Dublin North East Regional Service Plan 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Educational Prospectus for Dublin South, Kildare and Wicklow January – April 2020
Educational Prospectus for Dublin South, Kildare and Wicklow January – April 2020 Educational programmes within Tallaght University Hospital, St James’s Hospital and St Vincent’s University Hospital @RegionalEdDSK Regina Lennon – Regional Education Co-ordinator for South Dublin, Kildare and Wicklow Registered Nurse Tutor, Registered Public Health Nurse and Registered General Nurse Centre for Learning and Development St James’s Hospital Dublin 8 014284896 [email protected] Follow me on Twitter @Lennonr4 Biography Having studied Bachelor of Science and Nursing (Honours) General Nursing at the Dublin City University, in conjunction with Connolly hospital, Regina worked in Connolly hospital as a Register General Nurse after receiving her qualification. Moving to Australia, she worked within acute hospitals in both Melbourne and Darwin. On return to Dublin, Regina did agency work in a number of acute hospitals. Subsequently she was offered a position as a community nursing at North West Dublin. This led her to being selected for sponsorship and completing her Higher Diploma in Public Health Nursing at the University College Dublin. As a Public Health Nurse Regina’s caseload was based in inner city Dublin; this caseload involved working within child protection and welfare, advocating for children within the court system and supporting individuals/families in the homelessness crisis. Following an assessment of population need, Regina supported the establishment of the Incredible Years Programme in inner city Dublin. In 2017, Regina completed a First Class Masters in Nursing Education at the University College Dublin. Regina was appointed Regional Education Co-ordinator within CLD in St James’s hospital and her role involves co-ordinating education for community staff working in South Dublin, Kildare and Wicklow including Public Health, Older persons, Mental Health and Intellectual Disability services. -

Independent Monitoring Group
Independent Monitoring Group A Vision for Change – the Report of the Expert Group on Mental Health Policy Sixth Annual Report on implementation 2011 June 2012 Contents Page Executive Summary Glossary of Abbreviations 1. The Work of the Independent Monitoring Group 5 2. Progress on Implementation as reported by the Health Service Executive 10 National 10 Regional 21 3. Commentary on progress reported by Health Service Executive 42 4. Progress on Implementation as reported by Government Departments 55 5. Commentary on progress reported by Government Departments 71 6. Addressing the biological, psychological and social factors that contribute to mental health problems 74 7. The National Mental Health Programme Plan (Clinical Programmes) 78 8. Recovery 84 9. Overview of progress on implementation since 2006 91 10. Consultation process – comparisons between 2004 and 2012 100 11. Monitoring of Implementation 101 12. Recommendations 103 Appendices Glossary of Abbreviations ASIST Applied Suicide Intervention Skills Training AVFC A Vision for Change CAMHS Child and Adolescent Mental Health Services CAMHT Child and Adolescent Mental Health Team CAWT Co-operation and Working Together CBT Cognitive Behavioural Therapy CEO Chief Executive Officer CMHTs Community Mental Health Teams CPI The College of Psychiatry of Ireland CSPD HSE’s Clinical Strategy and Programme Directorate DCU Dublin City University DBT Dialectical Behavioural Therapy ECDs Executive Clinical Directors E&T Education and Training HRB Health Research Board HSE Health Service Executive IMG Independent Monitoring Group MHC Mental Health Commission NCL National Clinical Lead for Mental Health NCHDs Non-Consultant Hospital Doctors NOSP National Office for Suicide Prevention NSUE National Service Users Executive PPM Programme Project Manager RDOs Regional Directors of Operations SCAN Suicide Crisis Assessment Nurse WTE Whole Time Equivalent Executive Summary This is the 6 th Annual Report of the Independent Monitoring Group for A Vision for Change (IMG) and the final report of the Second Group. -

