Compression Hosiery in Lymphoedema
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Women's Hosiery
STUDIO N - FOR INTERNAL AND VENDOR USE ONLY ONLINE PHOTOGRAPHY GUIDE - Womens_Hosiery 1. TABLE OF CONTENTS 2. Hosiery Leggings 3. Sheer, Textured & Thigh high Hosiery 4. Shaper Hosiery 5. Sweater Tights 6. Over the Knee Socks, Leg Warmers & Trendy Thigh Highs - onfig 7. Socks: Knee-hi / no-show / ankle / -onfig 8. Socks: Womens sock sets / boot liners –product 9. Socks: Nike Elite 1 STUDIO N - FOR INTERNAL AND VENDOR USE ONLY ONLINE PHOTOGRAPHY GUIDE - Womens_Hosiery Hosiery Leggings MAIN AND ALT PRESENTATION Front Lower Front view, crop above waist/ belly button. Styling to cover top of waistband. Back Lower Back view, crop above waist. Style with cami to show waistband and possible pocket detail. Side Lower Side view. Crop above waist. NO HANDS Style with cami to show waistband and possible pocket detail. Left or right depending on the details. Detail Lower Detail view as shown unless there is a better detail determined on set. Zoom Lower Zoom detail - for closeup of fabric, textures and prints. Avoid seams, wrinkles and graphics on tees. (Vendor images exempt) Front Full (look) Gold Look / Editorial / Catalog / video, if available ADDITIONAL INFO swatch presentation Styling Exception: Multipurpose Hosiery Legging styled bare feet and bare top when requested. 2 STUDIO N - FOR INTERNAL AND VENDOR USE ONLY ONLINE PHOTOGRAPHY GUIDE - Womens_Hosiery Sheer, Textured, Control Top & Thigh High Hosiery MAIN AND ALT PRESENTATION Side Full Side view with right leg forward (watch distance between feet) NO HANDS Crop above top of hosiery. Detail Full (optional) Detail view if requested or needed. Front, Back or closeup on detail. -

Real Silk Company (Indianapolis, Ind.) Records, 1920–1952
Collection # M 0507 F 1016-1055 REAL SILK COMPANY (INDIANAPOLIS, IND.) RECORDS, 1920–1952 Collection Information Biographical Sketch Scope and Content Note Contents Cataloging Information Processed by Paul Brockman 14 December 1988; 16 August 1994 Updated 21 January 2005 Manuscript and Visual Collections Department William Henry Smith Memorial Library Indiana Historical Society 450 West Ohio Street Indianapolis, IN 46202-3269 www.indianahistory.org COLLECTION INFORMATION VOLUME OF 37 manuscript boxes, 40 reels of microfilm (30 linear feet); 1 COLLECTION: box of photographs COLLECTION 1920-1952 DATES: PROVENANCE: John Watson Representing Real Silk Associates, Indianapolis, IN, 24 May 1988 RESTRICTIONS: None COPYRIGHT: REPRODUCTION Permission to reproduce or publish material in this collection RIGHTS: must be obtained from the Indiana Historical Society. ALTERNATE None FORMATS: RELATED None HOLDINGS: ACCESSION 1989.0100 NUMBER: NOTES: BIOGRAPHICAL SKETCH Real Silk Company was founded in 1922 by J.A. and L.L. Goodman. The company ran knitting mills which manufactured hosiery, lingerie, and underwear. At its peak, the company's sales volume averaged more than one million dozen pairs of women's hosiery a year. In addition, Real Silk owned plants in Linton, Indiana, Georgia, and Mississippi. The company ran into financial difficulties in the early 1930s as a result of the Great Depression, and control was assumed by a bank committee. Real Silk's financial situation began to improve shortly thereafter and Gustav Efroymson assumed control of the company in 1932. Difficulties soon occurred with labor over wage increases which resulted in a strike in April and May, 1934, that included the arrests of sixteen strikers in Indianapolis. -
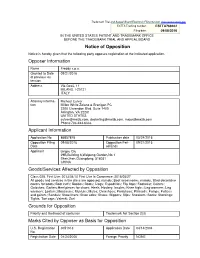
Notice of Opposition Opposer Information Applicant Information
