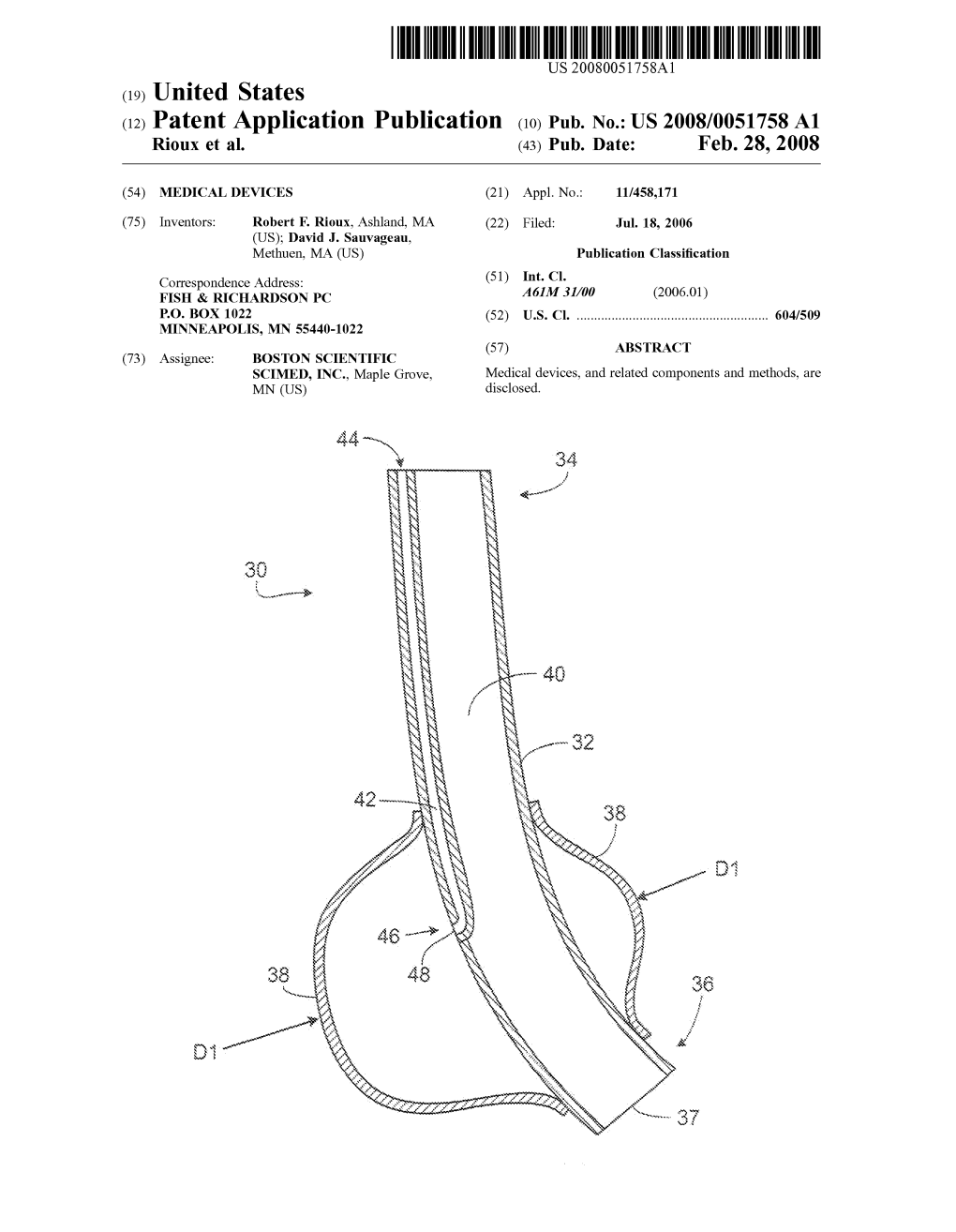
(12) Patent Application Publication (10) Pub. No.: US 2008/0051758 A1 Rioux Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2005/0129775 A1 Lanphere Et Al
US 2005O129775A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0129775 A1 Lanphere et al. (43) Pub. Date: Jun. 16, 2005 (54) FERROMAGNETIC PARTICLES AND (22) Filed: Aug. 27, 2004 METHODS Related U.S. Application Data (75) Inventors: Janel Lanphere, Pawtucket, RI (US); Erin McKenna, Boston, MA (US); (63) Continuation-in-part of application No. 10/651,475, Thomas V. Casey II, Grafton, MA filed on Aug. 29, 2003. (US) Publication Classification Correspondence Address: FISH & RICHARDSON PC (51) Int. Cl." ........................... A61K 9/127; A61K 9/14; 225 FRANKLIN ST A61K 33/26 BOSTON, MA 02110 (US) (52) U.S. Cl. ............................................ 424/489; 424/646 (73) ASSignee: Siedle Systems, Inc., Maple (57) ABSTRACT (21) Appl. No.: 10/928,452 Ferromagnetic particles and methods are disclosed. Patent Application Publication Jun. 16, 2005 Sheet 1 of 5 US 2005/0129775 A1 Patent Application Publication Jun. 16, 2005 Sheet 2 of 5 US 2005/0129775 A1 s nS) l r N. 1 Yn ESDNIAJ?SdWßd N-EZT| 1 - - - - - - - - - - - - - - - - - - - - - - - - - a - - a - - - - Patent Application Publication Jun. 16, 2005 Sheet 3 of 5 US 2005/0129775 A1 : 3 L D Cl U c). Z Y X C) Patent Application Publication Jun. 16, 2005 Sheet 4 of 5 US 2005/0129775 A1 s s Patent Application Publication Jun. 16, 2005 Sheet 5 of 5 US 2005/0129775 A1 26SS EMBOLIC PARTICLES FIBROID jS. 111 UTERINE ARTERY CATHETER 150 FIG. R., US 2005/0129775 A1 Jun. 16, 2005 FERROMAGNETIC PARTICLES AND METHODS 0011 Heating a particle can include exposing the particle to RF radiation. CROSS-REFERENCE TO RELATED 0012. -

Supplement 12
APPROVED DRUG PRODUCTS with THERAPEUTIC EQUIVALENCE EVALUATIONS 14TH EDITION Cumulative Supplement 1 2 DECEMBER 1994 CONTENTS PAGE 1.0 INTRODUCTION............................................. iii 1.1 Ilow to Use the Cumulative Supplement .. iii 1.2 Products Requiring Revised Labeling for Full Approval . v 1.3 Applicant Name Changes. vi 1.4 New Indications for Previously Approved Drug Products ............... vii 1 .5 USP Monograph Title Additions or Changes . ix 1.6 Report of Counts for the Prescription Drug Product List. x 2.0 DRUG PRODUCT LISTS ....................................... 2.1 Prescription Drug Product List ................................. 1 2.2 OTC Drug Product List ...................................... 61 2.3 Drug Products with Approval under Section 505 of the Act Administered by the Center for Biologics Evaluation and Research List. 63 2.4 Orphan Drug Product Designations . 64 2.5 Drug Products Which Must Demonstrate in vivo Bioavailability Only if Product Fails to Achieve Adequate Dissolution ................ 70 2.6 Biopharmaceutic Guidance Availability ........................... 71 2.7 ANDA Suitability Petitions . 72 PATENT AND EXCLUSIVITY INFORMATION ADDENDUM A. Exclusivity Terms. 74 B. Patent and Exclusivity Lists . 76 APPROVED DRUG PRODUCTS with THERAPEUTIC EQUIVALENCE EVALUATIONS 14TH EDITION CUMULATIVE SUPPLEMENT 12 DECEMBER 1994 1.0 INTRODUCTION 1.1 HOW TO USE THE CUMULATIVE SUPPLEMENT This Cumulative Supplement is one of a series of monthly updates to the Approved Drug Products with Therapeutic Equivalence -

