Epiretinal Membrane & Vitreomacular Traction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Challenges in Ophthalmic Pathology: the Vitreoretinal Membrane Biopsy
Challenges in PAUL HISCOTT, DAVID WONG, IAN GRIERSON ophthalmic pathology: The vitreoretinal membrane biopsy Abstract detachment.s Sheets or strands crossing the vitreous are sometimes called transvitreous The introduction of vitreoretinal microsurgery membranes. Anteriorly, membranes can arise has produced a new type of biopsy; that of the in, or be continuous with, the vitreous base and vitreoretinal membrane. This review even extend as far as the posterior iris surface or investigates methods by which these scar-like pupil. tissues are handled in the laboratory and Biopsies of pathological tissue are usually explores the implications of the results of such undertaken to establish a diagnosis. evaluations. The study of vitreoretinal Vitreoretinal biopsies also may be for diagnostic membrane biopsies has provided much purposes as, for example, in the case of information concerning the pathobiology of intraocular lymphoma, but such conditions are the various conditions which may give rise to rare and tend not to produce membranes. the tissue as well as insights into how Conversely, in the conditions which do produce membranes themselves develop. Moreover, membranes the diagnosis is seldom in doubt. the application of new laboratory techniques Why, then, attempt laboratory studies of is expected to enhance our understanding of vitreoretinal membranes? Laboratory findings the formation of vitreoretinal membranes, and from the membranes may have a number of lead to further advances in their surgical and uses, for example providing 'feed-back' to the medical management. surgeon concerning surgical dissection planes Key words Age-related macular degeneration, (see below). However, the principal objective of Epiretinal membrane, Proliferative diabetic these investigations is to improve our retinopathy, Proliferative vitreoretinopathy, understanding of the pathogenesis of P Hiscott D. -

SHOULD YOU OPEN a DRY-EYE CLINIC? Experts Help You Weigh the Pros and Cons
RETINAL PHOTOS ON THE GO P. 16 • CHANGES TO MEDICARE ABN FORMS P. 20 ENSURING A HAPPY CATARACT PATIENT P. 22 • MANAGING GLAUCOMA IN KPRO PATIENTS P. 58 THE CURRENT STATE OF VITREORETINAL EDUCATION P. 64 • WILLS EYE RESIDENT CASE REPORT P. 70 September 2020 reviewofophthalmology.com SHOULD YOU OPEN A DRY-EYE CLINIC? Experts help you weigh the pros and cons. P. 28 ALSO INSIDE: • The Latest Treatments for Dry Eye P. 38 • Comprehensive Ophthalmologists and Anti-VEGF Injections P. 48 • How to Manage Ocular Herpes P. 54 SHE MAY NEED MORE THAN ARTIFICIAL TEARS TO DISRUPT INFLAMMATION IN DRY EYE DISEASE1,2 Her eyes deserve a change. Choose twice-daily Xiidra for lasting relief that can start as early as 2 weeks.3*† Not an actual patient. *In some patients with continued daily use. One drop in each eye, twice daily (approximately 12 hours apart).3 †XiidraisanLFA-1antagonistforthetreatmentofdryeyedisease.Pivotaltrialdata:ThesafetyandefficacyofXiidrawereassessedinfour Important Safety Information (cont) 12-week,randomized,multicenter,double-masked,vehicle-controlledstudies(N=2133).Patientsweredosedtwicedaily.Useofartificial • I n clinicaltrials,themostcommonadversereactionsreportedin5-25%ofpatientswereinstillationsite tearswasnotallowedduringthestudies.Thestudyendpointsincludedassessmentofsigns(basedonInferiorfluoresceinCornealStaining irritation,dysgeusiaandreducedvisualacuity.Otheradversereactionsreportedin1%to5%ofthepatients Score [ICSS] on a scale of 0 to 4) and symptoms (based on patient-reported Eye Dryness Score [EDS] on a visual analogue scale of 0 to 100).3 were blurred vision, conjunctival hyperemia, eye irritation, headache, increased lacrimation, eye discharge, A larger reduction in EDS favoring Xiidra was observed in all studies at day 42 and day 84. Xiidra reduced symptoms of eye dryness at eye discomfort, eye pruritus and sinusitis. 2 weeks (based on EDS) compared to vehicle in 2 out of 4 clinical trials. -