Noca Quality Improvement Champion Award 2021
NOCA QUALITY IMPROVEMENT CHAMPION AWARD 2021 The NOCA ‘Quality Improvement Champion Award’ recognises an individual or team who has made best use of national or local clinical audit data to improve patient care in their hospital/hospital group/healthcare organisation. Contents ENTRIES ......................................................................................................................... 3 RECIPIENTS OF THE CHAMPION AWARDS ................................................................... 6 ENTRY 1 - WINNER ............................................................................................................... 8 ENTRY 2 ............................................................................................................................ 11 ENTRY 3 ............................................................................................................................ 16 ENTRY 4 ............................................................................................................................ 22 ENTRY 5 ............................................................................................................................ 25 ENTRY 6 ............................................................................................................................. 27 ENTRY 7 – HIGHLY COMMENDED .................................................................................. 30 ENTRY 8 – HIGHLY COMMENDED .................................................................................. 33 ENTRY 9 ............................................................................................................................ -

Better Services for Patients Time 4 Us
Health Matters Vol. 4 Issue 1 Spring 2008 Item Type Report Authors Health Service Executive (HSE) Rights Health Service Executive Ireland Download date 30/09/2021 21:58:05 Link to Item http://hdl.handle.net/10147/45763 Find this and similar works at - http://www.lenus.ie/hse New Hygiene Vaccine Delivery HfH Premiers in Campaign Success Crumlin Patients to question staff New system saves money and Our Lady’s Hospital, Crumlin on hand washing improves safety launches HfH Programme p9 p15 p18 KdajbZ ) >hhjZ& Heg^c\ '%%- =ZVai]NationalbViiZgh Staff Newsletter of the Health Service Executive Integrated System Can Deliver Better Services for Patients Time 4 Us Parents in Galway enjoy more recent review of how public With this approach, health services > Increases in the number of day inpatients could be treated in an quality time with children hospitals admit, treat and (within and between hospital and cases (the average in Ireland is 12 alternative to an acute hospital). p 24 A discharge patients has found community) are connected together per cent below the OECD average); The review highlights that these that patients would spend less time in seamlessly, delays between services > More discharge planning (currently practices are already working well hospital, and receive a better service, if are reduced and patients receive a no discharge date is planned for 83 in a number of Irish hospitals and all public hospitals adopted practices better service. per cent of patients); introducing them to all public hospitals that are the norm in other advanced The review recommends: > Bringing patients into hospital on the could be done relatively quickly. -
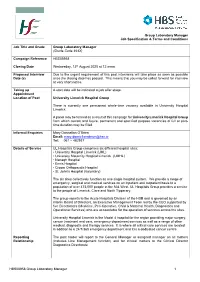
HBS08958 Group Laboratory Manager 1 Group Laboratory Manager Job Specification & Terms and Conditions Job Title and Grade Gr
Group Laboratory Manager Job Specification & Terms and Conditions Job Title and Grade Group Laboratory Manager (Grade Code 393X) Campaign Reference HBS08958 Closing Date Wednesday, 12th August 2020 at 12 noon Proposed Interview Due to the urgent requirement of this post interviews will take place as soon as possible Date (s) once the closing date has passed. This means that you may be called forward for interview at very short notice. Taking up A start date will be indicated at job offer stage. Appointment Location of Post University Limerick Hospital Group There is currently one permanent whole-time vacancy available in University Hospital Limerick. A panel may be formed as a result of this campaign for University Limerick Hospital Group from which current and future, permanent and specified purpose vacancies of full or part- time duration may be filled. Informal Enquiries Mary Donnellan O’Brien Email: [email protected] Tel: 061 – 482937 Details of Service UL Hospitals Group comprises six different hospital sites: • University Hospital Limerick (UHL) • University Maternity Hospital Limerick (UMHL) • Nenagh Hospital • Ennis Hospital • Croom Orthopaedic Hospital • St. John’s Hospital (Voluntary) The six sites collectively function as one single hospital system. We provide a range of emergency, surgical and medical services on an inpatient and outpatient basis to a population of over 473,000 people in the Mid-West. UL Hospitals Group provides a service to the people of Limerick, Clare and North Tipperary. The group reports to the Acute Hospitals Division of the HSE and is governed by an interim Board of Directors, an Executive Management Team led by the CEO supported by five Directorates (Medicine, Peri-Operative, Child & Maternal Health, Diagnostics and Operational Services) who are accountable for the operation of services across the sites. -