LGC Standards Pharmacopoeial Reference Standards 2014
LL CTS INKSP RODUTO A L P ITH W WEBSHO LGC Standards Pharmacopoeial reference standards 2014 FOR STANDARDS WITH CofA SEE OUR CATALOGUE: PHARMACEUTICAL IMPURITIES AND PRIMARY REFERENCE STANDARDS LGC Quality – ISO Guide 34 • GMP/GLP • ISO 9001 • ISO/IEC 17025 • ISO/IEC 17043 Pharmaceutical impurities Code Product CAS No. CS Price Unit Adiphenine Hydrochloride O LGC Standards N O MM1172.00 Adiphenine Hydrochloride 50-42-0 A 250mg HCl Pharmaceutical impurities and Adrenaline Tartrate OH H OH O OH primary reference standardsMM0614.00 2014 N OH Adrenaline Tartrate 51-42-3 A 500mg OH OH O OH OH H MM0614.02 L-Adrenaline 51-43-4 A 500mg OH N OH Imp. C (EP) as Hydrochloride: 1-(3,4-Di- O H OH MM0614.13 hydroxyphenyl)-2-(methylamino)ethanone 62-13-5 A 100mg N HCl Hydrochloride (Adrenalone Hydrochloride) OH (1R)-1-(3,4-Dihydroxyphenyl)-2- OH O S O MM0614.01 methylaminoethanesulphonic Acid H 78995-75-2 A 100mg OH N (Adrenaline -Sulphonate) OH Alanine NH2 MM0566.00 Alanine 56-41-7 A 500mg OH O Imp. A (Pharmeuropa): (2 S)-2-Aminobutanedioic Acid O NH 2 MM0567.00 OH (Aspartic Acid) 56-84-8 A 500mg OH O Albendazole O H MM0382.00 Albendazole N O 54965-21-8 A 500mg N H S N Imp. A (EP): 5-(Propylsulphanyl)-1H- H MM0382.01 N 80983-36-4 A 100mg NH2 benzimidazol-2-amine S N O H Imp. B (EP): Methyl [5-Propylsulphinyl)- N O MM0382.02 N 54029-12-8 A 100mg H 1H-benzimidazol-2-yl]carbamate S N O O H Imp. -

Iodine-Containing Drugs
Iodine-containing drugs Iodine-containing drugs (iodine) usually have an iodine content of >5mg/tablet or ml. The antiarrhythmic agent amiodarone, for example, contains 75 mg iodine/tablet, 10 ml betaisodona solution about 110 mg . - The administration of X-ray contrast media is another important reason for excessive iodine exposure. X-ray contrast media frequently contain > 100 mg iodine/ml. Contrast media contain almost exclusively organically bound iodine, but in vivo these compounds are partially deiodinated (deiodinase) (Mann et al. Eur J. Endocrinol 1994; 130 (5): 498). Assuming that water-soluble contrast media is eliminated within 10 to 14 days, enzymatic separation of iodine nevertheless leads to an offer of about 14 to 175 mg in the thyroid. Fat-soluble contrast media applied in cholecystograms have a much longer half time in the organism, and iodine can consequently be separated long. The table of Surks et al. (New Engl J Med 1995; 333: 1688) gives a survey of the most important iodine preparations applied in the