Exploring Topical Anti-Glaucoma Medication Effects on the Ocular Surface in the Context of the Current Understanding of Dry Eye
The Ocular Surface 16 (2018) 289e293 Contents lists available at ScienceDirect The Ocular Surface journal homepage: www.theocularsurface.com Original Research Exploring topical anti-glaucoma medication effects on the ocular surface in the context of the current understanding of dry eye Aaron B.C. Wong, Michael T.M. Wang, Kevin Liu, Zak J. Prime, Helen V. Danesh-Meyer, * Jennifer P. Craig Department of Ophthalmology, New Zealand National Eye Centre, The University of Auckland, New Zealand article info abstract Article history: Purpose: To assess tear film parameters, ocular surface characteristics, and dry eye symptomology in Received 11 November 2017 patients receiving topical anti-glaucoma medications. Received in revised form Methods: Thirty-three patients with a diagnosis of open angle glaucoma or ocular hypertension, 26 February 2018 receiving unilateral topical anti-glaucoma medication for at least 6 months, were recruited in a cross- Accepted 2 March 2018 sectional, investigator-masked, paired-eye comparison study. Tear film parameters, ocular surface characteristics, and dry eye symptomology of treated and fellow eyes were evaluated and compared. Keywords: Results: The mean ± SD age of the participants was 67 ± 12 years, and the mean ± SD treatment duration Glaucoma ± fi ¼ fi Prostaglandin analogue was 5.3 4.4 years. Treated eyes had poorer non-invasive tear lm breakup time (p 0.03), tear lm ¼ ¼ Tear film osmolarity (p 0.04), bulbar conjunctival hyperaemia (p 0.04), eyelid margin abnormality grade Ocular surface (p ¼ 0.01), tear meniscus height (p ¼ 0.03), and anaesthetised Schirmer value (p ¼ 0.04) than fellow eyes. Dry eye There were no significant differences in dry eye symptomology, meibomian gland assessments, and Meibomian gland ocular surface staining between treated and fellow eyes (all p > 0.05). -

Bilateral VMT Case Outline (Formatted).Pages
Abstract! Vitreomacular traction (VMT) is defined as partial posterior vitreous detachment with persistent macular attachment and subsequent foveal distortion, as visualized through macular optical coherence tomography. We report a rare case of bilateral simultaneous VMT. I. Case History! !•! 65 year old African American male !•! Presenting for follow-up examination for glaucoma testing including OCT of the RNFL and GCC. ! •! No other visual complaints !•! Identified as a glaucoma suspect in 2004; no other ocular history. !•! Medical history significant for non-insulin dependent type II diabetes mellitus, hypertension, hypercholesterolemia !•! Medications: Metformin, Enalapril, Crestor !•! Strong family history of open angle glaucoma including mother, brother, and sister. II. Pertinent findings! !•! BCVA: 20/20 OD, 20/25 OS !•! IOP: 19mmHg OU (Goldmann @ 14:51) !•! C/D: 0.75V/0.65V OD, 0.8V/0.7H OS !•! Macula: flat, even pigment !•! OCT retinal analysis: Bilateral loss of normal foveal architecture with cystic changes in the outer plexiform layer. Residual adhesion between the posterior hyaloid and internal limiting membrane is apparent. Modest increase in full-retinal thickness at the centre of the macula. III. Differential diagnosis! !•! Vitreomacular Adhesion (VMA) !•! Vitreomacular Traction (VMT) !•! Tractional Diabetic Macular Edema (DME) IV. Diagnosis and discussion! !•! Most definitive diagnosis: focal isolated VMT ! •! Clear partial posterior vitreous detachment with focal attachment at the macula resulting in distortion of the foveal contour. ! •! Adhesion extent can be measured with the OCT caliper function. ! •! Distortion of the foveal pit with separation of the retinal layers at the level of the outer plexiform layer. !•! Tractional Diabetic Macular Edema: Ruled out due to absence of co-existing diabetic retinopathy or other signs of DME. -

