Ketamine: What's Old Is New Again
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ketamine As a Rapid Antidepressant
BJPsych Advances (2016), vol. 22, 222–233 doi: 10.1192/apt.bp.114.014274 ARTICLE Ketamine as a rapid anti depressant: the debate and implications Roger C. M. Ho & Melvyn W. Zhang Roger Ho is an Associate Professor response rates to SSRIs and NaSSAs are around SUMMARY and consultant psychiatrist in 62% and 67% respectively (Papakostas 2008). the Department of Psychological Ketamine, a synthetic derivative of phencyclidine, Environmental factors such as relationship Medicine, Yong Loo Lin School of is a commonly misused party drug that is Medicine, National University of problems, financial difficulties and comorbid restricted in high-income countries because of Singapore. He has a special interest substance misuse often lead to poor treatment its addictive potential. Ketamine is also used as in psychoneuroimmunology and response, and antidepressants combined with the interface between medicine an anaesthetic in human and veterinary medicine. and psychiatry. Melvyn Zhang In the 1990s, research using ketamine to study the CBT have shown promising results in prevention is a senior resident with the pathophysiology of schizophrenia was terminated of mood disorders (Brenner 2010). Although 70– National Addiction Management owing to ethical concerns. Recently, controversy 90% of patients with depression achieve remission, Service, Institute of Mental Health, surrounding the drug has returned, as researchers around 10–30% are refractory to initial treatment Singapore. Correspondence Dr Roger C. M. have demonstrated that intravenous ketamine but respond to switching or combination of Ho, National University of Singapore, infusion has a rapid antidepressant effect and antidepressants, electroconvulsive therapy (ECT) Department of Psychological have therefore proposed ketamine as a novel or psychotherapy. -
Predicting Intestinal and Hepatic First-Pass Metabolism of Orally Administered Testosterone Undecanoate
applied sciences Article Predicting Intestinal and Hepatic First-Pass Metabolism of Orally Administered Testosterone Undecanoate Atheer Zgair 1,2,* , Yousaf Dawood 1, Suhaib M. Ibrahem 1, Hyun-moon Back 3, Leonid Kagan 3, Pavel Gershkovich 2 and Jong Bong Lee 2 1 College of Pharmacy, University of Anbar, Ramadi 31001, Iraq; [email protected] (Y.D.); [email protected] (S.M.I.) 2 School of Pharmacy, University of Nottingham, Nottingham NG7 2RD, UK; [email protected] (P.G.); [email protected] (J.B.L.) 3 Ernest Mario School of Pharmacy, Rutgers, The State University of New Jersey, Piscataway, NJ 08854, USA; [email protected] (H.-m.B.); [email protected] (L.K.) * Correspondence: [email protected]; Tel.: +964-(0)-781-777-1463 Received: 2 October 2020; Accepted: 15 October 2020; Published: 18 October 2020 Abstract: The bioavailability of orally administered drugs could be impacted by intestinal and hepatic first-pass metabolism. Testosterone undecanoate (TU), an orally administered ester prodrug of testosterone, is significantly subjected to first-pass metabolism. However, the individual contribution of intestinal and hepatic first-pass metabolism is not well determined. Therefore, the aim of the current study was to predict the metabolic contribution of each site. The hydrolysis–time profiles of TU incubation in human liver microsomes and Caco-2 cell homogenate were used to predict hepatic and intestinal first-pass metabolism, respectively. The in vitro half-life (t1/2 inv) for the hydrolysis of TU in microsomal mixtures was 28.31 3.51 min. By applying the “well-stirred” model, the fraction ± of TU that could escape hepatic first-pass metabolism (F ) was predicted as 0.915 0.009. -

PHARMACY of the MONTH Discovery Pharmacy, Volume 3, Number 7, January 2013 PHARMACY of the MONTH 18 54 – EISSN 2278 26 54 – Pharmacy
PHARMACY OF THE MONTH Discovery Pharmacy, Volume 3, Number 7, January 2013 PHARMACY OF THE MONTH 18 54 – EISSN 2278 26 54 – Pharmacy ISSN 2278 Intra- and Inter-Subject Variation in the Pharmacokinetics of Some Drugs- A Review Balasubramanian J1,2&4*, Tamil selvan2 1. Shield Health Care Pvt Ltd, Chennai-600 095, India 2. Sai Bio – Sciences Pvt Ltd, Chennai-600 094, India 3. Periyar Maniammai University, Thanjavur-613 403, Tamilnadu, India *Corresponding author: E-mail: [email protected] Received 24 November; accepted 21 December; published online 01 January; printed 16 January 2013 1. INTRODUCTION "Inter-individual variations of drugs pharmacokinetic parameters, resulting in fairly different plasma concentration-time profiles after administration of the same dose to different patients." Substantial differences in response to most drugs exist among patients. Therefore, the therapeutic standard dose of a drug, which is based on trails in healthy volunteers and patients, is not suitable for every patient. Variability exists in both pharmacokinetics and pharmacodynamics. For a typical drug, one standard deviation in the values observed for bioavailability (F), clearance (CL) and volume of distribution (Vd) would be about 20%, 50% and 30% respectively. Therefore, 95% of the time, the average concentration (Cav) will be between 35% and 270% of the target value. The most important factors in variability of pharmacokinetic parameters are: Genetic, Disease, Age and body size, Concomitant drugs, Environmental factors (e.g. foods, pollutants) and other factors include compliance, pregnancy, alcohol intake, seasonal variations, gender, or conditions of drug intake. 1.1. Genetic Patients vary widely in their responses to drugs. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine -

Pharmacokinetic Considerations and Recommendations in Palliative Care, with Focus on Morphine, Midazolam and Haloperidol
Expert Opinion on Drug Metabolism & Toxicology ISSN: 1742-5255 (Print) 1744-7607 (Online) Journal homepage: http://www.tandfonline.com/loi/iemt20 Pharmacokinetic considerations and recommendations in palliative care, with focus on morphine, midazolam and haloperidol L. G. Franken, B. C. M de Winter, H. J. van Esch, L. van Zuylen, F. P. M. Baar, D. Tibboel, R. A. A. Mathôt, T. van Gelder & B. C. P. Koch To cite this article: L. G. Franken, B. C. M de Winter, H. J. van Esch, L. van Zuylen, F. P. M. Baar, D. Tibboel, R. A. A. Mathôt, T. van Gelder & B. C. P. Koch (2016) Pharmacokinetic considerations and recommendations in palliative care, with focus on morphine, midazolam and haloperidol, Expert Opinion on Drug Metabolism & Toxicology, 12:6, 669-680, DOI: 10.1080/17425255.2016.1179281 To link to this article: https://doi.org/10.1080/17425255.2016.1179281 © 2016 The Author(s). Published by Informa Accepted author version posted online: 15 UK Limited, trading as Taylor & Francis Apr 2016. Group. Published online: 29 Apr 2016. Submit your article to this journal Article views: 918 View related articles View Crossmark data Citing articles: 6 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=iemt20 EXPERT OPINION ON DRUG METABOLISM & TOXICOLOGY, 2016 VOL. 12, NO. 6, 669–680 http://dx.doi.org/10.1080/17425255.2016.1179281 REVIEW Pharmacokinetic considerations and recommendations in palliative care, with focus on morphine, midazolam and haloperidol L. G. Frankena, B. C. M de Wintera, H. -

Non-IV Sedation and the MKO Melt Maggie Jeffries, MD and Chris Bender, CRNA Why Is the Type of Anesthesia Important?
Non-IV Sedation And the MKO Melt Maggie Jeffries, MD and Chris Bender, CRNA Why is the type of anesthesia important? Cataract surgery is the most common procedure performed by Ophthalmologists, the most commonly performed surgical procedure in the US Medicare population and the number one cause of blindness worldwide.1, 2 Eye surgery represents 4-5% of all surgical anesthesia claims in the Anesthesia Closed Claims Project database. Of the cases involving movement, 33% were under monitored anesthesia care, 59% under general anesthesia and 9% received a block. Vision loss accounted for 97% of all claims associated with movement during the procedure.3 A 2006 closed claim analysis of monitored anesthesia care cases found that 21% were undergoing elective eye surgery and of these, respiratory depression (21%) was the most common mechanism of injury.4 Why sedation without an IV? Older patient population with more difficult IV placement Patient anxiety related to getting the IV and many complaints are related to the IV. When given a choice, patients would choose oral sedation over IV sedation 5 The IV contributes to pre-op time and potentially delays and decreased efficiency Risk is minimal with IV but that risk eliminated by going IV free Sublingual route for medication administration Dysphagia and malabsorption are prevalent with advance age - sublingual route bypasses the need for swallowing and gastric absorption Bypasses the hepatic first pass effect with the result being bioavailability as much as 3-10 times greater when compared to oral -

