ESCMID Online Lecture Library @ by Author Use of Antimalarials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Neena Valecha1, Deepali Savargaonkar1, Bina Srivastava1, B
Valecha et al. Malar J (2016) 15:42 DOI 10.1186/s12936-016-1084-1 Malaria Journal RESEARCH Open Access Comparison of the safety and efficacy of fixed‑dose combination of arterolane maleate and piperaquine phosphate with chloroquine in acute, uncomplicated Plasmodium vivax malaria: a phase III, multicentric, open‑label study Neena Valecha1, Deepali Savargaonkar1, Bina Srivastava1, B. H. Krishnamoorthy Rao2, Santanu K. Tripathi3, Nithya Gogtay4, Sanjay Kumar Kochar5, Nalli Babu Vijaya Kumar6, Girish Chandra Rajadhyaksha7, Jitendra D. Lakhani8, Bhagirath B. Solanki9, Rajinder K. Jalali10, Sudershan Arora10, Arjun Roy10, Nilanjan Saha10, Sunil S. Iyer10, Pradeep Sharma10 and Anupkumar R. Anvikar1* Abstract Background: Chloroquine has been the treatment of choice for acute vivax malaria for more than 60 years. Malaria caused by Plasmodium vivax has recently shown resistance to chloroquine in some places. This study compared the efficacy and safety of fixed dose combination (FDC) of arterolane maleate and piperaquine phosphate (PQP) with chloroquine in the treatment of uncomplicated vivax malaria. Methods: Patients aged 13–65 years with confirmed mono-infection of P. vivax along with fever or fever in the previ- ous 48 h were included. The 317 eligible patients were randomly assigned to receive FDC of arterolane maleate and PQP (n 159) or chloroquine (n 158) for 3 days. Primaquine was given as an anti-relapse measure on day 3 and continued= for 14 consecutive days.= Primary efficacy analysis included assessment of the proportion of aparasitaemic and afebrile patients at 72 h. Safety endpoints were analysis of adverse events, vital signs, laboratory data, and abnor- malities on electrocardiograph. Patients participated in the study for at least 42 days. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -

Review Article Efforts Made to Eliminate Drug-Resistant Malaria and Its Challenges
Hindawi BioMed Research International Volume 2021, Article ID 5539544, 12 pages https://doi.org/10.1155/2021/5539544 Review Article Efforts Made to Eliminate Drug-Resistant Malaria and Its Challenges Wote Amelo 1,2,3 and Eyasu Makonnen 1,2 1Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, Addis Ababa University, Addis Ababa, Ethiopia 2Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), Addis Ababa University, Addis Ababa, Ethiopia 3Department of Pharmacology and Toxicology, School of Pharmacy, Jimma University, Jimma, Ethiopia Correspondence should be addressed to Wote Amelo; [email protected] Received 21 January 2021; Accepted 9 August 2021; Published 30 August 2021 Academic Editor: Jane Hanrahan Copyright © 2021 Wote Amelo and Eyasu Makonnen. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Since 2000, a good deal of progress has been made in malaria control. However, there is still an unacceptably high burden of the disease and numerous challenges limiting advancement towards its elimination and ultimate eradication. Among the challenges is the antimalarial drug resistance, which has been documented for almost all antimalarial drugs in current use. As a result, the malaria research community is working on the modification of existing treatments as well as the discovery and development of new drugs to counter the resistance challenges. To this effect, many products are in the pipeline and expected to be marketed soon. In addition to drug and vaccine development, mass drug administration (MDA) is under scientific scrutiny as an important strategy for effective utilization of the developed products. -

Annual Review 2004 Contents Contentsforeword