Trademark Trial and Appeal Board Electronic Filing System. http://estta.uspto.gov ESTTA Tracking number: ESTTA769402 Filing date: 09/08/2016 IN THE UNITED STATES PATENT AND TRADEMARK OFFICE BEFORE THE TRADEMARK TRIAL AND APPEAL BOARD Notice of Opposition Notice is hereby given that the following party opposes registration of the indicated application. Opposer Information Name Freddy s.p.a. Granted to Date 09/21/2016 of previous ex- tension Address Via Gesù, 11 MILANO, I-20121 ITALY Attorney informa- Michael Culver tion Millen White Zelano & Branigan PC 2200 Clarendon Blvd. Suite 1400 Arlington, VA 22201 UNITED STATES [email protected], [email protected], [email protected] Phone:703-243-6333 Applicant Information Application No 86857876 Publication date 05/24/2016 Opposition Filing 09/08/2016 Opposition Peri- 09/21/2016 Date od Ends Applicant Lingsu Qiu 29B,Building 6,Weipeng Garden,No.1 Shenzhen,Guangdong, 518031 CHINA Goods/Services Affected by Opposition Class 025. First Use: 2013/04/10 First Use In Commerce: 2015/05/27 All goods and services in the class are opposed, namely: Boot accessories, namely, fitted decorative covers for boots; Boot cuffs; Booties; Boots; Clogs; Espadrilles; Flip flops; Footwear; Gaiters; Galoshes; Garters;Heel pieces for shoes; Heels; Hosiery; Insoles; Knee highs; Leg-warmers; Leg warmers; Loafers; Moccasins; Mukluks; Mules; Overshoes; Pantyhose; Plimsolls; Pumps; Puttees and gaiters; Sandals; Shoe liners; Shoe soles; Shoes; Slippers; Slips; Sneakers; Socks; Stockings; Tights; Toe caps; Valenki; Zori Grounds for Opposition Priority and likelihood of confusion Trademark Act Section 2(d) Marks Cited by Opposer as Basis for Opposition U.S. -
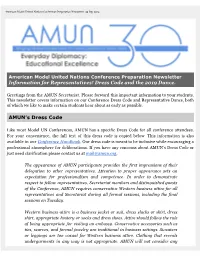
AMUN Dress Code & the Representative Dance
American Model United Nations Conference Preparation Newsletter. 30 Sep 2019. American Model United Nations Conference Preparation Newsletter Information for Representatives! Dress Code and the 2019 Dance. Greetings from the AMUN Secretariat. Please forward this important information to your students. This newsletter covers information on our Conference Dress Code and Representative Dance, both of which we like to make certain students hear about as early as possible. AMUN’s Dress Code Like most Model UN Conferences, AMUN has a specific Dress Code for all conference attendees. For your convenience, the full text of this dress code is copied below. This information is also available in our Conference Handbook. Our dress code is meant to be inclusive while encouraging a professional atmosphere for deliberations. If you have any concerns about AMUN’s Dress Code or just need clarification please contact us at [email protected]. The appearance of AMUN participants provides the first impressions of their delegation to other representatives. Attention to proper appearance sets an expectation for professionalism and competence. In order to demonstrate respect to fellow representatives, Secretariat members and distinguished guests of the Conference, AMUN requires conservative Western business attire for all representatives and Secretariat during all formal sessions, including the final sessions on Tuesday. Western business attire is a business jacket or suit, dress slacks or skirt, dress shirt, appropriate hosiery or socks and dress shoes. Attire should follow the rule of being appropriate for visiting an embassy. Conservative accessories such as ties, scarves, and formal jewelry are traditional in business settings. Sweaters or leggings are too casual for Western business attire. -
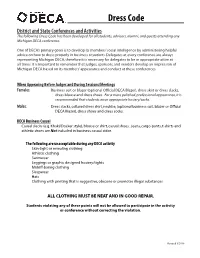
11-12 Forms.Indd
Dress Code District and State Conferences and Activities The following Dress Code has been developed for all students, advisors, alumni, and guests attending any Michigan DECA conference. One of DECA’s primary goals is to develop its members’ social intelligence by administering helpful advice on how to dress properly in business situations. Delegates at every conference are always representing Michigan DECA, therefore it is necessary for delegates to be in appropriate attire at all times. It is important to remember that judges, sponsors, and vendors develop an impression of Michigan DECA based on its members’ appearance and conduct at these conferences. When Appearing Before Judges and During Sessions/Meetings Females: Business suit or blazer (optional Offi cial DECA Blazer), dress skirt or dress slacks, dress blouse and dress shoes. For a more polished, professional appearance, it is recommended that students wear appropriate hosiery/socks. Males: Dress slacks, collared dress shirt, necktie; (optional business suit, blazer or Offi cial DECA Blazer), dress shoes and dress socks. DECA Business