USA. Iodine Content of Some Iodine Containing Medications and Radiographic Contrast Agents SUBSTANCE AMOUNT OF IODINE Expectorants Iophen 25 mg/ml Organidin (iodinated glycerol) 15 mg/tablet Par Glycerol 5 mg/ml R-Gen 6 mg/ml Iodides Potassium iodide (saturated solution) -25 mg/drop Pima syrup (potassium iodide) 255 mg/ml Lugol's solution (potassium iodide -7 mg/drop + iodine) Iodo-Niacin 115 mg/tablet Antiasthmatic drugs Mudrane 195 mg/tablet Elixophyllin-KI (theophylline) elixir 6.6 mg/ml © Merck KGaA 2002 Iophylline 2 mg/ml Antiarrhythmic drugs Amiodarone 75 mg/tablet Antiamebic drugs Iodoquinol 134 mg/tablet Topical antiseptic agents Poidone-iodine 10 mg/ml Clioquinol 12 mg/g Douches Povidone-iodine 10 mg/ml Radiographic contrast agents Iopanoic acid 333 mg/tablet Ipodate sodium 308 mg/tablet Intravenous preparations 140-380 mg/ml M.J. -
Summary and Recommendations for Thyroid Screening in Pregnancy: Is
Gregory A. Brent, MD Departments of Medicine and Physiology David Geffen School of Medicine at UCLA Etiologies of Hypothyroidism • Chronic autoimmune thyroiditis-Hashimoto’s disease • Partial thyroidectomy. • Radioactive iodine therapy for treatment of hyperthyroidism. • External radiotherapy of the head and neck in patients with Hodgkin’s lymphoma, leukemia, brain tumors, or bone-marrow transplantation. • Infiltrative disorders of the thyroid gland (eg, amyloidosis, sarcoidosis,hemochromatosis, or Riedel’s thyroiditis). Modified from Cooper and Biondi Lancet 379:1142, 2012 Pearce and Braverman Best Pract Clin Endo Metab 23:801, 2009 Agent Example of Sources Mode of Action Thyroid Disease in Humans Polychlorinated Found in coolants and TR Possible increase in biphenyls (PCBs) lubricants, properties; agonist/antagonist, TSH, thyroid multiple congeners, can alter levels of T4 autoantibodies, thyroid lipophilic and TSH volume Organochlorine Used as pesticide on Induce hepatic No established pesticides crops glucuronyltransferase association (UDPGTs) Polybrominated Found in flame Bind to TRs, Increase in diphenylethers retardants displaces T4 from hypothyroidism in some (PBDEs) binding proteins studies Bisphenol-A (BPA) Used in plastic bottles Antagonize TR, lower No established serum T4 association Adapted from Brent GA Thyroid 20:755, 2010 Agent Example of Mode of Action Thyroid Disease Sources In Humans Perchlorate, Rocket fuel, Inhibits iodine No established Thiocyanate fertilizer, uptake, at sufficient association smoking levels reduces -

PF 41(4) Table of Contents Publish Date: Jul 1, 2015