Annual Review 2004 Contents ContentsForeword ........................................................................................................................... 3 Editor’s Note ..................................................................................................................... 4 Organization Chart ............................................................................................................ 5 Administrative Board .......................................................................................................... 6 Special Events..................................................................................................................... 8 Consultants ...................................................................................................................... 13 Visiting Professors ............................................................................................................ 13 Faculty Board ...................................................................................................................13 Faculty Senate ..................................................................................................................14 Department of Clinical Tropical Medicine ........................................................................ 15 Department of Helminthology ......................................................................................... 22 Department of Medical Entomology ............................................................................... -

Update Tot 30-04-2020 1. Chloroquine and Hydroxychloroquine for The
Update tot 30-04-2020 1. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of Novel Coronavirus Disease (COVID-19) in Africa: Caution for Inappropriate Off-Label Use in Healthcare Settings. Abena PM, Decloedt EH, Bottieau E, Suleman F, Adejumo P, Sam-Agudu NA, et al. Am j trop med hyg. 2020. 2. Evaluation of Hydroxychloroquine Retinopathy Using Ultra-Widefield Fundus Autofluorescence: Peripheral Findings in the Retinopathy. Ahn SJ, Joung J, Lee BR. American journal of ophthalmology. 2020;209:35-44. http://dx.doi.org/10.1016/j.ajo.2019.09.008. Epub 2019 Sep 14. 3. COVID-19 research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine. Alexander PE, Debono VB, Mammen MJ, Iorio A, Aryal K, Deng D, et al. J clin epidemiol. 2020. 4. Chloroquine and Hydroxychloroquine in the Era of SARS - CoV2: Caution on Their Cardiac Toxicity. Bauman JL, Tisdale JE. Pharmacotherapy. 2020. 5. Repositioned chloroquine and hydroxychloroquine as antiviral prophylaxis for COVID-19: A protocol for rapid systematic review of randomized controlled trials. Chang R, Sun W-Z. medRxiv. 2020:2020.04.18.20071167. 6. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Colson P, Rolain J-M, Lagier J-C, Brouqui P, Raoult D. Int J Antimicrob Agents. 2020:105932-. 7. Dose selection of chloroquine phosphate for treatment of COVID-19 based on a physiologically based pharmacokinetic model. Cui C, Zhang M, Yao X, Tu S, Hou Z, Jie En VS, et al. Acta Pharmaceutica Sinica B. 2020. 8. Hydroxychloroquine; Why It Might Be Successful and Why It Might Not Be Successful in the Treatment of Covid-19 Pneumonia? Could It Be A Prophylactic Drug? Deniz O. -
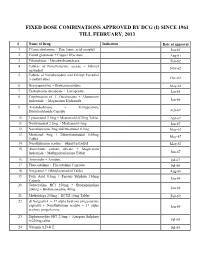
Fixed Dose Combinations Approved by Dcg (I) Since 1961 Till February, 2013
FIXED DOSE COMBINATIONS APPROVED BY DCG (I) SINCE 1961 TILL FEBRUARY, 2013 # Name of Drug Indication Date of approval 1. Cyanocobalamine + Zinc tannic acid complex Jan-61 2. Cobalt glutamate + Copper Glycinate Aug-61 3. Fibrinolysin + Desoxyribonuclease Feb-62 4. Tablets of Norethisterone acetate + Ethinyl Nov-62 oestradiol 5. Tablets of Norethynodrel and Ethinyl Estradiol 3-methyl ether Dec-62 6. Broxyquinoline + Brobenzoxalidine May-63 7. Testosterone decanoate + Isocaproate Jan-64 8. Combination of L Oxethazaine + Aluminium hydroxide + Magnesium Hydroxide Jun-66 9. Amylobarbitone + Trifluperazine Dihydrochloride Capsule Feb-67 10. Lynestronol 2.5mg + Mestranol 0.075mg Tablet Apr-67 11. Northynodrel 2.5mg + Mestranol 0.1mg Jun-67 12. Norethisterone 2mg and Mestranol 0.1mg May-67 13. Mestranol 4mg + Ethinyloestradial 0.05mg May-67 Tablet 14. Norethisterane acetate + ethinyl estradiol May-67 15. Aluminium sodium silicate + Magnesium hydroxide + Methypolysiloxane Tablet Jun-67 16. Ammoidin + Amidine Jul-67 17. Fluocortolene + Flucortolene Caproate Jul-68 18. Norgestrel + Ethinyloestradiol Tablet Aug-68 19. Folic Acid 0.5mg + Ferrous Sulphate 150mg Jan-69 Capsule 20. Tetracycline HCl 250mg + Broxyquinoline 200mg + Brobenzoxadine 40mg Jan-69 21. Methyldopa 250mg + HCTZ 15mg Tablet Feb-69 22. dl Norgestrel + 17 alpha hydroxy progesterone caproate + Norethisterone acetate + 17 alpha Jan-69 acetoxy progesterone 23. Diphenoxylate HCl 2.5mg + Atropine Sulphate 0.025mg tablet Jul-69 24. Vitamin A,D & E Jul-69 25. Lutin 0.1gm + Vit 0.1gm + Vit K1 2.5mg + Dicalcium Phosphate 0.1gm + Carlozochrome Jul-69 Salicylate 1mg tablet 26. Vit K 1 5mg + Calcium Lactolionate 100 m g+ Carlozocrome Salicylate 2.5mg + Phenol 0.5% Jul-69 + Lignocaine Hcl 1% injection 27. -
Quinoline-Based Hybrid Compounds with Antimalarial Activity
molecules Review Quinoline-Based Hybrid Compounds with Antimalarial Activity Xhamla Nqoro, Naki Tobeka and Blessing A. Aderibigbe * Department of Chemistry, University of Fort Hare, Alice Campus, Alice 5700, Eastern Cape, South Africa; [email protected] (X.N.); [email protected] (N.T.) * Correspondence: [email protected] Received: 7 November 2017; Accepted: 11 December 2017; Published: 19 December 2017 Abstract: The application of quinoline-based compounds for the treatment of malaria infections is hampered by drug resistance. Drug resistance has led to the combination of quinolines with other classes of antimalarials resulting in enhanced therapeutic outcomes. However, the combination of antimalarials is limited by drug-drug interactions. In order to overcome the aforementioned factors, several researchers have reported hybrid compounds prepared by reacting quinoline-based compounds with other compounds via selected functionalities. This review will focus on the currently reported quinoline-based hybrid compounds and their preclinical studies. Keywords: 4-aminoquinoline; 8-aminoquinoline; malaria; infectious disease; hybrid compound 1. Introduction Malaria is a parasitic infectious disease that is a threat to approximately half of the world’s population. This parasitic disease is transmitted to humans by a female Anopheles mosquito when it takes a blood meal. Pregnant women and young children in the sub-tropical regions are more prone to malaria infection. In 2015, 214 million infections were reported, with approximately 438,000 deaths and the African region accounted for 90% of the deaths [1–3]. Malaria is caused by five parasites of the genus Plasmodium, but the majority of deaths are caused by Plasmodium falciparum and Plasmodium vivax [1,4–6]. -

Review of Mass Drug Administration and Primaquine
Contents Acknowledgements ...................................................................................................................................... 2 Acronyms ...................................................................................................................................................... 3 Introduction .................................................................................................................................................. 4 Methods ....................................................................................................................................................... 4 Findings ......................................................................................................................................................... 6 Study objectives and design ............................................................................................................ 9 Contextual parameters - endemicity, seasonality, target population .......................................... 10 Outcome measures ....................................................................................................................... 13 Drug regimens ............................................................................................................................... 13 Co-Interventions ............................................................................................................................ 15 Delivery methods and community engagement .......................................................................... -