Casual Casual slacks (e.g. Khaki/Docker style), blouse or shirt, casual shoes. Jeans, cargo-pants, t-shirts and athletic shoes are Not included in business casual attire. The following are unacceptable during any DECA activity Skin-tight or revealing clothing Athletic clothing Swimwear Leggings or graphic designed hosiery/tights Midriff-baring clothing Sleepwear Hats Clothing with printing that is suggestive, obscene or promotes illegal substances ALL CLOTHING MUST BE NEAT AND IN GOOD REPAIR. Students violating any of these points will not be allowed to participate in the activity or conference without correcting the violation. -

Today Hosiery Is Used to Refer to Tights and Stockings, but the Term Once Referred to Machine-Knitted Hose and Underwear Which Might Be Made from Cotton Or Silk
Hosiery Today hosiery is used to refer to tights and stockings, but the term once referred to machine-knitted hose and underwear which might be made from cotton or silk. Newspaper cutting from The Herald, 1928. Mrl ACC 2772. It was produced on the stocking frame until the 19th century when power-driven full-fashioned knitting machines were invented, which would go on to produce a wider range of knitwear clothing including nylon tights. Fully-fashioned refers to the knitting of a shaped Advert for I & R Morley’s Australian-made underwear, component such as a sleeve (achieved by 1932. Mrl ACC 2772. increasing or decreasing the number of loops to produce the shape). In the East Midlands firms invested heavily in full-fashioned knitting machines which they considered to be superior. Imports and globalisation William Cotton’s first patent, Yarns: The magazine of the House of Brettle, 1860. BBE ACC 1532. eventually forced most companies to adopt the cheaper cut and sew method using Vol 1, no 1, 1929. BBE ACC 1532. circular machines to produce fabric knitted in large tubes, which is how most of the clothes we wear today are made. William Cotton (born in Leicestershire in 1819) invented a full-fashioned machine in 1860 capable of producing four items at once. When his patent ran out in 1879 other firms began developing their own machines. In 1929 Brettles developed their first full fashioned silk hose machine, built at their works at Belper, Derbyshire. Previously they would have to wait over a year for a British firm to build them a new machine, or even go to Germany for their requirements. -

Personnel Practices: Dress Code Policies
International Public Management Association for Human Resources HR-CENTER January 2006 Personnel Practices: Dress Code Policies International Public Management Association for Human Resources 1617 Duke Street Alexandria, VA 22314 (703)-549-7100 http://www.ipma-hr.org 1 DRESS CODE POLICIES Table of Contents I. Dress Code Overview……………………………………..…..3 II. Sample Policies A. City of Carrollton, TX………………………………….…..6 B. City of Fort Worth, TX……..………..…………………..…8 C. City of Lodi, CA…………………………………………..15 D. State of Michigan……………………………………..…...12 E. Okalahoma City, OK……….………...…………………....15 As you develop your own plans and policies, please email information to gov@ipma- hr.org. IPMA-HR HR Center 1617 Duke Street Alexandria, VA 22314 (703)-549-7100 2 A new paradigm for "dress for success"? Body piercing. T-shirts. Facial hair. Tattoos. Where should employers draw the line in the workplace? What grooming guidelines, if any, should organizations develop? When it comes to dress codes, what legal rights do employers and employees have? Are there any guidelines on religious dress? These questions and more are what employers and employees are asking everyday. With times quickly changing and as younger generations get older, norms and expectations slowly transform. Business attire five days a week has become more rare in the average workplace or agency. Young executives and managers are more liberal in there approaches to issues of this sort, making the term “dress for success” less stressful and more cost effective for the average person. Grooming Standards Personal "style" reflects a diverse workplace and often individuals with tattoos are creative individuals. However depending on his or her job, an employee's appearance may alienate customers. -

