An Echo to Choosing Wisely® in Switzerland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Switzerland in the 19Th Century
Switzerland in the 19th century The founding of the Swiss federal state ushered in a period of greater stability as regards both domestic and foreign affairs. The revised Constitution of 1874 extended the powers of the federal government and introduced the optional legislative referendum. Switzerland developed its system of direct democracy further and in 1891 granted the people the right of initiative on the partial revision of the Federal Constitution. That same year the Catholic conservatives – the losers of the Sonderbund war – celebrated, for the first time, the election of one of its representatives to the federal government. The federal state used its new powers to create favourable conditions for the development of a number of industries and service sectors (railways, machine construction and metalworking, chemicals, food industry and banking). These would become the mainstays of the Swiss economy. Not everyone in Switzerland reaped the benefits of the economic upturn. In the 19th century poverty, hunger and a lack of job prospects drove many Swiss people to seek their fortunes elsewhere, particularly in North and South America. At home, industrial towns and cities saw an influx of rural and, increasingly, foreign migrants. Living conditions for many members of this new urban working class were often precarious. Foreign policy During the wave of revolution that engulfed Europe in the early 1850s, relations between Switzerland and Austria, which also ruled northern Italy, were extremely tense. Many Italians, who wanted to see a united and independent Italy (Risorgimento), sought refuge in liberal- run Ticino. The local community sympathised with their cause, some even fighting alongside their Italian comrades or smuggling weapons for them. -

Spitäler Uster Und Wetzikon Geben Fusionsvorhaben Auf
Uster/Wetzikon, 11.12.2020 Medienmitteilung Fusion abgesagt Spitäler Uster und Wetzikon geben Fusionsvorhaben auf Verschiedene Umfeld- und Rahmenbedingungen, unter denen die Fusion 2018 in Angriff genommen worden war, haben sich innert kurzer Zeit markant verändert. Die Fortsetzung des Vorhabens ist in- zwischen stark risikobehaftet. Die beiden Verwaltungsräte geben das Fusionsprojekt deshalb mit grossem Bedauern auf. Sie sehen im Scheitern aber auch Chancen: Der intensive Austausch im Fusi- onsprozess ermöglicht eine vertiefte Zusammenarbeit auch ohne Fusion. Die Abstimmung über die Fusion der beiden Häuser hätte am 17. Mai 2020 erfolgen sollen. Covid-19- bedingt musste der Termin verschoben werden. Ins Auge gefasst wurde der Septembertermin. Durch diese Verschiebung war eine Neubeurteilung der Bewertungen im Hinblick auf die Ausfertigung des Fu- sionsvertrags nötig geworden. Dabei wurde deutlich, dass die beiden Jahre 2018 und 2019 in der Bilanz des Spitals Uster Spuren hinterlassen haben, welche mit Blick auf die Bewertung keine Parität mehr er- warten liessen. Der Septembertermin musste fallengelassen werden. Die erforderliche Parität kann mittlerweile plausibel gemacht werden. Sie ist aber aufgrund der Entwicklungen im wirtschaftlichen, gesundheitspolitischen und gesellschaftlichen Umfeld derart mit Unwägbarkeiten belastet, dass der Ab- bruch des Fusionsprozesses weniger risikobehaftet ist als dessen Fortsetzung. Nebst dieser veränderten Risikobeurteilung spielen beim Entscheid, die Fusionspläne aufzugeben, wei- tere Faktoren eine Rolle. Eine Fusion hätte den tiefgreifenden Umbau von Prozessen, Infrastruktur und Organisation zur Folge (IT, Bauvorhaben, Führung, etc.). Das war bekannt. Aber in der aktuellen Situa- tion sind diese Aufgaben praktisch nicht zu stemmen. Zudem rückt die Spitalplanung 2023 rasch näher: Die Gesundheitsdirektion hat den Termin für die Einreichung der Bewerbungsunterlagen auf den 1. -

