NALANDA Preface
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ground Water Year Book, Bihar (2015 - 2016)
का셍ााल셍 उप셍ोग हेतू For Official Use GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD जल ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पूर्वी क्षेत्र, पटना सितंबर 2016 MID-EASTERN REGION, PATNA September 2016 ` GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES जल CENTRAL GROUND WATER BOARD ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पर्वू ी क्षेत्र, पटना MID-EASTERN REGION, PATNA सितंबर 2016 September 2016 GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) CONTENTS CONTENTS Page No. List of Tables i List of Figures ii List of Annexures ii List of Contributors iii Abstract iv 1. INTRODUCTION.............................................................................................................1 2. HYDROGEOLOGY..........................................................................................................1 3. GROUND WATER SCENARIO......................................................................................4 3.1 DEPTH TO WATER LEVEL........................................................................................8 3.1.1 MAY 2015.....................................................................................................................8 3.1.2 AUGUST 2015..............................................................................................................10 3.1.3 NOVEMBER 2015........................................................................................................12 3.1.4 JANUARY 2016...........................................................................................................14 -

41629-013: Bihar State Highways II Project
Social Monitoring Report Project Number: 41629-013 / 44425-013 September 2019 Period: January 2018 – June 2018 IND: Bihar State Highway II Project SH – 78 Submitted by Bihar State Road Development Corporation Limited, Patna This social monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Bihar State Highway Project Phase – II CONTRACT PACKAGE NO.1& 2 (SH-78) (Bihta – Sarmera) Monitoring and Implementation of Resettlement Plan (RP) Semi Annual Report January 2018 - June 2018 Submitted By Egis International S.A in JV with Egis India Consulting Engineers Pvt. Ltd. Plot No.66, Sec.32 Gurgaon-122001 CONTENTS Abbreviation ................................................................................................................................................... 2 GLOSSARY ...................................................................................................................................................... 3 1. PROJECT BACKGROUND ........................................................................................................................... 4 2. PROJECT DESCRIPTION .......................................................................................................................... -

Womens' Empowerment
Directory of Voluntary Organisations Women’s Empowerment 2010 Documentation Centre for Women and Children (DCWC) National Institute of Public Cooperation and Child Development 5, Siri Institutional Area, Hauz Khas, New Delhi – 110016 Number of Copies: 100 Copyright: National Institute of Public Cooperation and Child Development, 2010 Project Team Project In-charge : Mrs. Meenakshi Sood Project Team : Ms. Renu Banker Ms. Alpana Kumari Computer Assistance : Mrs. Sandeepa Jain Mr. Abhishek Tiwari Acknowledgements : Ministry of Women and Child Development Planning Commission Voluntary Organisations Ministry of Rural Development Ministry of Panchayati Raj Ministry of Tribal Affairs Ministry of Urban Development DISCLAIMER All efforts have been made to verify and collate information about organisations included in the Directory. Information has been collected from various sources, namely directories, newsletters, Internet, proforma filled in by organisations, telephonic verification, letter heads, etc. However, NIPCCD does not take any responsibility for any error that may inadvertently have crept in. The address of offices of organisations, telephone numbers, e-mail IDs, activities, etc. change from time to time, hence NIPCCD may not be held liable for any incorrect information included in the Directory. Foreword Voluntary organisations play a very important role in society. They take up activities in the area of their expertise and provide support to the community in whose welfare they have interest. Social development has been ranked high on the priority list of Government programmes since Independence, and voluntary organisations have been equal partners in accelerating the pace of development. Being in close proximity to the community, voluntary organisations have done pioneering work in many areas, rendered productive services, highlighted several social problems, undertaken advocacy, and lobbied for the rights of the underprivileged. -

