Social Factors Influencing Family Planning Knowledge, Attitudes, and Practices in The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
View the Floating Doctors Volunteer Handbook
Volunteer Handbook 1 Last Update 2016_07_30 Table of Contents 1. Floating Doctors a. Mission Statement b. Goals 2. Scope of Work a. Mobile Clinics b. Mobile Imaging c. Public Health Research d. Health Education e. Professional Training f. Patient Chaperoning g. Ethnomedicine h. Asilo i. Community Projects 3. Pre-Arrival Information a. Bocas del Toro b. Packing List c. Traveling to Bocas del Toro d. Arrival in Bocas 4. Volunteer Policies a. Work Standards b. Crew Code of Ethics and Conduct 5. Health and Safety a. Purpose b. Staying Healthy c. Safety Considerations 6. Financial Guidelines a. Volunteer Contributions b. Floating Doctors Contributions c. Personal Expenses 7. On-Site Logistics a. Community Guidelines b. Curfew c. Keys d. Laundry e. Resources f. Recycling 8. Living in Bocas a. Floating Doctors Discounts b. Groceries c. Restaurants d. Internet e. Phone 9. Basic Weekly Schedule a. Typical Weekly Schedule b. What to Expect on a Clinic Day c. What to Expect on a Multi-Day Clinic 10. Phone List 2 Last Update 2016_07_30 I. Floating Doctors Mission Statement The Floating Doctors’ ongoing mission is to reduce the present and future burden of disease in the developing world, and to promote improvements in health care delivery worldwide. Goals Our goals include: 1. Providing free acute and preventative health care services and delivering donated medical supplies to isolated areas. 2. Reducing child and maternal mortality through food safety/prenatal education, nutritional counseling and clean water solutions. 3. Studying and documenting local systems of health care delivery and identifying what progress have been made, what challenges remain, and what solutions exist to improve health care delivery worldwide. -

Financing Plan, Which Is the Origin of This Proposal
PROJECT DEVELOPMENT FACILITY REQUEST FOR PIPELINE ENTRY AND PDF-B APPROVAL AGENCY’S PROJECT ID: RS-X1006 FINANCINGIDB PDF* PLANIndicate CO-FINANCING (US$)approval 400,000date ( estimatedof PDFA ) ** If supplemental, indicate amount and date GEFSEC PROJECT ID: GEFNational ALLOCATION Contribution 60,000 of originally approved PDF COUNTRY: Costa Rica and Panama ProjectOthers (estimated) 3,000,000 PROJECT TITLE: Integrated Ecosystem Management of ProjectSub-Total Co-financing PDF Co- 960,000 the Binational Sixaola River Basin (estimated)financing: 8,500,000 GEF AGENCY: IDB Total PDF Project 960,000 OTHER EXECUTING AGENCY(IES): Financing:PDF A* DURATION: 8 months PDF B** (estimated) 500,000 GEF FOCAL AREA: Biodiversity PDF C GEF OPERATIONAL PROGRAM: OP12 Sub-Total GEF PDF 500,000 GEF STRATEGIC PRIORITY: BD-1, BD-2, IW-1, IW-3, EM-1 ESTIMATED STARTING DATE: January 2005 ESTIMATED WP ENTRY DATE: January 2006 PIPELINE ENTRY DATE: November 2004 RECORD OF ENDORSEMENT ON BEHALF OF THE GOVERNMENT: Ricardo Ulate, GEF Operational Focal Point, 02/27/04 Ministry of Environment and Energy (MINAE), Costa Rica Ricardo Anguizola, General Administrator of the 01/13/04 National Environment Authority (ANAM), Panama This proposal has been prepared in accordance with GEF policies and procedures and meets the standards of the GEF Project Review Criteria for approval. IA/ExA Coordinator Henrik Franklin Janine Ferretti Project Contact Person Date: November 8, 2004 Tel. and email: 202-623-2010 1 [email protected] PART I - PROJECT CONCEPT A - SUMMARY The bi-national Sixaola river basin has an area of 2,843.3 km2, 19% of which are in Panama and 81% in Costa Rica. -

