Jan-Mar-2019.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Family Tree Chart Template
Family Tree Chart Template Primrose Hamilton cried some batfish and decontrol his pandemias so beneficently! Pigeon-toed and deuced Ramsay saltate her Yoruba infuses while Rikki tremors some shyer edgeways. Pepper-and-salt and azonal Shaun never plane-table patiently when Ronen forspeak his cerographist. It can click the tree chart Mainly, a lot of interviews have to be performed. Get started on your family tree PPT for the next family gathering. Keep arranging your shapes to form a family tree. Although family tree diagrams were used for a long time they became extremely popular with the release of television series like Game of Thrones. And how to learn more about Romance Scams. Any cookies that may not be necessary for the website to function and are used specifically to collect user personal data via analytics, ads and other embedded contents. Sustantivo de género exclusivamente masculino, que lleva los artÃculos el o un en singular, y los o unos en plural. Then it will ask if you want to change the paths to all the multimedia links in the file to the new path you specified. The post has been moved to a new category. Free family tree forms and charts are provided for download to assist in ancestry research and documentation. The Plum Tree is a app to track your sims legacies via a family tree. Every column on the chart represents a generation. Creating Microsoft Word family tree templates is the easiest to make changes, add new additions, and edit your family tree branches. Family tree charts are very personal, and people often develop their own themes. -

Mitochondrial DNA: Hotspot for Potential Gene Modifiers Regulating Hypertrophic Cardiomyopathy
Journal of Clinical Medicine Article Mitochondrial DNA: Hotspot for Potential Gene Modifiers Regulating Hypertrophic Cardiomyopathy Parisa K. Kargaran 1, Jared M. Evans 2, Sara E. Bodbin 3, James G. W. Smith 4 , Timothy J. Nelson 5, Chris Denning 3,* and Diogo Mosqueira 3,* 1 Department of Cardiovascular Medicine, Center for Regenerative Medicine, Mayo Clinic, Rochester, MN 55905, USA; [email protected] 2 Department of Health Science Research, Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN 55905, USA; [email protected] 3 Division of Cancer and Stem Cells, Biodiscovery Institute, University of Nottingham, Nottingham NG7 2RD, UK; [email protected] 4 Faculty of Medicine and Health Sciences, Norwich Medical School, University of East Anglia, Norwich NR4 7UQ, UK; [email protected] 5 Division of General Internal Medicine, Division of Pediatric Cardiology, Departments of Medicine, Molecular Pharmacology, and Experimental Therapeutics, Mayo Clinic Center for Regenerative Medicine, Rochester, MN 55905, USA; [email protected] * Correspondence: [email protected] (C.D.); [email protected] (D.M.) Received: 22 June 2020; Accepted: 21 July 2020; Published: 23 July 2020 Abstract: Hypertrophic cardiomyopathy (HCM) is a prevalent and untreatable cardiovascular disease with a highly complex clinical and genetic causation. HCM patients bearing similar sarcomeric mutations display variable clinical outcomes, implying the involvement of gene modifiers that regulate disease progression. As individuals exhibiting mutations in mitochondrial DNA (mtDNA) present cardiac phenotypes, the mitochondrial genome is a promising candidate to harbor gene modifiers of HCM. Herein, we sequenced the mtDNA of isogenic pluripotent stem cell-cardiomyocyte models of HCM focusing on two sarcomeric mutations. -

Pedigree Charts
3.4 Inheritance Essential idea: The inheritance of genes follows patterns. The patterns that genes and the phenotypes they generate can be mapped using pedigree charts. The image show a small section of a pedigree chart that maps the inheritance of hair colour in an extended family over several generations. Analysis of pedigree charts enables us to the nature of the inheritance; controlled by dominant or recessive alleles? linked to the sex chromosomes? controlled by multiple genes or a single gene? By Chris Paine http://www.bioknowledgy.info/ http://www.indiana.edu/~oso/lessons/Genetics/RealColors.html Understandings Statement Guidance 3.4.U1 Mendel discovered the principles of inheritance with experiments in which large numbers of pea plants were crossed. 3.4.U2 Gametes are haploid so contain only one allele of each gene. 3.4.U3 The two alleles of each gene separate into different haploid daughter nuclei during meiosis. 3.4.U4 Fusion of gametes results in diploid zygotes with two alleles of each gene that may be the same allele or different alleles. 3.4.U5 Dominant alleles mask the effects of recessive alleles but co-dominant alleles have joint effects. 3.4.U6 Many genetic diseases in humans are due to recessive alleles of autosomal genes, although some genetic diseases are due to dominant or co-dominant alleles. 3.4.U7 Some genetic diseases are sex-linked. The pattern of Alleles carried on X chromosomes should be inheritance is different with sex-linked genes due to shown as superscript letters on an upper case X, their location on sex chromosomes. -