Macular Hole Formation Following Choroidal Neovascularization
Yoshida et al., Int J Ophthalmol Clin Res 2015, 2:1 International Journal of ISSN: 2378-346X Ophthalmology and Clinical Research Case Report: Open Access Macular Hole Formation Following Choroidal Neovascularization Treatment in A High Myopic Eye with Epiretinal Membrane Yusaku Yoshida*, Manabu Yamamoto, Takeya Kohno and Kunihiko Shiraki Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, Japan *Corresponding author: Yusaku Yoshida, MD, Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan, Fax:+81-666-343- 873, E-mail: [email protected] macular hole development where post-treatment regression of CNV Abstract seemed to have played a major role in a high myopic eye with ERM. Purpose: To report on the development of macular hole after treatment of choroidal neovascularization (CNV) in a patient with Case high myopia and epiretinal membrane (ERM). A 60-year-old man was examined in the Department of Methods: Retrospective single case report. Ophthalmology of Osaka City University Hospital for reduced vision Patients: A 60-year-old man presented with reduced vision in his in his right eye in January 2009. On initial examination, decimal best- right eye. On the initial examination, the right eye was high myopic corrected visual acuity (BCVA) was 0.3 in the right eye and 1.5 in with decimal best-corrected visual acuity (BCVA) of 0.3. the left eye, while intraocular pressures were 13 and 14 mmHg in the right and left eye, respectively. His previous medical and family Results: A subretinal grayish-white lesion was seen at the macula with hemorrhage, and optical coherence tomography showed a histories included nothing of note. -

Floaters-Survey-Ophthalmol-2016.Pdf
survey of ophthalmology 61 (2016) 211e227 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/survophthal Major review Vitreous floaters: Etiology, diagnostics, and management Rebecca Milston, MOptoma, Michele C. Madigan, PhDb,c, J. Sebag, MD, FACS, FRCOphth, FARVOd,* a Centre for Eye Health, University of New South Wales, Sydney, New South Wales, Australia b School of Optometry and Vision Science, University of New South Wales, Sydney, New South Wales, Australia c Save Sight Institute and Discipline of Clinical Ophthalmology, Sydney Medical School, University of Sydney, New South Wales, Australia d VMR Institute for Vitreous Macula Retina, Huntington Beach, California, USA article info abstract Article history: Vitreous is a hydrated extracellular matrix comprised primarily of water, collagens, and Received 3 July 2015 hyaluronan organized into a homogeneously transparent gel. Gel liquefaction results from Received in revised form 25 molecular alterations with dissociation of collagen from hyaluronan and aggregation of November 2015 collagen fibrils forming fibers that cause light scattering and hence symptomatic floaters, Accepted 25 November 2015 especially in myopia. With aging, gel liquefaction and weakened vitreoretinal adhesion Available online 8 December 2015 result in posterior vitreous detachment, the most common cause of primary symptomatic floaters arising from the dense collagen matrix of the posterior vitreous cortex. Recent Keywords: studies indicate that symptomatic floaters are not only more prevalent, but also have a vitreous negative impact on the quality of life that is greater than previously appreciated. We review collagen the literature concerning management of symptomatic vitreous floaters, currently either myopia with observation, vitrectomy, or Nd:YAG laser. -
Epiretinal Membrane
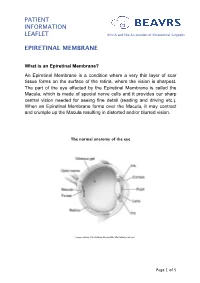
PATIENT INFORMATION LEAFLET British and Eire Association of Vitreoretinal Surgeons EPIRETINAL MEMBRANE What is an Epiretinal Membrane? An Epiretinal Membrane is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the Macula, which is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). When an Epiretinal Membrane forms over the Macula, it may contract and crumple up the Macula resulting in distorted and/or blurred vision. The normal anatomy of the eye *Image courtesy of the National Eye Institute http://www.nei.nih.gov Page 1 of 5 PATIENT INFORMATION British and Eire Association of Vitreoretinal Surgeons LEAFLET EPIRETINAL MEMBRANE Why do I have an Epiretinal Membrane? In most cases the development of an Epiretinal Membrane appears to be related to normal aging changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal surgery. Epiretinal membranes are not related to Macular Degeneration. Epiretinal Membranes do not usually affect the other eye. They are quite common and affect up to 8% of people in later years. Cross-section of a healthy macula Cross-section of a macula with an epiretinal membrane Assessment for Epiretinal Membrane Your eye doctor is able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. -