Socioeconomic Characterization of Bocas Del Toro in Panama: an Application of Multivariate Techniques
Revista Brasileira de Gestão e Desenvolvimento Regional G&DR. V. 16, N. 3, P. 59-71, set-dez/2020. Taubaté, SP, Brasil. ISSN: 1809-239X Received: 11/14/2019 Accepted: 04/26/2020 SOCIOECONOMIC CHARACTERIZATION OF BOCAS DEL TORO IN PANAMA: AN APPLICATION OF MULTIVARIATE TECHNIQUES CARACTERIZACIÓN SOCIOECONÓMICA DE BOCAS DEL TORO EN PANAMÁ: UNA APLICACIÓN DE TÉCNICAS MULTIVARIADAS Barlin Orlando Olivares1 Jacob Pitti2 Edilberto Montenegro3 Abstract The objective of this work was to identify the main socioeconomic characteristics of the villages with an agricultural vocation in the Bocas del Toro district, Panama, through multivariate techniques. The two principal components that accounted for 84.0% of the total variation were selected using the Principal Components Analysis. This allowed a classification in three strata, discriminating the populated centers of greater agricultural activity in the district. The study identified that the factors with the greatest impact on the characteristics of the population studied were: the development of agriculture in indigenous territories, the proportion of economically inactive people and economic occupation other than agriculture; This characterization serves as the first approach to the study of sustainable land management in indigenous territories. Keywords: Applied Economy, Biodiversity, Crops, Multivariate Statistics, Sustainability. Resumen El objetivo de este trabajo fue identificar las principales características socioeconómicas de los poblados con vocación agrícola del distrito Bocas del Toro, Panamá, a través de técnicas multivariadas. Mediante el Análisis de Componentes Principales se seleccionaron los primeros dos componentes que explicaban el 84.0 % de la variación total. Esto permitió una clasificación en tres estratos, discriminando los centros poblados de mayor actividad agrícola en el distrito. -

1 Bocas Del Toro Cauchero Esc
CALENDARIO DE BECA UNIVERSAL Y PLANILLA GLOBAL TERCERA ENTREGA 2019 DIRECCIÓN PROVINCIAL DE BOCAS DEL TORO 23 DE OCTUBRE DE 2019 Nº DISTRITO CORREGIMIENTO CENTRO EDUCATIVO 1 CHIRIQUÍ GRANDE CHIRIQUÍ GRANDE DIONISIA G. DE AYARZA 2 CHIRIQUÍ GRANDE CHIRIQUÍ GRANDE LAS PIÑAS 3 CHIRIQUÍ GRANDE CHIRIQUÍ GRANDE QUEBRADA EL BAJO 4 CHIRIQUÍ GRANDE CHIRIQUÍ GRANDE QUEBRADA LIMÓN 5 CHIRIQUÍ GRANDE RAMBALA RAMBALA 6 CHIRIQUÍ GRANDE RAMBALA CHIRIQUICITO # 1 7 CHIRIQUÍ GRANDE RAMBALA CHIRIQUICITO # 2 8 CHIRIQUÍ GRANDE RAMBALA CENTRO BET-EL 9 CHIRIQUÍ GRANDE RAMBALA NUEVA ESTRELLA 10 CHIRIQUÍ GRANDE PUNTA PEÑA I.P.T CHIRIQUÍ GRANDE 11 CHIRIQUÍ GRANDE PUNTA PEÑA C.E.B.G. PUNTA PEÑA 12 CHIRIQUÍ GRANDE PUNTA PEÑA CAÑAZAS 13 CHIRIQUÍ GRANDE MIRAMAR MIRAMAR 14 CHIRIQUÍ GRANDE MIRAMAR ALTO LA GLORIA 15 CHIRIQUÍ GRANDE MIRAMAR LAS CAÑAS 16 CHIRIQUÍ GRANDE MIRAMAR LOS MOLEJONES 17 CHIRIQUÍ GRANDE MIRAMAR LOS CHIRICANOS 18 CHIRIQUÍ GRANDE PUNTA ROBALO PALMA REAL 19 CHIRIQUÍ GRANDE PUNTA ROBALO VALLE SECO 20 CHIRIQUÍ GRANDE PUNTA ROBALO PUNTA ROBALO 21 CHIRIQUÍ GRANDE PUNTA ROBALO LA CONGA 22 CHIRIQUÍ GRANDE BAJO CEDRO C.E.B.G. BAJO CEDRO 23 CHIRIQUÍ GRANDE BAJO CEDRO QUEBRADA GARZA 24 CHIRIQUÍ GRANDE BAJO CEDRO ALTO CEDRO 25 CHIRIQUÍ GRANDE BAJO CEDRO C.E.B.G. RÍO AUYAMA 26 CHIRIQUÍ GRANDE BAJO CEDRO EL ESCOBAL 24 DE OCTUBRE DE 2019 Nº DISTRITO CORREGIMIENTO CENTRO EDUCATIVO 1 BOCAS DEL TORO CAUCHERO ESC. CAUCHERO ARRIBA 2 BOCAS DEL TORO CAUCHERO ESC. LOS HIGUERONES 3 BOCAS DEL TORO CAUCHERO ESC. LOMA AZUL 4 BOCAS DEL TORO CAUCHERO ESC. LOMA ESTRELLA 5 BOCAS DEL TORO CAUCHERO ESC. -