The Ombudsman and Public Hospitals
The Ombudsman and the Public Hospitals The Ombudsman is Impartial Independent A free service 2 Who is the Ombudsman and what does the Ombudsman do? Peter Tyndall is the Ombudsman. The Ombudsman can examine complaints about the actions of a range of public bodies, including public hospitals. All hospitals providing public health services come within the Ombudsman’s remit. The Ombudsman can examine complaints about how hospital staff carry out their everyday administrative activities when providing public health services. These include complaints about delays or failing to take action. However, there are certain complaints that the Ombudsman cannot examine. These include complaints about: private health care regardless of where it is provided and clinical judgment by the HSE (diagnoses or decisions about treatment Is the Ombudsman independent? Yes. The Ombudsman is independent and impartial when examining complaints. 1 What can I complain to the Ombudsman about? You can complain about your experience in dealing with a hospital. This might include, among other issues, a hospital: applying an incorrect charge failing to follow approved administrative procedures, protocols or reasonable rules failing to communicate clearly failing to seek your informed consent to a procedure keeping poor records failing to respect your privacy and dignity having staff who are rude or unhelpful or who discriminate against you being reluctant to correct an error failing to deal with your complaint in accordance with the complaints process. 2 Which -

Annual Report 2020
Mental Health Commission Annual Report 2020 Including the Report of the Inspector of Mental Health Services MORE INFORMATION www.mhcirl.ie www.linkedin.com/company/mentalhealthcommissionirl www.twitter.com/mhcireland Mental Health Commission Annual Report 2020 Contents Chairperson’s Statement 2 Chief Executive’s Review 4 2020 in Brief 6 Who We Are 7 • Vision, Mission and Values 9 • Strategic Objectives 2019-2022 10 • Mental Health Commission Members (April 2017 – April 2022) 11 • Senior Leadership Team 14 What We Do 15 • Regulatory Process 16 • Quality Improvement 31 • Mental Health Tribunals 36 • Decision Support Service 50 Governance 54 Appendices 61 Report of the Inspector of the Mental Health Services 67 1 Chairperson’s Statement In 2020, in the context of COVID-19, the MHC remained John Saunders focused on our mission ‘to regulate and engage to Chairperson promote, support, and uphold the rights, health and wellbeing of all people who access mental health and decision support services’. The MHC welcomes the determination and resolve of the Minister for Mental Health and Older People, Mary Butler TD, to progress new and reforming legislation. The MHC was invited to comment on the draft Heads of Bill to amend the Mental Health Act, 2001. We established a working group, which was chaired by our General Counsel and included the Inspector of Mental Health Services and the MHC’s Director of Regulation. This group worked with the Commission’s Legislation Committee to provide a detailed, evidenced-based, person-centred, and rights-based submission to the Department of Health. A synopsis of our recommendations can be found in the appendices to this report (page 64). -

The Hospice Friendly Hospitals Programme
The Hospice Friendly Hospitals Programme Overview 2007-2013 Foreword This report describes how care for people who die in Irish hospitals is planned and provided for; and how those processes evolved over the period 2007-2013. The report details a journey and we do not claim to have reached journey’s end. The ‘Hospice Friendly Hospitals’ (HFH) programme, as an aspiration or an idea, meets with very little resistance. Its aim - to transform the culture of hospital care for dying patients is a shared and transparent aim which we believe has now made its way into Irish discourse. While the aim may be agreeable, the means for change are not so straightforward. Culture change is not simple; the very founding premis being that those who are a part of and members of a particular culture are often the last to see what is good, and what is not so good about a system. Rather people carry on doing these good things and not so good things as they represent ‘the way things are done around here’. Culture is a powerful maintenance mechanism precisely because of its shared and unquestioned beliefs and values. THE HOSPICE FRIENDLY HOSPITALS PROGRAMME HOSPITALS THE HOSPICE FRIENDLY HFH set out to introduce newer ways of doing things, to (re)introduce core values, to question and unsettle some of the assumptions and to provide support, tools and forums. As an example, in her introduction to the HFH standards President Mary McALeese gave us a vision of a ‘care-full death’. We believe a narrative approach is crucial to communicate and record some of the complexity of this type of programme. -