Internationaler Basler Cup Basel, 28
Internationaler Basler Cup Basel, 28. - 30.5.2021 Event 34 Men, 50m Freestyle Open 30.05.2021 - 15:18 Entry list Prelim YB 1 ALLEGRINI, Mael 01 Lausanne Natation 23.12 2 YEBOAH, Robin 03 Schwimmverein beider Basel 23.25 3 CASERTA, Giovanni 02 A.S.Dilett. Calabria Swim Race 23.67 4 THENU, Maxime 02 Etoiles 92 23.78 5 PASSAFARO, Davide 06 A.S.Dilett. Calabria Swim Race 24.32 6 VERSCHOOTEN, Leo 06 Schwimmverein Baar 24.44 7 DEROUET, Noah 03 Dauphins De St-Louis 24.85 8 GIGAN, Matheo 05 Angers Natation 25.05 9 TANNO, Gian-Andrin 03 Schwimmgemeinschaft Liechtenstein 25.11 10 POIREL, Baptiste 02 Asptt Nancy 25.21 11 HERBULOT, Remi 05 Angers Natation 25.24 12 BECKERS, Felix 01 Schwimmclub Uster Wallisellen 25.39 13 MAIER, Reto 04 Schwimmclub Schaffhausen 25.50 14 FORMUZAL, Egor 04 TV Wetzlar 25.50 15 MEZULAT, Jodokus 01 Schwimmclub Schaffhausen 25.52 16 BARABAS, Andras 03 As. Club Sportiv "CIPRIAN" Sfantu Gheorghe 25.55 17 SCHMIEDEFELD, Richard 05 SV Cannstatt 1898 25.60 18 VESTER, Ben 05 SV Cannstatt 1898 25.70 19 PFENNINGER, Noe 03 Schwimmclub Uster Wallisellen 25.70 20 LEVET, Reef 03 Schwimmklub Bern 25.72 21 MUEHLETHALER, Lucas 02 Swim Team Biel-Bienne 25.74 22 GOEPPERT, Len 02 Schwimmclub Bottmingen-Oberwil 25.76 23 WIDMER, Romain 04 Schwimmclub Uster Wallisellen 25.81 24 ANSEL, Amedee 05 C.N Du Florival 25.83 25 BOUHAMOUCHE, Skander 04 CN La Chaux-de-Fonds 25.84 26 VEUVE, Cedric 03 Schwimmklub Bern 25.95 27 SCHMID, Ian 04 Limmat Sharks Zuerich 1 26.00 28 ROEMER, Niklas 05 TV Wetzlar 26.00 29 WINKELMANN, Xavier 05 Swim Team Biel-Bienne -

Clienia Psychiatriezentren Wetzikon Und Uster Ambulatorien Für Psychiatrie Und Psychotherapie 2 Herzlich Willkommen in Unseren Psychiatriezentren Wetzikon Und Uster
Clienia Psychiatriezentren Wetzikon und Uster Ambulatorien für Psychiatrie und Psychotherapie 2 Herzlich willkommen in unseren Psychiatriezentren Wetzikon und Uster Im Auftrag des Kantons Zürich führen wir Polikliniken mit Spezialsprechstunden, zwei Tageskliniken sowie den konsiliar- und liaisonpsychiatrischen Dienst für das GZO Spital Wetzikon, das Spital Uster und umliegende Heime. Die Clienia Psychiatriezentren Wetzikon (PZW) und Uster und Familien. Von Montag bis Freitag von 8 bis 18 Uhr (PZU) leisten an insgesamt vier Standorten nach den leisten wir den psychiatrischen Notfalldienst für die Region Grundsätzen des Zürcher Psychiatriekonzeptes wohnort- Zürcher Oberland. Wenn stationäre psychiatrische nahe, schnelle Hilfe in Zusammenarbeit mit Haus- und Behandlungen notwendig sind, arbeiten wir eng mit der Spezialärzten, Psychiatern und Psychotherapeuten, Clienia Privatklinik Schlössli in Oetwil am See zusammen. öffentlichen und privaten Diensten, Kliniken und Spitälern. Unsere Angebote decken das gesamte Spektrum der Unser Konsiliardienst bietet für die Spitäler GZO Wetzikon Erwachsenen- und Alterspsychiatrie ab. Wir bieten Ab- und Uster sowie die regionalen Alters- und Pflegeheime klärung, Beratung, Hilfestellung und Behandlung bei fachärztliche psychiatrische Diagnostik, Beurteilung, Thera - psychischen Krisen, Problemen und Erkrankungen aller pieempfehlung oder kurzfristige Mitbehandlung in Art wie zum Beispiel Deprimiertheit, Ängsten, Todes- enger Zusammenarbeit mit den Spital- bzw. Haus- und wünschen, Vergesslichkeit oder Wesensveränderungen. -