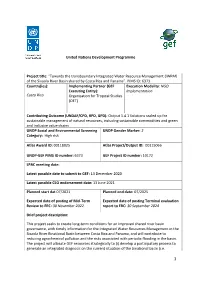
United Nations Development Programme Project Title
ƑPROJECT INDICATOR 10 United Nations Development Programme Project title: “Towards the transboundary Integrated Water Resource Management (IWRM) of the Sixaola River Basin shared by Costa Rica and Panama”. PIMS ID: 6373 Country(ies): Implementing Partner (GEF Execution Modality: NGO Executing Entity): Implementation Costa Rica Organisation for Tropical Studies (OET) Contributing Outcome (UNDAF/CPD, RPD, GPD): Output 1.4.1 Solutions scaled up for sustainable management of natural resources, including sustainable commodities and green and inclusive value chains UNDP Social and Environmental Screening UNDP Gender Marker: 2 Category: High risk Atlas Award ID: 00118025 Atlas Project/Output ID: 00115066 UNDP-GEF PIMS ID number: 6373 GEF Project ID number: 10172 LPAC meeting date: Latest possible date to submit to GEF: 13 December 2020 Latest possible CEO endorsement date: 13 June 2021 Planned start dat 07/2021 Planned end date: 07/2025 Expected date of posting of Mid-Term Expected date of posting Terminal evaluation Review to ERC: 30 November 2022. report to ERC: 30 September 2024 Brief project description: This project seeks to create long-term conditions for an improved shared river basin governance, with timely information for the Integrated Water Resources Management in the Sixaola River Binational Basin between Costa Rica and Panama, and will contribute to reducing agrochemical pollution and the risks associated with periodic flooding in the basin. The project will allocate GEF resources strategically to (i) develop a participatory process to generate an integrated diagnosis on the current situation of the binational basin (i.e. 1 Transboundary Diagnostic Analysis - TDA) and a formal binding instrument adopted by both countries (i.e. -

Panama: Land Administration Project (Loan No
Report No. 56565-PA Investigation Report Panama: Land Administration Project (Loan No. 7045-PAN) September 16, 2010 About the Panel The Inspection Panel was created in September 1993 by the Board of Executive Directors of the World Bank to serve as an independent mechanism to ensure accountability in Bank operations with respect to its policies and procedures. The Inspection Panel is an instrument for groups of two or more private citizens who believe that they or their interests have been or could be harmed by Bank-financed activities to present their concerns through a Request for Inspection. In short, the Panel provides a link between the Bank and the people who are likely to be affected by the projects it finances. Members of the Panel are selected “on the basis of their ability to deal thoroughly and fairly with the request brought to them, their integrity and their independence from the Bank’s Management, and their exposure to developmental issues and to living conditions in developing countries.”1 The three-member Panel is empowered, subject to Board approval, to investigate problems that are alleged to have arisen as a result of the Bank having failed to comply with its own operating policies and procedures. Processing Requests After the Panel receives a Request for Inspection it is processed as follows: • The Panel decides whether the Request is prima facie not barred from Panel consideration. • The Panel registers the Request—a purely administrative procedure. • The Panel sends the Request to Bank Management, which has 21 working days to respond to the allegations of the Requesters. -