Give “Him”These J£S3.|Gift Silk Hosiery L"Di 6 1 Mr
THE EVENING STAR, WASHJNGTON, D. C„ FRIDAY, DECEMBER 19. 1930, B-3 and Mra. Chewning during the holi- ready been made for the Midshipmen Blagden terrace, Washington, are then he has served u chief of staff of Zoo* to Philadelphia; Army- MAIDEN Pint Lieut. Jel- days, and some or her classmates, Miss dance that will be held at the stopping at Hotel Everglades, Miami, NAME WORTH sls the Hawaiian Division, m a director of ferion C. Campbell, Field Artillery, Tuesday evening, during their Winter visit Florida. Hostess the Industrial College In this city and from Port Mary Hansford Wallace, Miss Anne Navy Country Club in Diplomatic 8111, Okie., to the Panama m SOCIETY December 30. At this rate “It is believed CHICAGO. December 19 (JP).— What’* at Atlanta, Oa. Canal Zone; Capt. Ottmann W. Free- Green and Miss Virginia Darling, who by the two Mr. John Paul de Berry of Shanghi, Col. vr club officials that even with China, in a name? Mr*. George Vldmer, Cavalry, has born, Infantry, Bioux Falls. 8. Dak., large during is the guest of Mr. and Mrs. Eli Kathryn Kessler been to (Continued From Second Page.) came to Washington for the ball last additions erected the Sum- Smith figured transferred from Omaha, Nebr., Fort Benning, Oa . Capt. WUUam a mer the building will be crowded to B. at their home on Massachu- her maiden name was worth to the 434th Field Artillery at Mont- Williams, Medical evening, are also house guests of Mr. setts avenue. than Administrative of the Chewning. capacity. more sls a week. -

FEEDBACK FORM (Cont’D) Please Provide Detailed Comments
FEEDBACK FORM (cont’d) Please provide detailed comments. Feel free to attach extra pages if needed. Thanks for your assistance. Section Page Specific Specific or learning No. Comment Suggested Change Domain 5. What additional guidance or resources would be helpful for you to implement these early learning guidelines with your children? Feel free to copy and distribute this form and the Oklahoma Early Learning Standards to co-workers, colleagues, and early childhood professionals for review. OKDHS Pub. No. 10-54 Issued 10/10 Please fax this form to: 405-522-2564 or This publication is authorized by the Oklahoma Commission for Human Services in accordance with state and federal regulations and printed by Mail to: Department of Human Services the Oklahoma Department of Human Services at a cost of $645.60 for 807 copies. Copies have been deposited with the Publications Clearinghouse of Oklahoma Child Care Services the Oklahoma Department of Libraries. OKDHS offices may request copies on ADM-9 (23AM009E) electronic supply orders. Members of the public may P.O. Box 25352 obtain copies by contacting OKDHS Design Services at 1-877-283-4113 (toll free), by faxing an order to Oklahoma City, OK 73125, or (405) 962-1740, or by downloading a copy at www.okdhs.org/library/pubs. Return by email to: [email protected]. OOkkllaahhoommaa EEAARRLLYY LLEEAARRNNIINNGG GGUUIIDDEELLIINNEESS FFOORR CCHHIILLDDRREENN AAggeess TThhrreeee tthhrroouugghh FFiivvee Table of Contents ________________________________________________________________________ INTRODUCTION -

STANDARDIZED STUDENT DRESS CODE 2019-2020 BOARD APPROVED MARCH 19,2019 Tops and Bottoms
STANDARDIZED STUDENT Unacceptable Colors of Hair DRESS CODE Unnatural hair colors including primary colors, 2019-2020 intermediate colors and /or metallic colors. Combs or picks worn in the hair. BOARD APPROVED MARCH 19,2019 Brochure contains examples of acceptable / unacceptable items, but is not all inclusive. Please Acceptable Head Coverings refer to the standardized student dress code written None, except for special occasions approved by the version for a complete list below. principal. Exemptions and opt-out provisions will be considered for religious or medical reasons. Acceptable Outer Wear Styles Unacceptable Head Coverings Can be worn inside the school building any solid color. Head coverings are not permitted and cannot be visible on campus, in the school building, or in the waiting areas on campus. Head coverings include, but are not limited to sweatbands, caps, hats, bandanas, skull caps and hoodies. EISD