Interactions Between Rainbow Trout Eyed Eggs and Flavobacterium Spp
microorganisms Article Interactions between Rainbow Trout Eyed Eggs and Flavobacterium spp. Using a Bath Challenge Model: Preliminary Evaluation of Bacteriophages as Pathogen Control Agents Valentina L. Donati 1,*, Inger Dalsgaard 1, Anniina Runtuvuori-Salmela 2, Heidi Kunttu 2, Johanna Jørgensen 3, Daniel Castillo 3,† , Lotta-Riina Sundberg 2 , Mathias Middelboe 3 and Lone Madsen 1 1 Unit for Fish and Shellfish Diseases, National Institute of Aquatic Resources, Technical University of Denmark, 2800 Kongens Lyngby, Denmark; [email protected] (I.D.); [email protected] (L.M.) 2 Department of Biological and Environmental Science and Nanoscience Center, University of Jyväskylä, P.O. Box 35, FI-40014 Jyväskylä, Finland; anniina.runtuvuori@jyu.fi (A.R.-S.); heidi.kunttu@jyu.fi (H.K.); lotta-riina.sundberg@jyu.fi (L.-R.S.) 3 Marine Biological Section, Department of Biology, University of Copenhagen, 3000 Helsingør, Denmark; [email protected] (J.J.); [email protected] (D.C.); [email protected] (M.M.) * Correspondence: [email protected] † Present address: Instituto de Investigación Interdisciplinar en Ciencias Biomédicas SEK (I3CBSEK), Universidad SEK, Santiago 8340363, Chile. Citation: Donati, V.L.; Dalsgaard, I.; Runtuvuori-Salmela, A.; Kunttu, H.; Abstract: The microbial community surrounding fish eyed eggs can harbor pathogenic bacteria. Jørgensen, J.; Castillo, D.; Sundberg, In this study we focused on rainbow trout (Oncorhynchus mykiss) eyed eggs and the potential of L.-R.; Middelboe, M.; Madsen, L. bacteriophages against the pathogenic bacteria Flavobacterium psychrophilum and F. columnare. An Interactions between Rainbow Trout infection bath method was first established, and the effects of singular phages on fish eggs was Eyed Eggs and Flavobacterium spp. -

Internationaler Basler Cup Basel, 28
Internationaler Basler Cup Basel, 28. - 30.5.2021 Event 10 Men, 200m Freestyle Open 28.05.2021 - 15:52 Entry list Prelim YB 1 CASERTA, Giovanni 02 A.S.Dilett. Calabria Swim Race 1:50.30 2 CLAUDE, Killian 02 Sn Metz 1:56.89 3 TANNO, Gian-Andrin 03 Schwimmgemeinschaft Liechtenstein 1:57.29 4 ROEMER, Niklas 05 TV Wetzlar 1:57.50 5 KEMPF, Fabian 01 Schwimmclub Uster Wallisellen 1:57.73 6 MEZULAT, Jodokus 01 Schwimmclub Schaffhausen 1:58.19 7 PASSAFARO, Davide 06 A.S.Dilett. Calabria Swim Race 1:58.54 8 MAIER, Reto 04 Schwimmclub Schaffhausen 1:58.65 9 WRZESNIEWSKI, Moritz 05 TV Wetzlar 1:59.50 10 FORMUZAL, Egor 04 TV Wetzlar 2:00.00 11 PAPE, Colin 03 Club de natation Delemont 2:01.00 12 MCAVOY, Samuel 06 Limmat Sharks Zuerich 1 2:01.00 13 FUCHS, Kai 03 Schwimmclub Schaffhausen 2:01.00 14 GIGAN, Matheo 05 Angers Natation 2:01.23 15 VERSCHOOTEN, Leo 06 Schwimmverein Baar 2:01.33 16 HERBULOT, Remi 05 Angers Natation 2:01.45 17 TSCHIGG, Luis 04 Schwimmclub Schaffhausen 2:03.98 18 RETZLER, Noah 05 Limmat Sharks Zuerich 1 2:04.00 19 HOIGNE, Leonard 05 Schwimmklub Bern 2:04.68 20 PFENNINGER, Noe 03 Schwimmclub Uster Wallisellen 2:04.75 21 ZOLLINGER, Pascal 01 Swim Regio Solothurn 2:05.05 22 WIDMER, Romain 04 Schwimmclub Uster Wallisellen 2:05.10 23 KASSENBROCK, Maximilian 06 SG Schwimmen Muenster 2:05.19 24 AKCAY, Gueray 01 Schwimmverein beider Basel 2:05.49 25 MILLER, Jack 03 Schwimmclub Uster Wallisellen 2:05.77 26 SALONEN, Tommi 05 Schwimmklub Bern 2:05.84 27 KOCK, Kevin 07 SG Schwimmen Muenster 2:06.81 28 ROBERTUS, Valentin 03 Schwimmclub Schaffhausen -