Posterior Segment Retina
Carpineto_A4_2011 28/06/2011 16:50 Page 69 Posterior Segment Retina Diagnosing and Treating Vitreomacular Adhesion Paolo Carpineto,1 Luca Di Antonio,2 Agbeanda Aharrh-Gnama,2 Vincenzo Ciciarelli3 and Leonardo Mastropasqua4 1. Associate Professor; 2. Doctor of Philosophy; 3. Resident; 4. Professor and Chair, Ophthalmology Clinic, Department of Medicine and Aging Sciences, University G d’Annunzio Chieti-Pescara Abstract Perifoveal vitreous detachment with residual vitreofoveal adhesion is considered as the first stage of posterior vitreous detachment. A key point is the transition from an innocuous vitreomacular adhesion (VMA) to a pathological vitreomacular traction (VMT). By using optical coherence tomography (OCT), VMA is defined as adhesion of the posterior hyaloid cortex involving the centre of the foveal region with or without a hyper-reflective signal on the inner surface of the retina. VMT is diagnosed when the inner macular surface slopes steeply, or sharp angulation and localised deformation of the retinal profile is detected at the VMA site. Otherwise, VMA is simply considered to be persistent adherence of the cortical vitreous. The tractional effects of perifoveal vitreous detachment cause a variety of macular pathologies determined by the size and the strength of the residual vitreoretinal adhesion. Vitreomacular adhesion plays a major role in the development of diseases such as vitreomacular traction syndrome (VMTS), macular hole, epiretinal membrane, tractional macular oedema and myopic macular retinoschisis. In addition, clinical evidence supports the theory that the course of diabetic retinopathy and age-related macular degeneration may be strongly influenced by an incomplete posterior vitreous separation. The current standard of care of vitreomacular interface pathologies is vitrectomy and membrane peeling – a procedure that is thought to relieve epiretinal traction – followed by regeneration of the retinal architecture and recovery of visual function. -

Home>>Common Retinal & Ophthalmic Disorders
Common Retinal & Ophthalmic Disorders Cataract Central Serous Retinopathy Cystoid Macular Edema (Retinal Swelling) Diabetic Retinopathy Floaters Glaucoma Macular degeneration Macular Hole Macular Pucker - Epiretinal Membrane Neovascular Glaucoma Nevi and Pigmented Lesions of the Choroid Posterior Vitreous Detachment Proliferative Vitreoretinopathy (PVR) Retinal Tear and Detachment Retinal Artery and Vein Occlusion Retinitis Uveitis (Ocular Inflammation) White Dot Syndromes Anatomy and Function of the Eye (Short course in physiology of vision) Cataract Overview Any lack of clarity in the natural lens of the eye is called a cataract. In time, all of us develop cataracts. One experiences blurred vision in one or both eyes – and this cloudiness cannot be corrected with glasses or contact lens. Cataracts are frequent in seniors and can variably disturb reading and driving. Figure 1: Mature cataract: complete opacification of the lens. Cause Most cataracts are age-related. Diabetes is the most common predisposing condition. Excessive sun exposure also contributes to lens opacity. Less frequent causes include trauma, drugs (eg, systemic steroids), birth defects, neonatal infection and genetic/metabolic abnormalities. Natural History Age-related cataracts generally progress slowly. There is no known eye-drop, vitamin or drug to retard or reverse the condition. Treatment Surgery is the only option. Eye surgeons will perform cataract extraction when there is a functional deficit – some impairment of lifestyle of concern to the patient. Central Serous Retinopathy (CSR) Overview Central serous retinopathy is a condition in which a blister of clear fluid collects beneath the macula to cause acute visual blurring and distortion (Figure 2). Central serous retinochoroidopathy Left: Accumulation of clear fluid beneath the retina. -
Retinal Conditions
GENERAL INFORMATION RETINAL CONDITIONS RETINAL CONDITIONS WHAT ARE RETINAL CONDITIONS? Retinal conditions affect the light-sensitive tissue at the back of eye known as the retina. They include diseases that affect the part of the retina responsible for central vision (the macula) and the jelly-like fluid that sits in front of the retina (the vitreous). The retina acts like the ‘film’ of a camera, sending information about shapes, colours, patterns and movement via the optic nerve to the brain, where the information is processed into the final image that we see. DAMAGE TO THE RETINA CAUSES VISUAL DISTURBANCES OR LOSS OF VISION. RETINAL CONDITIONS 2 RETINAL CONDITIONS The main conditions that affect the retina are: Macular degeneration: A group of degenerative diseases of the macula that cause loss of central and fine-detail vision. Treatment to stop or slow the progression of the wet form includes eye injections and photodynamic therapy. Unfortunately, there is no approved treatment for the dry form. Diabetic retinopathy: An eye disease caused by the persistently high blood sugar levels that occur with diabetes. Depending on the stage of disease, treatment includes eye injections, retinal laser treatment and vitrectomy surgery (keyhole surgery to remove the vitreous). The most advanced stage of the disease is an ocular emergency that can cause total vision loss. Retinal vein occlusion: Vision loss that occurs when the veins in the retina are blocked and the build-up of pressure causes smaller downstream blood vessels to leak. The blockage can occur in a branch vein with vision loss restricted to part of the visual field (branch vein retinal occlusion) or a central vein with the entire visual field affected (central vein retinal occlusion). -