PF 41(4) Table of Contents Publish date: Jul 1, 2015 PROPOSED IRA Proposed IRA Intro Section USP MONOGRAPHS Methocarbamol (1-Jan-2016) Protamine Sulfate Injection (1-Jan-2016) IN-PROCESS REVISION IPR Introduction GENERAL CHAPTERS <1130> NUCLEIC ACID-BASED TECHNIQUES—APPROACHES FOR DETECTING TRACE NUCLEIC ACIDS (RESIDUAL DNA TESTING) (USP39-NF34 2S) REAGENTS, INDICATORS, AND SOLUTIONS Reagent Specifications Carbon Tetrachloride (USP39-NF34 2S) 4-Hydroxy-4-phenylpiperidine [NEW] (USP39-NF34 2S) Monosodium Glutamate [NEW] (USP39-NF34 2S) 6Z-Retinoic Acid [NEW] (USP39-NF34 2S) Sulfaguanidine [NEW] (USP39-NF34 2S) Chromatographic Columns L## (Tretinoin, Cosmosil Cholesterol) [NEW] (USP39-NF34 2S) REFERENCE TABLES Container Specifications Containers for Dispensing Capsules and Tablets [NEW] (USP39-NF34 2S) Description and Solubility Description and Solubility of USP and NF Articles [NEW] (USP39-NF34 2S) Description and Solubility - C Description and Solubility - F Description and Solubility - M DIETARY SUPPLEMENT MONOGRAPHS Methylcobalamin Tablets [NEW] (USP39-NF34 2S) Northern Schisandra Fruit Dry Extract [NEW] (USP39-NF34 2S) PF 41(4) Table of Contents 1 | Page NF MONOGRAPHS Chlorobutanol (USP39-NF34 2S) Eucalyptus Oil (USP39-NF34 2S) USP MONOGRAPHS Albuterol Sulfate (USP39-NF34 2S) Alprazolam Extended-Release Tablets (USP39-NF34 2S) Alprazolam Orally Disintegrating Tablets (USP39-NF34 2S) Aminobenzoate Potassium (USP39-NF34 2S) Aminobenzoate Potassium Capsules (USP39-NF34 2S) Aminobenzoate Sodium (USP39-NF34 2S) Gamma-Aminobutyric Acid Capsules -

Col11bined Index to USP 37 and NF 32, Volul11es 1-4
..... Combined Index to USP 37 and NF 32 Abaca-Aceto 1-1 COl11bined Index to USP 37 and NF 32, Volul11es 1-4 Page citations refer to the pages of Volumes 7, 2, 3, and 4 of uSP 37-NF 32. This index is repeated in its entirety in each volume. 1-1554 Volume 1 1555-3460 Volume 2 3461-5230 Volume 3 5231-6262 Volume 4 Numbers in angle brackets such as (421) refer to chapter numbers in the General Chapters section. and (salts of) chlorpheniramine, isometheptene mucate, and dextromethorphan, and dichloralphenazone capsules, 3416 phenylpropanolamine, oral solution and oxycodone capsules, 4141 Abacavir containing at least three of the and oxycodone tablets, 4142 oral solution, 1S5 5 following, 1576 and pentazocine tablets, 4231 sulfate, 1556 and (salts of) chlorpheniramine, and propoxyphene hydrochloride tablets, tablets, 1557 dextromethorphan, and 4458 Absolute phenylpropanolamine, tablets containing and propoxyphene napsylate tablets, 4463 alcohol, 1373 at least three of the following, 1577 and pseudoephedrine hydrochloride ether, 1372 and (salts of) chlorpheniramine, tablets, 1597 Absorbable dextromethorphan, and oral solution, 1566 dusting powder, 2745 pseudoephedrine, capsules containing at for effervescent oral solution, 1567 gelatin film, 3132 least three of the following, 1579 suppositories, 1567 gelatin sponge, 3132 and (salts of) chlorpheniramine, oral suspension, 1568 surgical suture, 4808 dextromethorphan, and tablets, 1569 Absorbent pseudoephedrine, oral powder extended-release tablets, 1570 cotton, 1372 containing at least three of -

1484 Contrast Media