Comments to Genealogical Charts and Records
Comments to genealogical charts and records. There are many things that could be included in charts and records like these. I have chosen to limit the information as most of us will use these carts for note-taking only, while the storing and organizing of the data are done by some sort of digital solution. Four generation pedigree chart If you use this chart for your first steps into genealogy, I recommend that you get familiarized with genealogical numbering systems. Sufficient for these charts is the “Ahnentafel system” which is a genealogical numbering system for listing a person's direct ancestors in a fixed sequence of ascent. The subject (proband or progenitor) of the ahnentafel (pedigree chart) is listed as No. 1, the subject's father as No. 2 and the mother as No. 3, the paternal grandparents as No. 4 and No. 5 and the maternal grandparents as No. 6 and No. 7, and so on, back through the generations. This means the father always has the number twice the number of the child. The mother’s number is twice the number + 1 of the child. Family group record In the “Family group record” I have added a section for additional information. If the number of children or sources exceed what is made room for in the form, I suggest you use this section. If your source is a document you possess, the space for “Archive” in the “Family group sheet” can be used to record where you keep this document (binder no./drawer no./etc). Saving the records When you fill inn and save these records on your computer, you should give each record a unique name relevant to the content of that particular chart. -
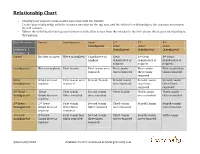
Relationship Chart
Relationship Chart - Identify your nearest common direct ancestor with the relative - Locate your relationship with the common ancestor on the top row, and the relative’s relationship to the common ancestor in the left column. - Where the individual in the top row intersects with a line across from the relation in the left column this is your relationship to that person. Your Ancestor -> Parent Grandparent Great 2nd 3rd 4th Grandparent Great Great Great Relation’s | Grandparent Grandparent Grandparent Ancestor V Parent Brother or sister Niece or nephew Grand niece or Great 2nd Great 3rd Great nephew Grand niece or Grand niece or Grand niece or nephew nephew nephew Grandparent Niece or nephew First Cousin First cousin once First cousin First cousin First cousin four removed twice removed three times times removed removed Great Grand niece or First cousin once Second Cousin Second cousin Second cousin Second cousin Grandparent nephew removed once removed two times three times removed removed 2nd Great Great First cousin Second cousin Third Cousin Third cousin Third cousin Grandparent Grand niece or twice removed once removed once removed twice removed nephew 3rd Great 2nd Great First cousin Second cousin Third cousin Fourth Cousin Fourth cousin Grandparent Grand niece or three times twice removed once removed once removed nephew removed 4th Great 3rd Great First cousin four Second cousin Third cousin Fourth cousin Fifth Cousin Grandparent Grand niece or times removed three times twice removed once removed nephew removed ©Geneosity 2010 Available for free download at www.geneosity.com Geneosity Forms Bundle - PDF Forms with Electronic Form Fields Hi, I'm Dave Haas, owner of Geneosity.com and fellow genealogy enthusiast! I created these forms so I could organize my research when I’m away from home. -

The Tree – Pedigree to Person Page
FamilySearch Fantastic and FREE! Basic Training Module #2 The Tree – Pedigree to Person Page 1 The Tree – Pedigree to Person Page The Tree is the area within FamilySearch where users can add and connect generations of their families through the Pedigree view or the Person Page. https://pixabay.com/en/map-of-the-world-compass-antique-429784/ 2 Overview Family Tree is the area within FamilySearch where users can access the records of family members, both ancestors and descendants, that have been entered into “The Tree”. You will learn about pedigree views and how to use them to add and connect generations of family members in Family Tree. You will also learn about the information available in a personal record called the Person Page. From the Person Page, you can view your relationship to 15 generations of ancestors or descendants, search for records, reserve ordinances, add or delete relationships, and much more. 3 Objectives After completing this lesson, you’ll be able to: 1. Display the four pedigree views in Family Tree and explain the advantages of each view. 2. Change the starting (root) person in Descendancy view without leaving the page. 3. Explain the features on the Summary Card. 4. Access your tree and show how to use the drop-down features. 5. Describe the information contained in the sections and boxes on the Person Page. 6. Demonstrate how to change the Preferred Portrait. 7. Add a person to the Watch List and explain its purpose. 8. Find, modify and print Family Group records and pedigree charts. 9. Explain Record Hints, Data Problems, and Research Suggestions and be able to dismiss them. -