Vitreomacular Traction Syndrome - to Treat Or Not to Treat
Vitreomacular Traction Syndrome - To treat or not to treat... That is the question. 82-year old male has decreased acuity OD with current VMT/macular hole stage 1a. Patient history of CME vs. Irvine-Gass/VMT macular hole stage 1a OS resolving spontaneously. Treat or observe the right eye and why? Case History: 82 year old Caucasian male currently presents for decreased visual acuity at a 3 month follow up for VMT/macular hole stage 1a OD. The patient has a history of focal VMT/CME vs. Irvine-Gass syndrome/macular hole stage 1a OS 2 month post- op cataract surgery in early 2014. This VMT/macular hole stage 1 spontaneously released to a lamellar hole with a non-full thickness traction aperture of 219 um. Patient has a history of focal vitreomacular adhesion OD 1 month post-op cataract surgery OD in early 2014. The patient’s OD focal VMA turned to focal VMT and is currently at focal VMT/macular hole 1a with symptomatic visual acuity decrease and minor metamorphopsia. The patient’s OS spontaneously resolved after the posterior hyaloid membrane released in late 2014. Ocular/medical Hx: 1. Disorder of voice 2. Sensorineural hearing loss, bilateral 3. Macular Pucker/Epiretinal Membrane (Erm) 4. Pseudophakia CE OS 1/21/14 CE OD 2/11/14 5. RENAL INSUFFCIENCY 6. Coronary Artery Disease 7. Asthenopia 8. Headache 9. Presbyopia 10. HYPERTENSION NOS 11. LUMBAGO 12. HYPERLIPIDEMIA NEC/NOS 13. Presbylarynges 14. DEPRESSIVE DISORDER NEC Allergies: ZOCOR, ATORVASTATIN, NIASPAN 1000MG ER TABLET, PRAVASTATIN, OMEPRAZOLE RABEPRAZOLE, GEMFIBROZIL, PANTOPRAZOLE, LISINOPRIL, ALFUZOSIN Medications: Aspirin, Hydroxyzine, Lansopranzole, Losartan, Lovastatin, Nitroglycerine, Ranitidine, Tramadole, Diazepam, Polyvinyl alcohol Pertinent Findings: The patient currently has decreased vision OD for the last 6 months, with reports of minor metamorphopsia that has not changed in the last 3 months. -

Keratoconus and Cone-Rod Dystrophy Among Brothers: Clinical Case Study and Genetic Analysis
Trends in Ophthalmology Open Access Journal DOI: 10.32474/TOOAJ.2019.02.000133 ISSN: 2644-1209 Case Report Keratoconus and Cone-Rod Dystrophy among Brothers: Clinical Case Study and Genetic Analysis Victoria Dimacali1*, Spyridon Koronis1, Stavrenia Koukoula1, Achilleas Rasoglou2, Aspasia Adamopoulou1, Elissavet Siskou3 and Miltos Balidis1 1Ophthalmica Institute of Ophthalmology and Microsurgery, Greece 2Department of Ophthalmology, General Hospital of Edessa, Greece 3Department of Ophthalmology, Papanikolaou General Hospital, Greece *Corresponding author: Victoria Dimacali, Ophthalmica Institute of Ophthalmology and Microsurgery, Thessaloniki, Greece Received: March 25, 2019 Published: April 01, 2019 Abstract Background: Advances in genomics continue to enable the discovery of gene variants which cause various inherited ophthalmic disorders. Several case reports have shown an association between keratoconus and retinal disease but whether there is a genetic basis for this is still not known. Methods: Clinical case study with Pentacam imaging, fundus autofluorescence (FAF), macular optical coherence tomography (OCT),Results: electrophysiology We report three studies, brothers, and genetic two of whomanalysis. have keratoconus and one who was found to have bilateral cone-rod dystrophy. MAP3K19, ADGRV1, and PIK3CG This was supported by color vision and electrophysiology testing, fundus autofluorescence,CHST6 gene in and the macular latter. Whole OCT exomefindings. sequencing Genomic data revealedanalysis revealeda rare missense three rare variant gene for variants IMPG2 ( gene in both brothers. ) common to the brother with cone-rod dystrophy and one brother with keratoconus. There was also a very significant variant in the Conclusion: Among the four genes with shared mutations in two of the brothers, IMPG2 has been linked to retinal disease while MAP3K19 and PIK3CG carry high risk scores for keratoconus pathogenesis.