Life Cycle Inventories of Bioenergy Data V2.0 (2007)
Swiss Centre for Life Cycle Inventories A joint initiative of the ETH domain and Swiss Federal Offices Life Cycle Inventories of Bioenergy Data v2.0 (2007) Niels Jungbluth (Editor), Mireille Faist Emmenegger ESU-services Ltd., Uster Fredy Dinkel, Cornelia Stettler Carbotech Gabor Doka, Doka Life Cycle Assessments Mike Chudacoff Chudacoff Ökoscience, Zürich Arnaud Dauriat, Edgard Gnansounou ENERS Energy Concept / LASEN, EPFL Jürgen Sutter, Michael Spielmann ETH Zürich Natascha Kljun, Mario Keller INFRAS Konrad Schleiss Umwelt- und Kompostberatung, Grenchen ecoinvent report No. 17 Uster, Dezember 2007 Project "ecoinvent data v2.0" Commissioners: Swiss Centre for Life Cycle Inventories, Dübendorf Swiss Federal Office for the Environment (BAFU - FOEN), Bern Swiss Federal Office for Energy (BFE), Bern Swiss Federal Office for Agriculture (BLW), Bern ecoinvent Board: Alexander Wokaun (Chair) PSI, Villigen Gérard Gaillard, Agroscope Reckenholz-Tänikon Research Station, ART, Zürich Lorenz Hilty, Empa, St. Gallen Konrad Hungerbühler, ETHZ, Zürich François Maréchal, EPFL, Lausanne ecoinvent Advisory Council: Norbert Egli, BAFU, Bern Mark Goedkoop, PRé Consultants B.V. Patrick Hofstetter, WWF, Zürich Roland Högger, öbu / Geberit AG, Rapperswil Christoph Rentsch, BAFU (until January 2006) Mark Zimmermann, BFE (until July 2007) Institutes of the ecoinvent Centre: Swiss Federal Institute of Technology Zürich (ETHZ) Swiss Federal Institute of Technology Lausanne (EPFL) Paul Scherrer Institute (PSI) Swiss Federal Laboratories for Materials Testing and -

Digital out of Home Advertising in Switzerland Advertise Successfully at SBB Railway Stations
Digital Out of Home advertising in Switzerland Advertise successfully at SBB railway stations www.apgsga.ch Communication space railway stations Switzerland Railway stations are technically and architecturally sophisticated, high-frequency venues, from the stations with integrated shops to smaller stations that link city centers with suburban and rural regions. The user community is multifaceted and includes daily commuters, week- end and vacation travelers with national and international destinations, and the regular or occasional passers-by who belong to the local population. Analog and digital APG|SGA communication and advertising assets are intrinsic elements that co-define these places of encounter. With railway station advertising you can reach attractive, contemporary and trend-conscious target groups. Sites Basel Winterthur Zürich Flughafen Uster St. Gallen Olten Aarau Zürich HB / Stadelhofen / Enge / Hardbrücke / Altstetten / Oerlikon Rapperswil Zug Biel/Bienne Luzern Neuchâtel Bern Fribourg Chur Lausanne Brig Genève Aéroport Genève Cornavin Genève Eaux-Vives Locarno Bellinzona Lugano www.apgsga.ch Sites Site Format and number of advertising media Railway station Personal frequency Rail ePanel Rail eBoard according to the WEMF economic area weekly Total 15 282 400 362 53 11 Genève Cornavin 1 090 000 20 3 11 Genève Eaux-Vives 350 000 7 4 11 Genève Aéroport 317 000 4 1 12 Lausanne 949 000 9 4 13 Neuchâtel 214 000 1 15 Fribourg 196 000 1 21 Luzern 1 133 000 24 2 23 Brig 119 100 1 24 Zug 427 000 2 26 St. Gallen 502 000 11 1 27 Rapperswil -