Pharmacokinetics of Hard Micronized Progesterone Capsules Via Vaginal
Drug Design, Development and Therapy Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Pharmacokinetics of hard micronized progesterone capsules via vaginal or oral route compared with soft micronized capsules in healthy postmenopausal women: a randomized open-label clinical study This article was published in the following Dove Press journal: Drug Design, Development and Therapy Hanbi Wang,1 Meizhi Liu,1 Purpose: This study aimed to evaluate the pharmacokinetics of hard micronized progester- Qiang Fu,2 Chengyan Deng1 one capsules (Yimaxin) via the vaginal or oral route compared with soft micronized progesterone capsules (Utrogestan) in a Chinese population. 1Reproductive Center, Department of Obstetrics and Gynecology, Peking Union Methods: A prospective single-center randomized open-label trial was conducted in 16 healthy Medical College Hospital, Chinese postmenopausal women. They were randomized into two groups to receive four phases of treat- Academy of Medical Sciences, Beijing, ment: vaginal Yimaxin, vaginal Utrogestan, oral Yimaxin, or oral Utrogestan, with different People’s Republic of China; 2Department of Pharmacy, Peking Union Medical sequences. College Hospital, Chinese Academy of Results: By the vaginal route, steady-state maximum concentration (Cmax) of Yimaxin and Medical Sciences, Beijing, People’s Republic of China Utrogestan was 29.13±8.09 and 12.30±1.60 mg/L, time to Cmax 9.72±10.50 and 11.03±9.62 hours, central compartment volume of distribution 4.26±1.86 and 10.40±2.32 L, clearance rate 0.18±0.05 and 0.38±0.10 L/h, and AUC 261.42±74.36 and 116.83±19.72 h·ng/mL, respectively. -

ROZEREM Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION • Reproductive effects: Include decreased testosterone and increased These highlights do not include all the information needed to use prolactin levels. Effect on reproductive axis in developing humans is ROZEREM safely and effectively. See full prescribing information for unknown. (5.5) ROZEREM. • Patients with severe sleep apnea: ROZEREM is not recommended for use in this population. (5.6) ROZEREM (ramelteon) tablets, for oral use Initial U.S. Approval: 2005 --------------------------------ADVERSE REACTIONS------------------------------ Most common adverse reactions (≥3% and more common than with --------------------------INDICATIONS AND USAGE------------------------------- placebo) are: somnolence, dizziness, fatigue, nausea, and exacerbated ROZEREM is indicated for the treatment of insomnia characterized by insomnia. (6.1) difficulty with sleep onset. (1) To report SUSPECTED ADVERSE REACTIONS, contact Takeda -----------------------DOSAGE AND ADMINISTRATION------------------------ Pharmaceuticals at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1- • Adult dose: 8 mg taken within 30 minutes of going to bed. (2.1) 800-FDA-1088 or www.fda.gov/medwatch. • Should not be taken with or immediately after a high-fat meal. (2.1) • Total daily dose should not exceed 8 mg. (2.1) --------------------------------DRUG INTERACTIONS-------------------------------- • Rifampin (strong CYP enzyme inducer): Decreases exposure to and ----------------------DOSAGE FORMS AND STRENGTHS---------------------- effects of ramelteon. -

Routes of Drug Administration, First-Pass Effect
Routes of drug administration, first-pass effect We usually divide routes of drug administration that produce systemic effect in Enteral or Parenteral. From Greek Enteros = Intestine and Para = Beside. Thus either it passes through the intestinal tract or it avoids it. This is extremely important as some drugs are poorly absorbed in the intestines, others are well absorbed however are metabolized almost completely by first-pass effect. Enteral Are entering the intestinal tract. Oral Given by mouth is the most common route of drug administration, however it also the one with the most complicated pathway to the target tissues. Most drugs are absorbed in the intestinal tract by passive transfer and usually end up in the portal circulation encountering the liver and thus high chance of passing the first-pass effect. Rectal Rectal administration can be used for producing local or systemic effects. It is quite unreliable however. 75% of drainage of the rectal region bypasses the portal circulation and thus minimizing first-pass effect. The inferior and middle rectal veins are linked to the systemic circulation whereas the superior rectal vein joins the inferior mesentering vein and from there onto the portal vein. It can be very useful during vomiting and in patients that are unable to take medications by mouth. Sublingual Sublingual administration can be classified into Parenteral as well, it does not enter the lower GastroIntestinal Tract, however it is placed under the tongue thus going oral. The drug diffuses into the capillary network and enters the system circulation directly. It is very rapidly absorbed, low infection risk, avoiding the rough environment of the GIT and no first-pass metabolism. -

