin (nicotinic acid) in its non-physiological dose level is known to be an effective lipid- , on lowering agent; its potential risk as a therapeutic agent, however, has not been critically 27 Sep 2021 at 22:43:08 considered. Since niacin is excreted predominantly as methylated pyridones, requiring methionine as a methyl donor, the present study was undertaken to examine whether metabolism of the amino acid is altered in the presence of large doses of niacin. Male Sprague–Dawley rats were given a nutritionally adequate, semi-synthetic diet containing niacin at a level of either 400 or 1000 mg/kg diet (compared to 30 mg/kg in the control diet) for up to 3 months. Supplementation with niacin (1000 mg/kg diet) for 3 months resulted in a significant increase in plasma and urinary total homocysteine levels; this increase was further accentuated in the , subject to the Cambridge Core terms of use, available at presence of a high methionine diet. The hyperhomocysteineaemia was accompanied by a significant decrease in plasma concentrations of vitamins B6 and B12, which are cofactors for the metabolism of homocysteine.