What Do We Know About COVID-19?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plant Viruses
Western Plant Diagnostic Network1 First Detector News A Quarterly Pest Update for WPDN First Detectors Spring 2015 edition, volume 8, number 2 In this Issue Page 1: Editor’s Note Dear First Detectors, Pages 2 – 3: Intro to Plant Plant viruses cause many important plant diseases and are Viruses responsible for huge losses in crop production and quality in Page 4: Virus nomenclature all parts of the world. Plant viruses can spread very quickly because many are vectored by insects such as aphids and Page 5 – Most Serious World Plant Viruses & Symptoms whitefly. They are a major pest of crop production as well as major pests of home gardens. By mid-summer many fields, Pages 6 – 7: Plant Virus vineyards, orchards, and gardens will see the effects of plant Vectors viruses. The focus of this edition is the origin, discovery, taxonomy, vectors, and the effects of virus infection in Pages 7 - 10: Grapevine plants. There is also a feature article on grapevine viruses. Viruses And, as usual, there are some pest updates from the West. Page 10: Pest Alerts On June 16 – 18, the WPDN is sponsoring the second Invasive Snail and Slug workshop at UC Davis. The workshop Contact us at the WPDN Regional will be recorded and will be posted on the WPDN and NPDN Center at UC Davis: home pages. Have a great summer and here’s hoping for Phone: 530 754 2255 rain! Email: [email protected] Web: https://wpdn.org Please find the NPDN family of newsletters at: Editor: Richard W. Hoenisch @Copyright Regents of the Newsletters University of California All Rights Reserved Western Plant Diagnostic Network News Plant Viruses 2 Ag, Manitoba Photo courtesy Photo Food, and Rural Initiatives and Food, of APS Photo by Giovanni Martelli, U of byBari Giovanni Photo Grapevine Fanleaf Virus Peanut leaf with Squash Mosaic Virus tomato spotted wilt virus Viruses are infectious pathogens that are too small to be seen with a light microscope, but despite their small size they can cause chaos. -
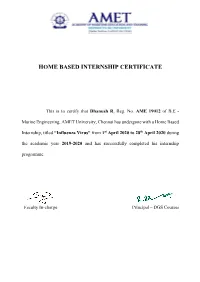
Home Based Internship Certificate
HOME BASED INTERNSHIP CERTIFICATE This is to certify that Dhanush R, Reg. No. AME 19012 of B.E - Marine Engineering, AMET University, Chennai has undergone with a Home Based Internship, titled “Influenza Virus” from 1st April 2020 to 28th April 2020 during the academic year 2019-2020 and has successfully completed his internship programme. Faculty In-charge Principal – DGS Courses INTERNSHIP AT HOME A Report On Internship In DEPARTMENT OF MARINE ENGINEERING By Name : Dhanush R Registration Number : AME19012 Year : 1ST Year Batch : BE(ME)-19 Group : 1 1 Influenza Virus SARS-CoV-2, a member of the family Coronaviridae A virus is a sub microscopic infectious agent that replicates only inside the living cells of an organism. Viruses can infect all types of life forms, from animals and plants to microorganisms, including bacteria and archaea. Since Dmitri Ivanovsky's 1892 article describing a non-bacterial pathogen infecting tobacco plants, and the discovery of the tobacco mosaic virus by Martinus Beijerinck in 1898, more than 6,000 virus species have been described in detail, of the millions of types of viruses in the environment. Viruses are found in almost every ecosystem on Earth and are the most numerous type of biological entity. The study of viruses is known as virology, a subspeciality of microbiology. When infected, a host cell is forced to rapidly produce thousands of identical copies of the original virus. When not inside an infected cell or in the process of infecting a cell, viruses exist in the form of independent particles, or virions, consisting of: (i) the genetic material, i.e. -