1484 Contrast Media myelography, see under Iohexol, p.1483; for specific references, to iodine or to other contrast media, severe hyperthyroidism, hy- Profile see below. peruricaemia, or cholangitis. Because of its cholinergic action, Iopentol is a nonionic monomeric iodinated radiographic con- Effects on the nervous system. Reports of serious neurolog- premedication with atropine has been suggested in some coun- trast medium (see p.1474). It may be given intravenously, intra- ical sequelae to lumbar myelography with iopamidol. tries for patients with coronary heart disease. Iodine-containing arterially, orally, or by instillation into body cavities, and is used contrast media may interfere with thyroid-function tests and with in procedures including angiography, arthrography, endoscopic 1. Wallers K, et al. Severe meningeal irritation after intrathecal in- jection of iopamidol. BMJ 1985; 291: 1688. some blood and urine tests. retrograde cholangiopancreatography, hysterosalpingography, urography, and visualisation of the gastrointestinal tract. It is also 2. Robinson C, Fon G. Adverse reaction to iopamidol. Med J Aust Breast feeding. No adverse effects have been observed in 1986; 144: 553. used for contrast enhancement in computed tomography. breast-feeding infants whose mothers were receiving iopanoic 3. Bell JA, McIlwaine GG. Postmyelographic lateral rectus palsy 1 associated with iopamidol. BMJ 1990; 300: 1343–4. acid and the American Academy of Pediatrics considers that it Iopentol is usually available as solutions containing 32.9 to 4. Mallat Z, et al. Aseptic meningoencephalitis after iopamidol my- is therefore usually compatible with breast feeding. 76.8% of iopentol (equivalent to 150 to 350 mg/mL of iodine) elography. Lancet 1991; 338: 252. -

(12) Patent Application Publication (10) Pub. No.: US 2002/0010208A1 Shashoua Et Al
US 2002001 0208A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2002/0010208A1 Shashoua et al. (43) Pub. Date: Jan. 24, 2002 (54) DHA-PHARMACEUTICAL AGENT Related U.S. Application Data CONJUGATES OF TAXANES (63) Continuation of application No. 09/135,291, filed on (76) Inventors: Victor Shashoua, Brookline, MA (US); Aug. 17, 1998, now abandoned, which is a continu Charles Swindell, Merion, PA (US); ation of application No. 08/651,312, filed on May 22, Nigel Webb, Bryn Mawr, PA (US); 1996, now Pat. No. 5,795,909. Matthews Bradley, Layton, PA (US) Publication Classification Correspondence Address: Edward R. Gates, Esq. (51) Int. Cl." ............................................ A61K 31/337 Wolf, Greenfield & Sacks, P.C. (52) U.S. Cl. .............................................................. 514/449 600 Atlantic Avenue Boston, MA 02210 (US) (57) ABSTRACT The invention provides conjugates of cis-docosahexaenoic (21) Appl. No.: 09/846,838 acid and pharmaceutical agents useful in treating noncentral nervous System conditions. Methods for Selectively target 22) Filled: Mayy 1, 2001 ingg pharmaceuticalp agents9. to desired tissues are pprovided. Patent Application Publication Jan. 24, 2002 Sheet 1 of 14 US 2002/0010208A1 1 OO 5 O -5OO - 1 OO-9 -8 -7 -6 -5 -4 LOG-10 OF SAMPLE CONCENTRATION (MOLAR) CCRF-CEM-o- SR ----- RPM-8226----- K-562- - -A - - HL-60 (TB) -g- - MOLT4: ... O Fig. 1 1 OO 5 O -5OO -1 O O -8 -7 -6 -5 -4 -- 9 LOGo OF SAMPLE CONCENTRATION (MOLAR) A549/ATCC-o-NS326. NCEKVX 28. --Q-- NCI-H322M-...-a---Eidsf8::... NC-H522--O-- HOP-62---Fig. 2 a-- NC-H460.-------- Patent Application Publication Jan. -