1 Antimalarial Activity of the 8 - Aminoquinolines Edward A
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln US Army Research U.S. Department of Defense 1991 1 Antimalarial Activity of the 8 - Aminoquinolines Edward A. Nodiff Franklin Research Center, Arvin Calspan Corporation, Valley Forge Corporate Center, Norristown, PA Sankar Chatterjee Department of Medicinal Chemistry, Division of Experimental Therapeutics, Walter Reed Army Institute of Research, Walter Reed Army Medical Center, Washington, DC Hikmat A. Musallam Department of Medicinal Chemistry, Division of Experimental Therapeutics, Walter Reed Army Institute of Research, Walter Reed Army Medical Center, Washington, DC Follow this and additional works at: http://digitalcommons.unl.edu/usarmyresearch Nodiff, Edward A.; Chatterjee, Sankar; and Musallam, Hikmat A., "1 Antimalarial Activity of the 8 - Aminoquinolines" (1991). US Army Research. 337. http://digitalcommons.unl.edu/usarmyresearch/337 This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in US Army Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Progress in Medicinal Chemistry - Vol. 28, edited by G.P. Ellis and G.B. West 0 1991, Elsevier Science Publishers, B.V. 1 Antimalarial Activity of the 8- Aminoquinoline s EDWARD A. NODIFF, B.A. SANKAR CHATTERJEE, Ph.D. and HIKMAT A. MUSALLAM, Ph.D.2 Franklin Research Center, Arvin Calspan Corporation, Valley Forge Corporate Center, 2600 Monroe Boulevard, Norristown, PA 19403 and 'Department of Medicinal Chemistry, Division of Experimental Therapeutics, Walter Reed Army Institute of Research, Walter Reed Army Medical Center, Washington, DC 20307-5100, U.S.A. INTRODUCTION 2 THE PARASITE Exoerythrocytic phase Erythrocytic phase Sporogony THE DISEASE 4 CLASSIFICATION OF ANTIMALARIAL DRUGS 4 HISTORY 5 METHODS FOR ANTIMALARIAL DRUG EVALUATION 8 Rane blood schizontocidal screen (P. -

Pyrimethamine and Proguanil Are the Two Most Widely Used DHFR Inhibitor Antimalarial Drugs. Cycloguanil Is the Active Metabolite of the Proguanil (1,2)
Jpn. J. Med. Sci. Biol., 49, 1-14, 1996. IN VITRO SELECTION OF PLASMODIUM FALCIPARUM LINES RESISTANT TO DIHYDROFOLATE-REDUCTASE INHIBITORS AND CROSS RESISTANCE STUDIES Virendra K. BHASIN* and Lathika NAIR Department of Zoology, University of Delhi, Delhi 110007, India (Received July 27, 1995. Accepted November 6, 1995) SUMMARY: A cloned Plasmodium falciparum line was subjected to in vitro drug pressure, by employing a relapse protocol, to select progressively resistant falciparum lines to pyrimethamine and cycloguanil, the two dihydrofolate- reductase (DHFR) inhibitor antimalarial drugs. The falciparum lines resistant to pyrimethamine were selected much faster than those resistant to cycloguanil. In 348 days of selection/cultivation, there was 2,400-fold increase in IC50 value to pyrimethamine, whereas only about 75-fold decrease in sensitivity to cycloguanil was registered in 351 days. Pyrimethamine-resistant parasites acquired a degree of cross resistance to cycloguanil and methotrexate, another DHFR inhibitor, but did not show any cross resistance to some other groups of antimalarial drugs. The highly pyrimethamine-resistant line was not predisposed for faster selection to cycloguanil resistance. Resistance acquired to pyrimethamine was stable. The series of resistant lines obtained form a good material to study the •eevolution•f of resistance more meaningfully at molecular level. INTRODUCTION Pyrimethamine and proguanil are the two most widely used DHFR inhibitor antimalarial drugs. Cycloguanil is the active metabolite of the proguanil (1,2). There is abundant evidence to indicate that the pyrimethamine resistance is now widely distributed throughout malaria-endemic areas of the world (3-5). The incidence of the proguanil resistance appears to be in doubt and *To whom correspondence should be addressed . -