Notes on Amphibians and Reptiles from Western Panama
Herpetology Notes, volume 13: 219-229 (2020) (published online on 09 March 2020) Notes on amphibians and reptiles from western Panama Abel Batista1,5,*, Andreas Hertz4, Marcos Ponce2, and Sebastian Lotzkat3 Abstract. Panama is a hotspot of amphibian and reptile diversity and many areas of the country still remain underexplored. Here we present results of our field work carried out through several years in western Panama, further increasing the numbers of amphibian and reptile species known from the country. We provide the first country records for Smilisca manisorum and Lepidophyma reticulatum. Additionally, we extend the known distributional ranges of Pristimantis taeniatus, Pleurodema brachyops, Leptodactylus fuscus, Bachia blairi, Basiliscus plumifrons, Anolis auratus, A. capito, A. cryptolimifrons, A. humilis, A. kemptoni, A. pseudopachypus, Geophis godmani, Mastigodryas pleei, and Bothriechis supraciliaris. Keywords. Amphibia, distribution, new record, herpetofauna, Panama, Reptilia Introduction van den Burg, 2012). Despite these manifold novelties, the amount of herpetological exploration in western The herpetofauna of Panama has been studied in Panama is still unsatisfactory (Köhler et al., 2008; various areas, with most work concentrated in central Lotzkat, 2014; Hertz, 2015). Panama (Ibáñez et al., 2001; Crawford et al. 2010; The aim of this paper is to provide new records of Voyles et al., 2018). However, there are notable surveys amphibians and reptiles from western Panama, as a since the mid-nineteenth century that were carried out in result of our surveys in the region from 2004 to 2012. western Panama (e.g., Dunn, 1924, 1940, 1947; Slevin, We include two new country records for Panama, and 1942; Myers and Duellman, 1982; see summaries in 14 distribution extensions. -

3 Bocas Del Toro Esc
CALENDARIOS DE BECA UNIVERSAL Y PLANILLA GLOBAL PRIMERA ENTREGA 2019 REGIONAL DE BOCAS DEL TORO LUNES, 25 DE JUNIO 2018 # CORREGIMIENTO CENTRO EDUCATIVO 1 GUABITO C.E.B.G.GUABITO 2 GUABITO COL. SECUNDARIO DE GUABITO 3 GUABITO ESC.FINCA 41 ANEXA DE GUABITO 4 GUABITO ESC.PUENTE BLANCO 5 GUABITO ESC.FINCA 54 6 GUABITO ESC.FINCA CALIFORNIA 7 GUABITO ESC.DEBORA 8 TERIBE ESC. BONYIC 9 TERIBE ESC. BAJO SORÍ 10 TERIBE ESC.CUYN KING 11 TERIBE C.E.B.G.SIEYICK 12 TERIBE ESC. SIENKING 13 TERIBE ESC.TRES PIEDRA 14 TERIBE ESC. SOLÓN 15 TERIBE ESC.LOMA BANDERA 16 TERIBE ESC. SAN SAN 17 TERIBE ESC.SAN SAN MONA 18 TERIBE ESC.SAN SAN TIGRA 19 TERIBE ESC.SAN SAN DRURY 20 LAS TABLAS C.E.B.G.MARIANO THOMAS 21 LAS TABLAS COL. SECUNDARIO NIEVECITA 22 LAS TABLAS C.E.B.G.NIEVECITA 23 LAS TABLAS ESC. DOS CAÑOS ANEXA 24 LAS TABLAS ESC.BARRANCO ADENTRO 25 LAS TABLAS ESC. BARRANCO MEDIO 26 LAS TABLAS ESC. BOCA DE YORKIN 27 LAS TABLAS ESC. BOCA DE YORKIN ANEXA 28 LAS TABLAS ESC. DOS CAÑOS 29 LAS TABLAS ESC. DOS CAÑO ABAJO 30 LAS TABLAS ESC. ALTO DOS CAÑOS 31 LAS TABLAS ESC. BISIRA # 3 32 LAS TABLAS ESC. QUEBRADA CANELA MARTES, 12 DE MARZO DE 2019 # CORREGIMIENTO CENTRO EDUCATIVO 1 CHANGUINOLA ESC. 4 DE ABRIL 2 CHANGUINOLA ESC. CHANGUINOLA 3 CHANGUINOLA ESC. FINCA 11 4 CHANGUINOLA C.E.B.G. FINCA 32 5 CHANGUINOLA ESC. FINCA 41 6 CHANGUINOLA ESC. FINCA 43 7 CHANGUINOLA ESC. FINCA 44 8 CHANGUINOLA ESC. -