DRUG-INDUCED HYPOTHYROIDISM Drug-Induced Primary
394 MEDICINA - VolumenISSN 77 - Nº1669-9106 5, 2017 SPECIAL ARTICLE MEDICINA (Buenos Aires) 2017; 77: 394-404 DRUG-INDUCED HYPOTHYROIDISM LEONARDO F. L. RIZZO1, DANIELA L. MANA1, HÉCTOR A. SERRA1, 2 1Dirección Médica Química Montpellier SA, 2Cátedra de Farmacología, Facultad de Ciencias Médicas, U.C.A., Buenos Aires, Argentina Abstract The thyroid axis is particularly prone to interactions with a wide variety of drugs, whose list increases year by year. Hypothyroidism is the most frequent consequence of drug-induced thyroid dysfunction. The main mechanisms involved in the development of primary hypothyroidism are: inhibition of the synthesis and/ or release of thyroid hormones, immune mechanisms related to the use of interferon and other cytokines, and the induction of thyroiditis associated with the use of tyrosine kinase inhibitors and drugs blocking the receptors for vascular endothelial growth factor. Central hypothyroidism may be induced by inhibition of thyroid-stimulating hormone (bexarotene or corticosteroids) or by immunological mechanisms (anti-CTLA4 or anti-PD-1 antibody drugs). It is also important to recognize those drugs that generate hypothyroidism by interaction in its treatment, either by reducing the absorption or by altering the transport and metabolism of levothyroxine. Thus, it is strongly recommended to evaluate thyroid function prior to the prescription of medications such as amiodarone, lithium, or interferon, and the new biological therapies that show important interaction with thyroid and endocrine function in general. Key words: thyroid, hypothyroidism, drugs Resumen Hipotiroidismo inducido por drogas. El eje tiroideo es particularmente proclive a sufrir interacciones con una amplia variedad de drogas, cuya lista se acrecienta año a año. -

Revised References to Heavy Metals <231>
Revised References to Heavy Metals <231> Targeted Official Date for Omission of References: 01-January-2018 Title File Type <3> Topical And Transdermal Drug Products--Product Quality Tests General Chapter <661> Containers--Plastics General Chapter <1059> Excipient Performance General Chapter <1086> Impurities In Drug Substances And Drug Products General Chapter <1151> Pharmaceutical Dosage Forms USP Acarbose USP Acebutolol Hydrochloride USP Acesulfame Potassium NF Acetaminophen USP Acetazolamide USP Acetic Acid NF Diluted Acetic Acid NF Glacial Acetic Acid USP & NF Acetohexamide USP Acetohydroxamic Acid USP Acetylcysteine USP & NF Acetyltributyl Citrate