Appendix D. Useful Contact Information
Consultants in Infectious Diseases/ Genitourinary Medicine (cont’d) Dr Eoin Feeney St Vincent’s University Hospital, Elm Park, Dublin 4 Tel: 01 221 4000 Dr Justin Low, Louth County Hospital, Dundalk Tel: 086 8241847 Paediatric Infectious Diseases Professor Karina Butler Our Lady’s Children’s Hospital Crumlin Dublin 12 Tel: 01 4096100 Dr Paddy Gavin Children’s University Hospital Temple Street Dublin 1 Tel: 01 8784200 Infectious Disease Assessment for Migrants 2015 Appendix D. Useful contact information Consultants in Infectious Diseases/ Paediatric Infectious Diseases Genitourinary Medicine Professor Karina Butler Dr Busi Mooka Our Lady’s Children’s Hospital Mid West Regional Hospital Crumlin Limerick Dublin 12 Tel: 061 301111 Tel: 01 4096100 Dr Catherine Fleming Dr Paddy Gavin Dr Helen Tuite Children’s University Hospital University College Hospital Temple Street Galway Dublin 1 Tel: 091 544544 Tel: 01 8784200 Professor Mary Horgan, Dr Arthur Jackson Sexually Transmitted Infection/ Cork University Hospital Genitourinary Medicine Clinics Co Cork Youth Health Service, Tel: 021 454 6400 73 Shandon Street, Cork City Dr Susie Clarke, Tel: 021-4220490/1 Dr Fiona Lyons, Professor Colm Bergin, Gay Men’s Health Service, Professor Fiona Mulcahy Baggot Street Clinic, St James’s Hospital GUIDE Dept 19 Haddington Road, James’s St Dublin 4 Dublin 8 Tel: 01 6699553 Tel: 01 4162315, 01 4162316 St James’s Hospital, Dr Jack Lambert, GUIDE Clinic, Dr Paddy Mallon, James’s Street, Dr Gerard Sheehan Dublin 8 Mater Misericordiae University Hospital, Tel: -

THE NATIONAL PATIENT TREATMENT REGISTER APRIL 2010 Table of Contents
A report on the national patient treatment registar Item Type Report Authors National Purchases Treatment Fund Publisher National Purchases Treatment Fund Download date 26/09/2021 22:55:13 Link to Item http://hdl.handle.net/10147/234087 Find this and similar works at - http://www.lenus.ie/hse A REPORT ON THE NATIONAL PATIENT TREATMENT REGISTER APRIL 2010 Table of Contents Summary of Hospitals 1 Statistical Summary 2 Trend Analysis 3 – 10 Median Wait Time in months for Adult Surgical Procedures 11 – 12 Median Wait Time in months for Child Surgical Procedures 13 Hospital Statistical Bibliography 14 – 29 Review and Analysis Program 30 – 31 Glossary 32 Acknowledgements 33 The hospitals illustrated are as follows – SUMMARY - DUBLIN NORTH/NORTH EAST HSE AREA SOUTHERN/SOUTH EAST HSE AREA The Patient • Beaumont Hospital Dublin • Bantry General Hospital • Cappagh Orthopaedic Hospital • Cork University Hospital Treatment Register • Cavan General Hospital** • Lourdes Orthopaedic Hospital, Kilcreene** • Connolly Hospital, Blanchardstown • Kerry General Hospital • Louth County Hospital** • Mallow General Hospital • Monaghan General Hospital** • Mercy University Hospital, Cork The Patient Treatment Register (PTR) is • Our Lady of Lourdes Hospital, Drogheda** • South Infirmary Victoria University Hospital Cork an online register of patients on in-patient • Our Lady’s Hospital, Navan** • South Tipperary General Hospital** and day-case surgical and medical waiting • The Childrens University Hospital Temple Street** • St. Luke’s Hospital, Kilkenny** • Mater Hospital, Dublin • Waterford Regional Hospital** lists in Ireland. Wait time information is • Wexford Hospital** published monthly to the PTR website www.ptr.ie on 44 hospitals nationally. Patients and General Practitioners can DUBLIN EAST COAST, DUBLIN SOUTH WEST/ access up to date information on wait NORTH WEST/WEST/MID-WEST HSE AREA MIDLANDS HSE AREA times for individual procedures for 44 • Letterkenny General Hospital • Midland Regional Hospital at Mullingar • Mayo General Hospital hospitals. -