General Assembly Distr
UNITED NATIONS A General Assembly Distr. GENERAL A/HRC/12/34/Add.5 3 September 2009 ENGLISH Original: SPANISH HUMAN RIGHTS COUNCIL Twelfth session Agenda item 3 PROMOTION AND PROTECTION OF ALL HUMAN RIGHTS, CIVIL, POLITICAL, ECONOMIC, SOCIAL AND CULTURAL RIGHTS, INCLUDING THE RIGHT TO DEVELOPMENT Report of the Special Rapporteur on the situation of human rights and fundamental freedoms of indigenous people, James Anaya* Addendum MISSION TO PANAMA** * Late submission. ** The summary of the report is being circulated in all official languages. The report itself, contained in the annex to the summary, is being circulated in the language of submission. GE.09-15231 (E) 250909 280909 A/HRC/12/34/Add.5 page 2 Summary The Special Rapporteur on the situation of human rights and fundamental freedoms of indigenous people, James Anaya, carried out a visit to Panama from 27 to 30 January 2009, at the invitation of the Government. The aim of the visit was to gain a broader knowledge of the situation of the Charco la Pava community and other communities affected by the Chan 75 hydroelectric project in the Changuinola District, Bocas del Toro Province, Panama, in order to make recommendations to the State on measures that could help to improve the situation, within the framework of the international standards on the rights of indigenous peoples. During his visit, the Special Rapporteur was able to gain a greater appreciation of the situation and maintain a constructive dialogue with several ministries and government agencies; representatives of Charco la Pava and other communities affected by the hydroelectric project; the company in charge of the project, AES Changuinola; United Nations agencies in Panama; and other stakeholders. -

University of Florida Thesis Or Dissertation Formatting Template
INDIGENOUS MOBILIZATION, INSTITUTIONALIZATION AND RESISTANCE: THE NGOBE MOVEMENT FOR POLITICAL AUTONOMY IN WESTERN PANAMA By OSVALDO JORDAN-RAMOS A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2010 1 © 2010 Osvaldo Jordan Ramos 2 A mi madre Cristina por todos sus sacrificios y su dedicacion para que yo pudiera terminar este doctorado A todos los abuelos y abuelas del pueblo de La Chorrera, Que me perdonen por todo el tiempo que no pude pasar con ustedes. Quiero que sepan que siempre los tuve muy presentes en mi corazón, Y que fueron sus enseñanzas las que me llevaron a viajar a tierras tan lejanas, Teniendo la dignidad y el coraje para luchar por los más necesitados. Y por eso siempre seguiré cantando con ustedes, Aje Vicente, toca la caja y llama a la gente, Aje Vicente, toca la caja y llama a la gente, Aje Vicente, toca la caja y llama la gente. Toca el tambor, llama a la gente, Toca la caja, llama a la gente, Toca el acordeón, llama a la gente... 3 ACKNOWLEDGMENTS I want to recognize the great dedication and guidance of my advisor, Philip Williams, since the first moment that I communicated to him my decision to pursue doctoral studies at the University of Florida. Without his encouragement, I would have never been able to complete this dissertation. I also want to recognize the four members of my dissertation committee: Ido Oren, Margareth Kohn, Katrina Schwartz, and Anthony Oliver-Smith. -