Lecture 7 Introduction to Viruses Introduction
Lecture 7 Introduction to Viruses Introduction Virus, parasite with a noncellular structure composed mainly of nucleic acid within a protein coat. Most viruses are too small (100–2,000 Angstrom units) to be seen with the light microscope and thus must be studied by electron microscopes. In one stage of their life cycle, in which they are free and infectious, virus particles do not carry out the functions of living cells, such as respiration and growth; in the other stage, however, viruses enter living plant, animal, or bacterial cells and make use of the host cell's chemical energy and its protein- and nucleic acid–synthesizing ability to replicate themselves. Over 5,000 species of viruses have been discovered. Discovery of Viruses In 1884 the French microbiologist Charles Chamberland invented a filter, known today as the Chamberland filter or Chamberland–Pasteur filter that has pores smaller than bacteria. Thus he could pass a solution containing bacteria through the filter and completely remove them from the solution. In the early 1890s the Russian biologist Dmitri Ivanovsky used this filter to study what became known as the tobacco mosaic virus. His experiments showed that extracts from the crushed leaves of infected tobacco plants remain infectious after filtration. At the same time several other scientists proved that, although these agents (later called viruses) were different from bacteria, they could still cause disease, and they were about one hundredth the size of bacteria. In 1899 the Dutch microbiologist Martinus Beijerinck observed that the agent multiplied only in dividing cells. Having failed to demonstrate its particulate nature he called it a "contagium vivum fluidum", a "soluble living germ". -

Synthetic Biology in Fine Art Practice. Doctoral Thesis, Northumbria University
Citation: Mackenzie, Louise (2017) Evolution of the Subject – Synthetic Biology in Fine Art Practice. Doctoral thesis, Northumbria University. This version was downloaded from Northumbria Research Link: http://nrl.northumbria.ac.uk/38387/ Northumbria University has developed Northumbria Research Link (NRL) to enable users to access the University’s research output. Copyright © and moral rights for items on NRL are retained by the individual author(s) and/or other copyright owners. Single copies of full items can be reproduced, displayed or performed, and given to third parties in any format or medium for personal research or study, educational, or not-for-profit purposes without prior permission or charge, provided the authors, title and full bibliographic details are given, as well as a hyperlink and/or URL to the original metadata page. The content must not be changed in any way. Full items must not be sold commercially in any format or medium without formal permission of the copyright holder. The full policy is available online: http://nrl.northumbria.ac.uk/policies.html EVOLUTION OF THE SUBJECT SYNTHETIC BIOLOGY IN FINE ART PRACTICE LOUISE MACKENZIE PhD 2017 EVOLUTION OF THE SUBJECT SYNTHETIC BIOLOGY IN FINE ART PRACTICE LOUISE MACKENZIE A thesis submitted in partial fulfilment of the requirements of the University of Northumbria at Newcastle for the degree of Doctor of Philosophy Research undertaKen in the Faculty of Arts, Design & Social Sciences in collaboration with the Institute of Genetic Medicine at Newcastle University December 2017 ABSTRACT AcKnowledging a rise in the use of synthetic biology in art practice, this doctoral project draws from vital materialist discourse on biotechnology and biological materials in the worKs of Donna Haraway, Jane Bennett, Rosi Braidotti and Marietta Radomska to consider the liveliness of molecular biological material through art research and practice. -

The Place of Viruses in Biology in Light of the Metabolism- Versus-Replication-First Debate
Hist. Phil. Life Sci., 34 (2012), 391-406 The Place of Viruses in Biology in Light of the Metabolism- versus-replication-first Debate Purificación López-García Unité d’Ecologie, Systématique et Evolution CNRS UMR8079, Université Paris-Sud 91405 Orsay, France ABSTRACT - The last decade has seen a revival of old virocentric ideas. These concepts are heterogeneous, extending from proposals that consider viruses functionally as living beings and/or as descendants of viral lineages that preceded cell evolution to other claims that consider viruses and/or some viral families a fourth domain of life. While the debates about whether viruses are alive or not and whether some virus-like replicators preceded the first cells fall under the long-lasting dichotomous view on the nature and origin of life (metabolism- versus replication-first), the claim that some giant viruses form a fourth domain in an organismal tree of life is not consistent with current evidence and can be falsified. KEYWORDS - Tree of life, metabolism, self-replication, origin of life, definition of life, giant viruses, horizontal gene transfer, evolution Introduction At the beginning of the twentieth century, the conditions for a scientific investigation into the origin of life on Earth were established. The rebuttal of continuous spontaneous generation by Louis Pasteur in the 1860s and the publication of On the Origin of Species in 1859 by Charles Darwin, led inevitably to the question of how the first life forms emerged. At the same time, immense progress in organic chemistry, biochemistry, cytology, and, among other advances, the discovery of the crucial importance of the cell nucleus, made it possible to approach a question that had remained until then too complex and intractable (Fry 2006). -