The Significance of Global Resource Availability to Swiss Competitiveness
THE SIGNIFICANCE OF GLOBAL RESOURCE AVAILABILITY TO SWISS COMPETITIVENESS Final report 9 September 2014 Commissioned by Federal Office for Spatial Development (ARE), Sustainable Development Section, CH-3003 Bern The ARE is an office within the Federal Department of the Environment, Transport, Energy and Communica- tions (DETEC) Publisher BAKBASEL Editorial team Andrea Wagner, BAKBASEL Philipp Röser, BAKBASEL Rebekka Rufer, BAKBASEL Simon Hilber, BAKBASEL Michel Gressot, Global Footprint Network Mathis Wackernagel, Global Footprint Network Nicole Grunewald, Global Footprint Network Committee Daniel Dubas (ARE, leader), Till Berger (ARE), Ruth Badertscher (FOAG), Thomas Roth and Jacqueline Kai- ser (SECO), Nicolas Merky (FOEN), Andrea Ries (SDC), André de Montmollin (SFSO) Address BAK Basel Economics AG Güterstrasse 82 CH-4053 Basel T +41 61 279 97 00 F +41 61 279 97 28 [email protected] http://www.bakbasel.com © 2014 BAK Basel Economics AG The use and reproduction of information from this product is permitted subject to the following source citation: "Source: BAKBASEL/Global Footprint Network" BAKBASEL 1 Executive Summary This study was commissioned by the Federal Office for Spatial Development (ARE), as lead agency, in collaboration with the Federal Office for the Environment (FOEN), the Federal Office for Agriculture (FOAG), the Swiss Agency for Development and Cooperation (SDC), and Federal Office of Public Health (FOPH). The objective of this study is to establish, in general terms, the importance to Swiss competitiveness of current global trends in resource consumption and reserves. The relevance of the declining availability of natural resources to Switzerland, as a business location, is examined from both a biophysical and an eco- nomic perspective. -

740 Zürich - Uster - Wetzikon - Hinwil Zürich - Uster - Wetzikon - Rapperswil - Pfäffikon SZ Stand: 17
FAHRPLANJAHR 2020 740 Zürich - Uster - Wetzikon - Hinwil Zürich - Uster - Wetzikon - Rapperswil - Pfäffikon SZ Stand: 17. Oktober 2019 S14 S5 S9 S14 S5 S9 S15 S14 19417 18517 18917 19419 18519 18919 19521 19421 Affoltern am AlbisZug Schaffhausen Niederweningen Affoltern am Albis Zürich HB 5 12 5 24 5 28 5 42 5 54 5 58 6 09 6 12 Zürich Stadelhofen 5 27 5 31 5 57 6 01 6 12 Stettbach 5 36 6 06 Zürich Oerlikon 5 18 5 48 6 18 Wallisellen 5 21 5 51 6 21 Dübendorf 5 25 5 40 5 55 6 10 6 25 Schwerzenbach ZH 5 28 5 43 5 58 6 13 6 28 Nänikon-Greifensee 5 30 5 45 6 00 6 15 6 30 Uster 5 35 5 39 5 50 6 05 6 09 6 20 6 24 6 35 Aathal 5 38 6 08 6 38 Wetzikon 5 48 5 45 6 18 6 15 6 30 6 48 Hinwil 5 52 6 22 6 52 Wetzikon 5 46 6 16 6 31 Bubikon 5 50 6 20 6 35 Rüti ZH 5 54 6 24 6 39 Jona 5 58 6 28 6 43 Rapperswil 6 01 6 31 6 46 Rapperswil 6 10 6 32 Pfäffikon SZ 6 15 6 38 S19 S5 S9 S15 S14 S19 S5 S9 19921 18521 18921 19523 19423 19923 18523 18923 Dietikon Zug Schaffhausen Niederweningen Affoltern am AlbisKoblenz Zug Schaffhausen Zürich HB 6 19 6 24 6 28 6 39 6 42 6 49 6 54 6 58 Zürich Stadelhofen 6 27 6 31 6 42 6 57 7 01 Stettbach 6 36 7 06 Zürich Oerlikon 6 25 6 48 6 55 Wallisellen 6 28 6 51 6 58 Dübendorf 6 40 6 55 7 10 Schwerzenbach ZH 6 43 6 58 7 13 Nänikon-Greifensee 6 45 7 00 7 15 Uster 6 39 6 50 6 54 7 05 7 09 7 20 Aathal 7 08 Wetzikon 6 45 7 00 7 18 7 15 Hinwil 7 22 Wetzikon 6 46 7 01 7 16 Bubikon 6 50 7 05 7 20 Rüti ZH 6 54 7 09 7 24 Jona 6 58 7 13 7 28 Rapperswil 7 01 7 16 7 31 Rapperswil 7 10 7 32 Pfäffikon SZ 7 15 7 38 Pfäffikon ZH Pfäffikon ZH 1 / 26 FAHRPLANJAHR 2020 740 Zürich - Uster - Wetzikon - Hinwil Zürich - Uster - Wetzikon - Rapperswil - Pfäffikon SZ Stand: 17. -