Sustaining Antimalarial Drug Development
Review TRENDS in Parasitology Vol.22 No.7 July 2006 Medicines for Malaria Venture: sustaining antimalarial drug development Ian Bathurst and Chris Hentschel Medicines for Malaria Venture (MMV), International Center Cointrin (ICC) Building, 20 rte de Pre´ -Bois, 1215 Geneva 15, Switzerland The Medicines for Malaria Venture (MMV) is committed Between 75% and 90% of malaria cases are currently to discovering, developing and delivering new drugs for found in sub-Saharan Africa but global warming and malaria. Founded in 1999 as a nonprofit organization demographic changes could change this. Both warming bringing private sector management methods to bear and increased flooding are conditions that favor the spread on a global public health problem, MMV is today of the mosquito species that transmits malaria, thus recognized as a leader among the public–private increasing the possibility that malaria will return to partnerships working on diseases for the developing parts of Europe and the USA [5,6]. world. Together with its many partners, MMV manages PPPs have rapidly evolved as the preferred way to the world’s largest malaria research and development ensure that progress can be made in addressing health- portfolio, covering the innovation spectrum from basic care issues that neither the public nor the private sector drug discovery to late-stage development. can solve on their own. MMV, incorporated as a Swiss foundation and officially launched on 3 November 1999, Introduction to MMV was among the first PPPs established to tackle the drug The Medicines for Malaria Venture (MMV; www.mmv.org) innovation gap of a major global neglected disease. -

PHARMACOLOGY of NEWER ANTIMALARIAL DRUGS: REVIEW ARTICLE Bhuvaneshwari1, Souri S
REVIEW ARTICLE PHARMACOLOGY OF NEWER ANTIMALARIAL DRUGS: REVIEW ARTICLE Bhuvaneshwari1, Souri S. Kondaveti2 HOW TO CITE THIS ARTICLE: Bhuvaneshwari, Souri S. Kondaveti. ‖Pharmacology of Newer Antimalarial Drugs: Review Article‖. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 4, January 26, 2015; Page: 431-439. ABSTRACT: Malaria is currently is a major health problem, which has been attributed to wide spread resistance of the anopheles mosquito to the economical insecticides and increasing prevalence of drug resistance to plasmodium falciparum. Newer drugs are needed as there is a continual threat of emergence of resistance to both artemisins and the partner medicines. Newer artemisinin compounds like Artemisone, Artemisnic acid, Sodium artelinate, Arteflene, Synthetic peroxides like arterolane which is a synthetic trioxolane cognener of artemisins, OZ439 a second generation synthetic peroxide are under studies. Newer artemisinin combinations include Arterolane(150mg) + Piperaquine (750mg), DHA (120mg) + Piperaquine(960mg) (1:8), Artesunate + Pyronardine (1:3), Artesunate + Chlorproguanil + Dapsone, Artemisinin (125mg) + Napthoquine (50mg) single dose and Artesunate + Ferroquine.Newer drugs under development including Transmission blocking compounds like Bulaquine, Etaquine, Tafenoquine, which are primaquine congeners, Spiroindalone, Trioxaquine DU 1302, Epoxamicin, Quinolone 3 Di aryl ether. Newer drugs targeting blood & liver stages which include Ferroquine, Albitiazolium – (SAR – 97276). Older drugs with new use in malaria like beta blockers, calcium channel blockers, protease inhibitors, Dihydroorotate dehydrogenase inhibitors, methotrexate, Sevuparin sodium, auranofin, are under preclinical studies which also target blood and liver stages. Antibiotics like Fosmidomycin and Azithromycin in combination with Artesunate, Chloroquine, Clindamycin are also undergoing trials for treatment of malaria. Vaccines - RTS, S– the most effective malarial vaccine tested to date.