The History of Virology – the Scientific Study of Viruses and Therefore the Infections- Research Analysis of Virology and Retr
Current research in Virology & Retrovirology 2021, Vol.2, Issue 3 Short Communication The history of virology – the scientific study of viruses and therefore the infections- Research Analysis of Virology and Retrovirology Kwanighee Yonsei University, South Korea cholerae. Bacteriophages were heralded as a possible treatment for Copyright: 2021 Kwanighee . This is an open-access article distributed diseases like typhoid and cholera, but their promise was forgotten under the terms of the Creative Commons Attribution License, which with the event of penicillin. Since the early 1970s, bacteria have permits unrestricted use, distribution, and reproduction in any medium, continued to develop resistance to antibiotics such as penicillin, provided the original author and source are credited. and this has led to a renewed interest in the use of bacteriophages to treat serious infections. Early research 1920–1940, D'Herelle Abstract travelled widely to market the utilization of bacteriophages within the treatment of bacterial infections. In 1928, he became professor The history of virology – the scientific study of viruses and therefore of biology at Yale and founded several research institutes. He was the infections they cause – began within the closing years of the convinced that bacteriophages were viruses despite opposition 19th century. Although Pasteur and Jenner developed the primary from established bacteriologists such as the Nobel Prize winner vaccines to guard against viral infections, they didn't know that Jules Bordet (1870–1961). Bordet argued that bacteriophages viruses existed. The first evidence of the existence of viruses came from experiments with filters that had pores sufficiently small to were not viruses but just enzymes released from "lysogenic" retain bacteria. -

Viruses and Prokaryotes
DO NOT EDIT--Changes must be made through “File info” CorrectionKey=A Viruses and CHAPTER 18 Prokaryotes Big idea Viruses and some bacteria can be harmful to human health or the environment, but most bacteria and archaea are an important part of every community they inhabit. 18.1 Studying Viruses and Prokaryotes 4C data analysis ChoosiNg daTa rePreSeNTaTiON 2G 18.2 Viral Structure and reproduction 4C 18.3 Viral diseases 4C 18.4 Bacteria and archaea 8C 18.5 Beneficial roles of Prokaryotes 11C 18.6 Bacterial diseases and antibiotics 7F, 11C Online BiOlOgy HMDScience.com ONLiNe Labs ■■ Bacteria’s Role in Wastewater Treatment ■■ QuickLab Examining Bacteria in Yogurt ■■ Virtual Lab Testing Antibacterial Agents ■■ Leaf Print Bacteria ■■ Video Lab Bacterial Staining ■■ Using Bacteria to Break Down Oil ■■ Modeling Viruses ■■ S.T.e.M. Lab Modeling Viral Mutations ■■ Viruses and Cancer (t) ©Steve Gschmeissner/Photo Inc. Researchers, 526 Unit 6: Classification and Diversity DO NOT EDIT--Changes must be made through “File info” CorrectionKey=A Q how are bacteria helpful to humans? These bacteria live in the lining of an esophagus, the tube that leads from your mouth to your stomach. Only a few years ago, it was thought that nothing could survive in an esophagus, but the entire digestive tract is home for many types of bacteria. Being a home to bacteria isn’t bad, though. Some doctors hypothesize that these bacteria may protect us from some throat and stomach cancers. colored SEM; magnification unknown r e a d i N g T ool bo x This reading tool can help you learn the material in the following pages. -