letter jackets and school organization sweaters or jackets are acceptable. Tops and Bottoms May be worn outside of school building Approved Colors for Bottoms Jumpers/Skirts/Skorts/Pants/Shorts/Capris Black Navy Khaki Unacceptable Outerwear Any shade of the color Khaki Acceptable Styles of Bottoms Pleated or flat front style, cotton, twill, chino .etc. most fabrics other than denim. Length: Grades PK-4: hem of the pants/shorts/capris must not be Trench Coat Duster more than 3 inches above the knee. Grades 5-12: hem of the pants/shorts/capris must touch the kneecap or below. Acceptable Socks/Hosiery/Leggings Socks (ankle, mid-calf and knee) hosiery, leggings and tights. When hosiery, leggings and tights are part of the attire they must be worn under skirts or dresses. -

Student Conduct Fnca Dress Code (Local)
Fort Worth ISD 220905 STUDENT CONDUCT FNCA DRESS CODE (LOCAL) PURPOSE The District’s dress code is established in an effort to improve stu- dent learning and to facilitate a safe learning environment. It is in- tended to instill discipline, prevent disruption, avoid safety hazards, and teach respect for authority. GENERAL GUIDELINES Students shall be dressed and groomed in a manner that is clean and neat and that will not be a health or safety hazard to them- selves or others. The District prohibits any clothing or grooming that in the principal’s judgment may reasonably be expected to cause disruption of or interference with normal school operations. The District’s dress code shall be a part of the local Student Code of Conduct. PREKINDERGARTEN – Students shall be required to adhere to the dress code during GRADE 12 school hours and dress appropriately while participating in other school-sponsored activities. Clothing shall be of the correct size for students, with no sagging pants. Shirts or blouses shall be tucked into clothing. Clothing that complies with the dress code may be purchased from retail stores of a parent’s or guardian’s choice. PREKINDERGARTEN Bottoms shall comply with the following: – GRADE 8 1. Navy, khaki, black, or blue denim pants, shorts, skirts, skorts, capris, or jumpers are acceptable; students may wear denim blue jeans that are free of embellishments. 2. All bottoms must be hemmed or cuffed. 3. Skirts, skorts, and shorts shall be no shorter than three inches above the knee. Tops shall comply with the following: 1. Two solid colors, navy or white, are acceptable. -

Hosiery: Function, Fashion, and Patriotism Collide with Science
Hosiery: Function, Fashion, and Patriotism Collide with Science by Wendy C. Potter, 2014 CTI Fellow David W. Butler High School This curriculum unit is recommended for: Apparel and Textile Production I and II, grades 9-12th Keywords: hosiery, textile history, common core, fashion history, culture Teaching Standards: See Appendix 1 for teaching standards addressed in this unit. Synopsis: Hosiery, a leading industry in fashion for years, not only lends itself to fashionable choices for the consumer, but also practical choices for all walks of life. Be it military, post-surgery patient, diabetic, athlete, businessman, or fashion conscious student, hosiery fits into everyone’s life. Having been around for centuries, hosiery continues to improve our quality of life as a result of chemical engineering. This curriculum unit takes a panoramic view of the history of hosiery. Students will be challenged to investigate apparel from various centuries as it relates to hosiery as well as discuss topics such as modesty, science history, culture, war, and gender issues. While this curriculum was designed to fit into Apparel and Textile Production I and II Essential Standards, parts of it will complement other subjects. Common core standards in writing, literacy, and math are addressed, while also giving the student a rich history in an area of fashion that is often overlooked. Use of current technology is encouraged throughout the curriculum, but can be modified with consideration to technology limitations and accessibility. Upon completing components of the curriculum unit, the student will have an interdisciplinary view of hosiery, necessary for career exploration in the apparel industry.