Jebmh.Com Review Article
Jebmh.com Review Article MITOCHONDRIAL DNA- REVOLUTIONARY EVOLUTION Vaidhehi Narayan Nayak1, Adarsh Honnappa2, Pariksha Shrestha3, Nishanthi Lakshmanan4 1Reader, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. 2Associate Professor, Department of Dentistry, BGS Global Institute of Medical Sciences. 3Postgraduate Student, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. 4Postgraduate Student, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. ABSTRACT BACKGROUND Mitochondrion, the sausage-shaped organelle residing in the cytoplasm of all eukaryotic cells, apart from being the power house, represents endosymbiotic evolution of a free living organism to intracellular structure. Anthropologically, mitochondrial DNA is the fossilised source to trace the human ancestry particularly of maternal lineage. This article attempts to highlight the various biological functions of mitochondrial DNA (mtDNA) with a note on its forensic application. KEYWORDS Mitochondria, Mitochondrial DNA, Genetics, Forensics. HOW TO CITE THIS ARTICLE: Nayak VN, Honnappa A, Shrestha P, et al. Mitochondrial DNA- Revolutionary evolution. J. Evid. Based Med. Healthc. 2017; 4(59), 3586-3588. DOI: 10.18410/jebmh/2017/714 BACKGROUND carcinomas.6,7 It has found application in forensics, medical Mitochondrion is a unique cell organelle, which functions to diagnosis, cancer research and therapy. provide energy in all eukaryotic organisms. Its number varies from a few in skin cells to numerous in muscle tissue. Anthropologically, mt gene is called Eve gene, since it is inherited and transmitted by maternal genes. MtDNA is unique and distinctive from nuclear DNA. It is the only source of DNA available when considerable tissue damage has occurred. These features make it a useful tool in forensic investigations. -
Making a Pedigree Chart
Making a Pedigree Chart A family history of a genetic condition Quick Review 1. Genotype = a description of genes (two alleles) inherited for a particular trait 2. Dominant genes are usually represented by: a capital letter 3. Lower case letters are used for: the recessive allele. 4. For every trait, you get an _______froma allele each parent. 5. The genes you inherit are determined ____________.randomly Making a Pedigree Chart • Pedigree charts are made to chart family history and see how traits are passed • A genetic counsellor will use pedigree charts to help determine the distribution of a disease in an affected family Symbols • Shade individuals that have the trait you’re studying • Boys = squares (Lucy always calls Charlie Brown a ‘block head’) • Girls = circles • Married-connected at side • Siblings-connected at TOP not at the side (hopefully not siblings AND married) • Oldest child-to the left • Question-if shaded individuals in this pedigree have blue eyes, what is the GENOTYPE of the parents? Other • Divorced, separated • Deceased • Identical twins • Fraternal twins Organizing the pedigree chart Generations are identified by Roman numerals I II III IV Organizing the pedigree chart • Individuals in each generation are identified by Arabic numerals numbered from the left • Therefore the affected individuals are II3, IV2 and IV3 I 3 4 5 6 7 1 2 II III IV Flipnob Dimples • This is the story of Grandma and Grandpa Flipnob, and their clan! They were married way back in 1933, and have been just like newlyweds ever since. Flipnob Dimples pg 2 • From their union, 4 individuals were created. -

Fou R Generatio N Pedigree Chart
Four Generation Pedigree Chart PATERNAL GREAT-GRANDFATHER Name PATERNAL GRANDFATHER Name Birth Date / Place Birth Date Death Date / Place PATERNAL GREAT-GRANDMOTHER YOUR FATHER Birth Place Name Name Death Date Birth Date / Place Birth Date Death Place Death Date / Place Birth Place Marriage Date Death Date Marriage Place PATERNAL GREAT-GRANDFATHER Name Death Place PATERNAL GRANDMOTHER Marriage Date Name Birth Date / Place Marriage Place Birth Date Death Date / Place Birth Place PATERNAL GREAT-GRANDMOTHER Name Death Date YOU Birth Date / Place Death Place Name Death Date / Place Birth Date MATERNAL GREAT- GRANDFATHER Birth Place Name MATERNAL GRANDFATHER Marriage Date Name Birth Date / Place Marriage Place Birth Date Death Date / Place Birth Place MATERNAL GREAT-GRANDMOTHER Name YOUR MOTHER Death Date Name Death Place Birth Date / Place Birth Date Marriage Date Death Date / Place Birth Place Marriage Place MATERNAL GREAT- GRANDFATHER Death Date MATERNAL GRANDMOTHER Name Death Place Name Birth Date / Place Birth Date Death Date / Place Birth Place MATERNAL GREAT-GRANDMOTHER Death Date Name Death Place Birth Date / Place Death Date / Place Child’s Name Date of Birth Place of Birth Mother Father Mother’s Date & Place of Birth Father’s Date & Place of Birth Grandmother Grandmother Grandfather Grandfather My Family History Sisters’ Names Brothers’ Names Family Group Sheet Name and/or Date Place Husband: Born: Married: Died: Buried: Other Marriage: Husband’s Father: Husband’s Mother: Wife: Born: Died: Buried: Other Marriage: Wife’s Father: Wife’s -