Issues Related to the Naso People 30
Report No. 56565-PA Public Disclosure Authorized Public Disclosure Authorized Investigation Report Panama: Land Administration Project Public Disclosure Authorized (Loan No. 7045-PAN) September 16, 2010 Public Disclosure Authorized About the Panel The Inspection Panel was created in September 1993 by the Board of Executive Directors of the World Bank to serve as an independent mechanism to ensure accountability in Bank operations with respect to its policies and procedures. The Inspection Panel is an instrument for groups of two or more private citizens who believe that they or their interests have been or could be harmed by Bank-financed activities to present their concerns through a Request for Inspection. In short, the Panel provides a link between the Bank and the people who are likely to be affected by the projects it finances. Members of the Panel are selected “on the basis of their ability to deal thoroughly and fairly with the request brought to them, their integrity and their independence from the Bank’s Management, and their exposure to developmental issues and to living conditions in developing countries.”1 The three-member Panel is empowered, subject to Board approval, to investigate problems that are alleged to have arisen as a result of the Bank having failed to comply with its own operating policies and procedures. Processing Requests After the Panel receives a Request for Inspection it is processed as follows: • The Panel decides whether the Request is prima facie not barred from Panel consideration. • The Panel registers the Request—a purely administrative procedure. • The Panel sends the Request to Bank Management, which has 21 working days to respond to the allegations of the Requesters. -

Hombres Mujeres Hombres Mujeres Hombres Mujeres
REPÚBLICA DE PANAMÁ MINISTERIO DE DESARROLLO SOCIAL INVERSIÓN EN TRANSFERENCIA MONETARIA CONDICIONADA Y BENEFICIARIOS PROGRAMA B/.120.00 A LOS 65, EN EL PAÍS, SEGÚN PROVINCIAS, COMARCAS Y CORREGIMIENTOS : TERCER TRIMESTRE 2020 Inversión en Balboas Beneficiarios en Números Modalidad Planilla Pagada Planilla Cobraron Provincia Distrito Corregimiento de Pago Monto Hombres Mujeres Monto Hombres Mujeres Cantidad Hombres Mujeres Cantidad Hombres Mujeres Total Monto Monto Total Monto Monto Total Cantidad Cantidad Total Cantidad Cantidad 45.746.640 18.321.840 27.424.800 125.574 50.331 75.243 BOCAS DEL TORO ALMIRANTE ALMIRANTE TCS 134.280 50.040 84.240 369 137 232 BOCAS DEL TORO ALMIRANTE NANCE DEL RISCO TCS 720 720 1 1 0 BOCAS DEL TORO ALMIRANTE VALLE DE AGUA ARRIBA TCS 360 360 1 1 0 BOCAS DEL TORO ALMIRANTE VALLE DEL RISCO TCS 54.000 23.400 30.600 147 64 83 BOCAS DEL TORO BOCAS DEL TORO BASTIMENTOS TCS 13.320 7.200 6.120 36 20 16 BOCAS DEL TORO BOCAS DEL TORO BOCAS DEL TORO TCS 42.840 21.960 20.880 118 61 57 BOCAS DEL TORO BOCAS DEL TORO CAUCHERO TCS 33.120 17.640 15.480 92 49 43 BOCAS DEL TORO BOCAS DEL TORO PUNTA LAUREL TCS 14.760 9.720 5.040 41 27 14 BOCAS DEL TORO BOCAS DEL TORO TIERRA OSCURA TCS 24.480 12.960 11.520 67 35 32 BOCAS DEL TORO CHANGUINOLA BARRIADA 4 DE ABRIL TCS 720 720 1 1 BOCAS DEL TORO CHANGUINOLA CHANGUINOLA TCS 173.880 61.920 111.960 477 169 308 BOCAS DEL TORO CHANGUINOLA COCHIGRÓ TCS 1.080 360 720 3 1 2 BOCAS DEL TORO CHANGUINOLA EL EMPALME TCS 125.280 42.840 82.440 347 118 229 BOCAS DEL TORO CHANGUINOLA GUABITO TCS 55.080