NF Acetyltriethyl Citrate NF Acetyltyrosine DS Acitretin USP Adapalene USP Adenine USP Adenosine USP S-Adenosyl-L-methionine Disulfate Tosylate DS Adipic Acid NF Agar NF Alanine USP & DS Alclometasone Dipropionate USP Alcohol in Dextrose Injection USP Alendronate Sodium USP Alfadex NF Alginic Acid NF Alprazolam USP Altretamine USP Ammonium Alum USP Potassium Alum USP Alumina and Magnesia Oral Suspension USP Alumina, Magnesia, and Calcium Carbonate Oral Suspension USP Aluminum Acetate Topical Solution USP Aluminum Chloride USP Aluminum Chlorohydrate USP Aluminum Chlorohydrate Solution USP Aluminum Chlorohydrex Polyethylene Glycol USP Aluminum Chlorohydrex Propylene Glycol USP Aluminum Dichlorohydrate USP Aluminum Dichlorohydrate Solution USP Aluminum Dichlorohydrex Polyethylene Glycol USP Aluminum Dichlorohydrex Propylene Glycol USP Aluminum Hydroxide Gel USP Dried Aluminum Hydroxide Gel -
Supplement 12
'95 15TH EDITION U.S DEPARTMENT OF HEALTH AND HUMAN$iER\WIC;ES PUBUC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION ANDHESEAlRCH OFFICE OF MANAGEMENT . IJIVISION OF DRUG INFORMATION RESOURCES SUBSCRIBE NOW! Available in March 1996 New 16th Edition APPROVED DRUG PRODUCTS WITH THERAPEUTIC EQUIVALENCE EVALUATIONS 16lli EDITION 1996 CONTENTS • Prescription Drug Product List .' • OTC Drug Product List • Drug Products with Approval under Section 505 of the Act Administered by the Center for Biologics Evaluation and Research List • Discontinued Drug Product List • USP Monograph Title Additions or Changes • Orphan Drug Product Designations • Drug Products Which Must Demonstrate in vivo Bioavailability Only if Product Fails to Achieve Adequate Dissolution • Biopharmaceutic Guidance Availability • ANDA Suitability Petitions • Patent and Exclusivity Information See Subscription Form Inside Back Cover APPROVED DRUG PRODUCTS with THERAPEUTIC EQUIVALENCE EVALUATIONS 15TH EDITION Cumulative Supplement 12 DECEMBER 1995 CONTENTS PAGE 1.0 INTRODUCTION.............................................. iii 1 .1 How to Use the Cumulative Supplement ........................... iii 1.2 Court Order Affecting Uruguay Round Agreements Act-Extended Patents .... iv 1.3 Products Requiring Revised Labeling for Full Approval . v 1.4 Applicant Name Changes . vi 1.5 Availability of the Publication and Updating Procedures . vii 1.6 Report of Counts for the Prescription Drug Product List. viii 2.0 DRUG PRODUCT LISTS ........................................ 2.1 Prescription Drug Product List ................................. 2.2 OTC Drug Product List ...................................... 68 2.3 Drug Products with Approval under Section 505 of the Act Administered by the Center for Biologics Evaluation and Research List ..... 73 2.4 Orphan Drug Product Designations .............................. 74 2.5 Drug Products Which Must Demonstrate in vivo Bioavailability Only if Product Fails to Achieve Adequate Dissolution ...............