Print Collection Flyer
IMPACT FACTOR 5.048 an Open Access Journal by MDPI Unconventional Viruses Collection Editor: Message from the Collection Editor Prof. Dr. Jean-Michel Claverie Dear Colleagues, Aix Marseille Univ, CNRS, IGS, Structural and Genomic Since its very beginning, with the serendipitous discovery Information Laboratory of the tobacco mosaic virus by Dmitri Ivanovsky in 1892, (UMR7256), Mediterranean Institute of Microbiology virology has mostly focused on those viruses responsible (FR3479), 163 Avenue de Luminy, for (oen dreadful) diseases of human, animals, or plants. F-13288 Marseille, France One noticeable exception was the study of bacteriophages jean-michel.claverie@ univ- that led to the basic concepts of modern cellular biology amu.fr and to many of today’s molecular biology tools. Through isolations or large-scale environmental metagenomic studies, a flurry of new viruses has since been uncovered that are considered unconventional due to their virion size and morphology, unusual gene contents, or exotic modes of replication. Beyond their unanticipated diversity, these “unconventional viruses” are challenging the established borders between the viral and cellular worlds as well as traditional views on the origin of life. This Special Issue will gladly welcome articles pertaining to any of these unconventional viruses, from virophages to multipartite RNA and DNA viruses, huge phages, archaeal viruses, giant DNA viruses, as well as to the emerging concept of virus-encoded metabolism. ion mdpi.com/si/44745 TopicaClollect on Collecti IMPACT FACTOR 5.048 an Open Access Journal by MDPI Editor-in-Chief Message from the Editor-in-Chief Dr. Eric O. Freed Viruses (ISSN 1999-4915) is an open access journal which Director, HIV Dynamics and provides an advanced forum for studies of viruses. -

Narrative Immunities: the Logic of Infection and Defense in American Speculative Fiction
Western University Scholarship@Western Electronic Thesis and Dissertation Repository 1-9-2018 11:30 AM Narrative Immunities: The Logic of Infection and Defense in American Speculative Fiction Riley R. McDonald The University of Western Ontario Supervisor Schuster, Joshua The University of Western Ontario Joint Supervisor Carmichael, Thomas The University of Western Ontario Graduate Program in English A thesis submitted in partial fulfillment of the equirr ements for the degree in Doctor of Philosophy © Riley R. McDonald 2018 Follow this and additional works at: https://ir.lib.uwo.ca/etd Part of the American Literature Commons Recommended Citation McDonald, Riley R., "Narrative Immunities: The Logic of Infection and Defense in American Speculative Fiction" (2018). Electronic Thesis and Dissertation Repository. 5174. https://ir.lib.uwo.ca/etd/5174 This Dissertation/Thesis is brought to you for free and open access by Scholarship@Western. It has been accepted for inclusion in Electronic Thesis and Dissertation Repository by an authorized administrator of Scholarship@Western. For more information, please contact [email protected]. Abstract In this project I analyze the roles that notions of viruses and immunities and their figurations play within the narrative discourse of speculative fiction. Focusing on a series of texts from twentieth- and twenty-first century American fiction, I seek to examine the ways in which the dialectical confrontation between infection and immunity is explored, reified, or challenged on a narrative level. The terms “virus” and “immunity,” so intrinsic to life sciences, have come into use to describe specific micro-organisms and biological processes only within the last 150 years. Yet these terms possess a significantly longer history in political, legalistic, and philosophical discourses. -

The KT Jeang Retrovirology Prize 2020: Tatyana Golovkina Retrovirology Editorial*
Retrovirology Editorial Retrovirology (2020) 17:21 https://doi.org/10.1186/s12977-020-00529-x Retrovirology EDITORIAL Open Access The KT Jeang Retrovirology prize 2020: Tatyana Golovkina Retrovirology Editorial* A native of Russia, Tatyana Golovkina graduated in 1985 Working at the Institute of Carcinogenesis, she continued with a MS in biology from Moscow State University her studies of virology, as many viruses of course were (Fig. 1). While it marked the beginning of an exciting and being studied for their roles in carcinogenesis. She joined fulflling journey into the world of scientifc research, it the lab of Irina Kryukova, a retrovirologist known for her was not the career path she and her family envisioned. work on the chicken retrovirus known as Rous Sarcoma Like many young people in the former USSR, Golovkina Virus. Golovkina credits Kryukova with teaching her that spent much of her youth training to become a pianist. in order to be successful as a scientist, you have to be Tis required countless hours of practice which became willing to be exploratory, as long as you are asking inter- increasingly difcult with the arrival of a baby sister in esting questions and follow the science wherever it may her family’s small apartment. To her family’s dismay, she lead. Golovkina also worked in the lab of Andrey Gudkov decided it would be better to pursue a diferent career as she continued her graduate studies on the evolution of and relegate piano to a hobby; the problem was that none endogenous retroviruses in the genomes of small mam- of them had envisioned anything else. -