Ep 2229936 B1
(19) TZZ ¥_T (11) EP 2 229 936 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/14 (2006.01) A61K 9/51 (2006.01) 06.05.2015 Bulletin 2015/19 A61K 9/107 (2006.01) A61K 9/48 (2006.01) A61K 31/568 (2006.01) (21) Application number: 09003370.5 (22) Date of filing: 09.03.2009 (54) Nanonized testosterone formulations for improved bioavailability Nanonisierte Testosteronformulierungen für verbesserte Bioverfügbarkeit Formules de testostérone de taille nano pour une meilleure biodisponibilité (84) Designated Contracting States: (74) Representative: UEXKÜLL & STOLBERG AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Patentanwälte HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL Beselerstrasse 4 PT RO SE SI SK TR 22607 Hamburg (DE) (43) Date of publication of application: (56) References cited: 22.09.2010 Bulletin 2010/38 EP-A- 1 698 329 WO-A-00/67728 WO-A-2007/103294 DE-A1- 19 825 856 (73) Proprietor: PharmaSol GmbH DE-A1- 19 932 157 US-A1- 2002 119 916 12307 Berlin (DE) US-B1- 6 814 959 (72) Inventors: • BAGCHUS W M ET AL: "IMPORTANT EFFECT OF • Keck, Cornelia FOOD ON THE BIOAVAILABILITY OF ORAL 12161 Berlin (DE) TESTOSTERONE UNDECANOATE" • Muchow, Marc PHARMACOTHERAPY, BOSTON, US, vol. 23, no. 67292 Kirchheimbolanden (DE) 3, 1 January 2003 (2003-01-01), pages 319-325, XP001147255 ISSN: 0277-0008 Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Principles of Pharmacology
© Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC manning/Shutterstock © Sofi NOT FOR SALE OR DISTRIBUTION NOT FOR2 SALE OR DISTRIBUTION Principles of Pharmacology © Jones & Bartlett Learning, LLC Laura Williford Owens,© Robin Jones Webb & Corbett, Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTIONTekoa L. King NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE✜ Chapter OR DISTRIBUTION Glossary NOT FOR SALE OR DISTRIBUTION exchange of drugs between the systemic circulation Absorption Movement of drug particles from the gastro- and the circulation in the central nervous system. intestinal tract to the systemic circulation by passive Chronobiology (chronopharmacology) Use of knowledge of cir- absorption, active transport, or pinocytosis. cadian rhythms to time administration of drugs for © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC Affinity Degree of attraction between a drug and a recep- maximum benefi t and minimal harm. tor. Th e greater NOTthe attraction, FOR SALE the greater OR DISTRIBUTIONthe extent Clearance Measure of the body’sNOT ability FOR to SALE eliminate OR a drug.DISTRIBUTION of binding. Competitive antagonist Drug or ligand that reversibly binds Agonist Drug that activates a receptor when bound to that to receptors at the same receptor site that agonists use receptor. (active site) without activating the receptor to initiate Agonist–antagonist© Jones & BartlettDrug that Learning,has agonist properties LLC for one a reaction.© Jones & Bartlett Learning, LLC NOTopioid FOR receptor SALE and antagonist OR DISTRIBUTION properties for a diff erent CytochromeNOT P-450 FOR (CYP450) SALE Generic OR name DISTRIBUTION for the family of type of opioid receptor. -
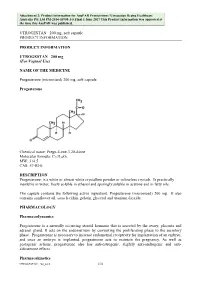
Attachment 2. Product Information for Progesterone
Attachment 2: Product information for AusPAR Prometrium / Utrogestan Besins Healthcare Australia Pty Ltd PM-2014-03908-1-5 Final 1 June 2017 This Product Information was approved at the time this AusPAR was published. UTROGESTAN 200 mg, soft capsule PRODUCT INFORMATION PRODUCT INFORMATION UTROGESTAN 200 mg (For Vaginal Use) NAME OF THE MEDICINE Progesterone (micronised) 200 mg, soft capsule Progesterone Chemical name: Pregn-4-ene-3,20-dione Molecular formula: C21H30O2. MW: 314.5 CAS: 57-83-0. DESCRIPTION Progesterone: is a white or almost white crystalline powder or colourless crystals. Is practically insoluble in water, freely soluble in ethanol and sparingly soluble in acetone and in fatty oils. The capsule contains the following active ingredient: Progesterone (micronised) 200 mg. It also contains sunflower oil, soya lecithin, gelatin, glycerol and titanium dioxide. PHARMACOLOGY Pharmacodynamics Progesterone is a naturally occurring steroid hormone that is secreted by the ovary, placenta and adrenal gland. It acts on the endometrium by converting the proliferating phase to the secretory phase. Progesterone is necessary to increase endometrial receptivity for implantation of an embryo, and once an embryo is implanted, progesterone acts to maintain the pregnancy. As well as gestagenic actions, progesterone also has anti-estrogenic, slightly anti-androgenic and anti- aldosterone effects. Pharmacokinetics UTROGESTAN 200_0416 1/10 Attachment 2: Product information for AusPAR Prometrium / Utrogestan Besins Healthcare Australia Pty Ltd PM-2014-03908-1-5 Final 1 June 2017 This Product Information was approved at the time this AusPAR was published. UTROGESTAN 200 mg, soft capsule PRODUCT INFORMATION Absorption Following oral administration, micronised progesterone is absorbed by the digestive tract.