Performance Profile
Performance Profile October - December 2017 Quarterly Report Contents Corporate Updates .................................................................................................................................................. 3 Quality and Patient Safety ..................................................................................................................................... 10 Performance Overview .......................................................................................................................................... 13 Health and Wellbeing ......................................................................................................................................... 14 Primary Care ...................................................................................................................................................... 21 Mental Health ..................................................................................................................................................... 29 Social Care ......................................................................................................................................................... 34 Social Care - Disabilities .................................................................................................................................... 36 Social Care – Older Persons ............................................................................................................................. 42 National Ambulance -

List of Approved Hospitals, Scan Centres & Treatment Centres
Cover For Me Cover For Us Cover For All Of Us Cover For Me Cover For Us Cover For All Of Us Hospital Maternity Out-Patient Activate Hospital & Core Plan Ranges Hospital Maternity Out-Patient Cover For Me Cover For Us Cover For All Of Us List Of Approved Hospitals, International Health & Travel Scan CentresSports Cover & Out-Patient Scan Treatment Centres September 2015 International Health & Travel Sports Cover Out-Patient Scan Hospital Maternity Out-Patient Women’s & Men's Health Complementary Therapy Dental & Optical Women’s & Men's Health Complementary Therapy Dental & Optical International Health & Travel Sports Cover Out-Patient Scan Women’s & Men's Health Complementary Therapy Dental & Optical 01 List Of Approved Hospitals Name of Hospital Type Cavan Cavan General Hospital Public Cover For Me Cover For Us Cover For All Of Us Clare Bushypark Treatment Centre, Ennis Addiction Centre Mid Western Regional Hospital, Ennis Public Cork Bantry General Hospital Public Bon Secours Hospital Private Cork University Hospital Public Hospital Maternity Out-Patient Cork University Maternity Hospital Public Cuan Mhuire, Farnanes Addiction Centre Mallow General Hospital Public Mater Private Cork Private Mercy University Hospital Public South Infirmary Victoria University Hospital Public St Mary’s Orthopaedic Hospital Public Tabor Lodge, Belgooly Addiction Centre International Health & Travel Sports Cover Out-Patient Scan Donegal Letterkenny General Hospital Public White Oaks Treatment Centre Addiction Centre Dublin Beacon Cancer Centre Private Beacon Hospital, Dublin 18 - Cardiac Procedures - All Plans High Tech - Private Beacon Hospital, Dublin 18 - All other procedures Private* Women’s & Men's Health Complementary Therapy Dental & Optical Beacon Hospital, Dublin 18 - Basic & Good Plans High Tech - Private * Beacon Hospital is classified as a private hospital (excluding cardiac procedures) for all plans in the Activate Hospital & Core plan ranges apart from Basic plan, Good plan & Activate Hospital plan.