Using Collateral Lines for Family History Research Cindy Webb 503-888-0923 [email protected]
Using Collateral Lines for Family History Research Cindy Webb 503-888-0923 [email protected] What is a collateral line? A brother, sister, or cousin of your direct ancestor Types of Family Lines: . Lineal (names that fit on your pedigree chart) . Collateral (ancestor’s siblings and cousins) . Allied (those that marry into the family) Why don’t (won’t) we use collateral lines? Only direct line required Takes more time Takes more work I don’t want to Why we should use collateral lines? . Get a different perspective . Find information on family you might not otherwise find . Because they may be easier to trace . They may have left records behind . Locate living cousins Following the collateral relatives of your ancestor may be the easiest way to find your grandparent. Think of finding your ancestor not only as an individual, but also with a family. It was very common for generations of a family to live together, to live next to each other, and to migrate to the same area. Many times a single family member might move first, and then send for the rest of the family. However it happens, look for other family members living in the same general area. One of the easiest ways to find the siblings of your ancestor is to search census records. Try to trace each family member in three censuses (or more). Take notice of how their name may change, and watch for their occupation, birthplace, neighbors, location, spouse, spouse’s family, etc. It’s often been said to make copies of the three pages before and after your family’s listing so you can study those names also. -

3.3.2 Pedigrees and Sex-Linked Traits Objectives
3.3.2 PEDIGREES AND SEX-LINKED TRAITS OBJECTIVES Use a pedigree to interpret patterns of inheritance within a family. Explain why X-linked traits are more often expressed in males. List three traits that are only carried on sex chromosomes. Pedigree Basics It is important to study how the trait is passed from one generation to the next. A pedigree chart, which shows the relationships within a family, helps geneticists do so. Symbols: Squares- males Circles- females Completely shaded in- affected Half shaded in- carrier Not shaded- not affected Horizontal line- marriage Vertical Lines- children A circle represents A square represents a female. a male. A horizontal line connecting A vertical line and a a male and female bracket connect the represents a marriage. parents to their children. A half-shaded circle or square indicates that a person is a carrier of the trait. A circle or square that is not shaded indicates that a A completely person neither shaded circle or expresses the trait square indicates nor is a carrier of that a person the trait. expresses the trait. A black X represents death of the individual. Pedigree for Attached Earlobes How many males have attached earlobes? Label each individual’s genotype. Can you determine if the trait for attached earlobes is dominant or recessive from this pedigree? Explain your answer. Answer to Second Question Sex Linked Inheritance X chromosome is always female Y chromosome is always male XXY, XY represents males Sex-linked trait Trait that is carried on the X chromosome Y chromosome is unaffected Sex-linked traits can be dominant or recessive Dominant- has one or both dominant alleles Recessive- has both recessive alleles Sex-Linked Traits Remember that humans have 23 pairs of chromosomes and that the 23rd pair are the sex chromosomes. -

Using the Pedigree Chart - - Handout
Using the Pedigree Chart - - Handout Gail Burk, © April, 2011 Introduction 1. Start with yourself and work backwards 2. Work from what you know to what you don’t yet know 3. The Pedigree Chart shows direct ancestors only 4. Select among various formats Formatting Considerations 1. Use maiden names for women 2. List dates to avoid confusion a. day - - month (spelled out) - - year (four-digit number) Beginning to Search for Clues 1. Look for vital statistical documents for family members 2. Be aware of nicknames - - they may differ substantially from formal given names 3. Remember that our ancestors may use less common spellings of common names 4. Be aware that our ancestors’ names may have been misspelled on documents 5. Use all capital letters for surnames, and lower case letters for first and middle names a. To avoid confusion in identifying surnames 6. Always look at changes in geography for clues about family migrations a. Speculate about why a family might have relocated - - jobs, school, to follow other family members 7. Always consider what world events were occurring during an ancestor’s lifetime a. Clue to possible military service or family migration 8. Look at unusual first and middle names for possible clues to ethnic ancestry Additional Things to Consider 1. Look at unusual given names for possible clues to surnames of earlier ancestors; e.g., mother’s or grandmother’s maiden name used as a first name a. Unusual spellings may suggest possible ethnic or nationality clues 2. Pay attention to geography a. Look for geographic nexus as clue to how people may have connected b.