Modernization of Control of Pathogenic Micro-Organisms in the Food-Chain Requires a Durable Role for Immunoaffinity-Based Detection Methodology—A Review
foods Review Modernization of Control of Pathogenic Micro-Organisms in the Food-Chain Requires a Durable Role for Immunoaffinity-Based Detection Methodology—A Review Aldert A. Bergwerff * and Sylvia B. Debast Laboratory of Clinical Microbiology and Infectious Diseases, Isala Hospital, Dr. van Heesweg 2, NL-8025 AB Zwolle, The Netherlands; [email protected] * Correspondence: [email protected] Abstract: Food microbiology is deluged by a vastly growing plethora of analytical methods. This review endeavors to color the context into which methodology has to fit and underlines the impor- tance of sampling and sample treatment. The context is that the highest risk of food contamination is through the animal and human fecal route with a majority of foodborne infections originating from sources in mass and domestic kitchens at the end of the food-chain. Containment requires easy-to-use, failsafe, single-use tests giving an overall risk score in situ. Conversely, progressive food-safety systems are relying increasingly on early assessment of batches and groups involving risk-based sampling, monitoring environment and herd/flock health status, and (historic) food- chain information. Accordingly, responsible field laboratories prefer specificity, multi-analyte, and high-throughput procedures. Under certain etiological and epidemiological circumstances, indirect antigen immunoaffinity assays outperform the diagnostic sensitivity and diagnostic specificity of Citation: Bergwerff, A.A.; Debast, e.g., nucleic acid sequence-based assays. The current bulk of testing involves therefore ante- and S.B. Modernization of Control of post-mortem probing of humoral response to several pathogens. In this review, the inclusion of Pathogenic Micro-Organisms in the immunoglobulins against additional invasive micro-organisms indicating the level of hygiene and Food-Chain Requires a Durable Role for Immunoaffinity-Based Detection ergo public health risks in tests is advocated. -

The Birth of Virology
Antonie van Leeuwenhoek 71: 15±20, 1997. 15 c 1997 Kluwer Academic Publishers. Printed in the Netherlands. The birth of virology Marian C. Horzinek Head, Virology Unit, Dept. Inf. Dis.& Immunol. Director, Institute of Veterinary Research, Veterinary Faculty, Utrecht University, Yalelaan 1, de Uithof, 3584 CL Utrecht, The Netherlands Si quis sit ea immanitatae naturae ut congressus haminum fugit atque oderit, tamen id pati non poterit ut non anquirat aliquem apud quem evomat virus acerbitatis suae Introduction Consequently, virology should occupy quite a prominent position in microbiological thinking, and This quote is from Cicero's `De Amicitia' (23, 87) it does world-wide. However, in paraphrasing the bib- Ð I happen to remember it from my days at school, lical `A prophet is not without honour, save in his own and it comes in conveniently to start a talk on the country' (New Testament; St. Matthew Chapter 13, birth of virology, my occupation since three decades. Verse 57) - concerning the hero we celebrate today it In Cicero's quote it is said of an intransigent person should read: `..., not even in his own country'. Beijer- that she `...still cannot be without somebody where to inck's importance for virology was barely mentioned spit out the venom of one's own bitterness' (Horzinek by the `NRC Handelsblad', a leading Dutch newspaper 1 1995). Throughout antiquity `virus' was a common, which ran a 1 /2 page article on him (November 30, general term to designate anything unpleasant and dan- 1995) at the occasion of this Centennial. Our Calvinist gerous, from snake and scorpion poison to disease heritage still shows.