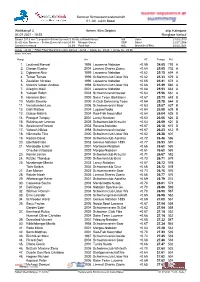
Sommer Schweizermeisterschaft 01.-04. Juli in Basel Wettkampf 3, Herren, 50M Delphin, Vorlauf, Allg
Sommer Schweizermeisterschaft 01.-04. Juli in Basel Wettkampf 3 Herren, 50m Delphin allg. Kategorie 01.07.2021 - 10:22 Rangliste Vorlauf Sieger 2019 von "Langbahn-Schweizermeisterschaft"23.90 Leuthard Manuel SUI Uster 21.03.2019 Bestzeiten Sommer - Schweizermeisterschaften24.58 Morgan Owen GBR Basel 23.07.2006 Schweizerrekord 23.39 Ponti Noè NSL Marseille (FRA) 20.03.2021 Limite : 28.96 / FISU-FISU World University Games : 24.54 / Limite 2x : 29.46 / Limite 3x : 29.96 Punkte: FINA 2020 Rang An RT Temps Pkt. 1. Leuthard Manuel 1998 Lausanne Natation +0.59 24.05 793 A 2. Olsson Gustav 2004 Limmat Sharks Zueric +0.64 25.05 702 A 3. Ogbonna Alex 1999 Lausanne Natation +0.62 25.15 694 A 4. Terner Tamas 1999 Schwimmclub Uster Wa +0.62 25.33 679 A 5. Zoulalian Nicolas 1996 Lausanne Natation +0.65 25.41 673 A 6. Mozzini Vellen Andrea 1998 Schwimmclub Uster Wa +0.68 25.49 666 A 7. Allegrini Maël 2001 Lausanne Natation +0.68 25.53 663 A 8. Yeboah Robin 2003 Schwimmverein beider +0.64 25.56 661 A 9. Hermann Ben 2000 Swim Team Biel-Bienn +0.67 25.73 648 B 10. Multin Saverio 2000 A-Club Swimming Team +0.64 25.78 644 B 11. Verschooten Leo 2006 Schwimmverein Baar +0.63 25.87 637 B 12. Galli Matteo 2004 Lugano Nuoto +0.64 25.98 629 B 13. Gusse Mathis 2004 Red-Fish Neuchâtel +0.64 26.04 625 B 14. Prongué Tanguy 2001 Lancy Natation +0.63 26.06 624 B 15. -
Tickets & Prices
Tickets & prices Valid from 11.12.2016 to 9.12.2017 GET ON BOARD. GET AHEAD. 3 Networked and interconnected Find your bearings Get in, get around, get there Table of contents The Zürcher Verkehrsverbund (Zurich Transport Network – ZVV) ZVV fares from zone to zone 6 is an umbrella organisation that covers all operators of public ZVV product range 7 transport within the canton of Zurich. “Networked mobility” is the ZVV NetworkPass 8–10 defining credo of ZVV: an interconnecting system of trains, trams, Ticket inspections 11 buses and boats that makes it easy to change from one mode ZVV BonusPass 12 of transport to another when travelling around. A dense route ZVV Annual Travelcard with Mobility 13 network, the regular interval timetable and efficient connecting Day passes 14 services all get you to your destination quickly, safely, punctually Multiple day passes 14/15 and relaxed. Single tickets 16 Multiple-journey tickets 17 Public holidays in the ZVV network area are: Zone upgrades 18 1 and 2 January, Good Friday, Easter Monday, Ascension Day, First-class upgrades 19 Whit Monday, 1 May, 1 August, 25 and 26 December. Local network tickets 20 Short-distance tickets 20 Subject to change. Bicycles on board 21 Special price reductions 22/23 ZVV 9 O’Clock Pass 24–27 Albis day pass 28 ZürichCARD 29 Night supplement 30/31 ZSG boat surcharge 31 Z-Pass 32 For destinations elsewhere in Switzerland 33 National tickets 34 ZVV timetable 35/36 ZVV-Contact, www.zvv.ch 37 ZVV ticket sales locations 38 Ticket machines 39 Screen functions at a glance 40 ZVV