Provisional Population Totals, Series-11, Bihar
CENSUS OF INDIA 2001 SERIES- 11 BIHAR PAPER 1 OF 2001 PROVISIONAL POPULATION TOTALS SUDHIR KUMAR RAKESH Director of Census Operations, Bihar Lord Buddha Dedicated to the people of Bihar and enumerators - the data producers. For the benefit of policy makers and research workers - the data consumers. CONTENTS SL. NO. PARTICULARS PAGE NO. 1. Foreword v 2 List of Officers! Officials involved in preparation of Provisional Population Totals vii 3 Figures at a Glance ix 4 State Highlights x 5 Map showing Administrative Division of India Highlighting State xi 6 Map showing Administrative Division of State, 2001 Census xiii 7 Introduction 1 8 Analysis of Results 7· 9 Provisional Population Tables 25 10 Maps 31 11 Diagrams and Charts 39 12 Organisational Chart of Census Hierarchy 49 13 Specimen Copy of Houselist Schedule 51 - 14 Specimen Copy of Household Schedule 53 15 Pictorial 55 FOREWORD After the successful completion of Census of India 2001, it gives me great pleasure to present these provisional population totals for the state of Bihar. This paper gives some basic characteristics of the population of Bihar as on 1st March, 2001 (00.00 hrs.) as recorded during the population enumeration related with the Census of India 2001. These figures are only provisional ones, compiled on the basis of the abstracts of population data prepared by the enumerators. These provisional population figures are being published with the intention of meeting the immediate need of the Government, various organisations, researchers and the general public. It would help provide them the basic population figures as quickly as possible after the population enumeration work has been completed. -
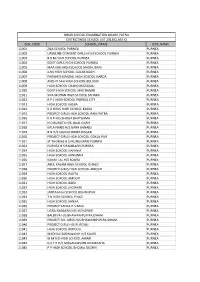
Sch Code School Name Dist Name 11001 Zila School
BIHAR SCHOOL EXAMINATION BOARD PATNA DISTRICTWISE SCHOOL LIST 2013(CLASS X) SCH_CODE SCHOOL_NAME DIST_NAME 11001 ZILA SCHOOL PURNEA PURNEA 11002 URSULINE CONVENT GIRLS HIGH SCHOOL PURNEA PURNEA 11003 B B M HIGH SCHOOL PURNEA PURNEA 11004 GOVT GIRLS HIGH SCHOOL PURNEA PURNEA 11005 MAA KALI HIGH SCHOOL MADHUBANI PURNEA 11006 JLNS HIGH SCHOOL GULAB BAGH PURNEA 11007 PARWATI MANDAL HIGH SCHOOL HARDA PURNEA 11008 ANCHIT SAH HIGH SCHOOL BELOURI PURNEA 11009 HIGH SCHOOL CHANDI RAZIGANJ PURNEA 11010 GOVT HIGH SCHOOL SHRI NAGAR PURNEA 11011 SIYA MOHAN HIGH SCHOOL SAHARA PURNEA 11012 R P C HIGH SCHOOL PURNEA CITY PURNEA 11013 HIGH SCHOOL KASBA PURNEA 11014 K D GIRLS HIGH SCHOOL KASBA PURNEA 11015 PROJECT GIRLS HIGH SCHOOL RANI PATRA PURNEA 11016 K G P H/S BHOGA BHATGAMA PURNEA 11017 N D RUNGTA H/S JALAL GARH PURNEA 11018 KALA NAND H/S GARH BANAILI PURNEA 11019 B N H/S JAGNICHAMPA NAGAR PURNEA 11020 PROJECT GIRLS HIGH SCHOOL GOKUL PUR PURNEA 11021 ST THOMAS H S MUNSHIBARI PURNEA PURNEA 11023 PURNEA H S RAMBAGH,PURNEA PURNEA 11024 HIGH SCHOOL HAFANIA PURNEA 11025 HIGH SCHOOL KANHARIA PURNEA 11026 KANAK LAL H/S SOURA PURNEA 11027 ABUL KALAM HIGH SCHOOL ICHALO PURNEA 11028 PROJECT GIRLS HIGH SCHOOL AMOUR PURNEA 11029 HIGH SCHOOL RAUTA PURNEA 11030 HIGH SCHOOL AMOUR PURNEA 11031 HIGH SCHOOL BAISI PURNEA 11032 HIGH SCHOOL JHOWARI PURNEA 11033 JANTA HIGH SCHOOL BISHNUPUR PURNEA 11034 T N HIGH SCHOOL PIYAZI PURNEA 11035 HIGH SCHOOL KANJIA PURNEA 11036 PROJECT KANYA H S BAISI PURNEA 11037 UGRA NARAYAN H/S VIDYAPURI PURNEA 11038 BALDEVA H/S BHAWANIPUR RAJDHAM -
Initial Environmental Examination: India, Bihar Power System
Environmental Assessment Report Final Initial Environmental Examination Project Number: 41626 August 2010 IND: Bihar Power System Improvement Project The Final environmental examination report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. Government of Bihar Bihar State Electricity Board BIHAR POWER SYSTEM IMPROVEMENT PROJECT FINAL REPORT INITIAL ENVIRONMENTAL EXAMINATION DISTRIBUTION COMPONENT AUGUST 2010 ASIAN DEVELOPMENT BANK GOVERNMENT OF BIHAR COPYRIGHT: The concepts and information contained in this document are the property of government of Bihar & Asian Development Bank. Use or copying of this document in whole or in part without the written permission of either Government of Bihar or Asian Development Bank constitutes an infringement of copyright. Bihar Power System Improvement Project FINAL REPORT INITIAL ENVIRONMENTAL EXAMINATION BIHAR POWER SYSTEM IMPROVEMENT PROJECT DISTRIBUTION COMPONENT Contents EXECUTIVE SUMMARY vi A. Assessment of Legal Framework and Policy vi B. Anticipated Environmental Impacts vii C. Environmental Assessment for the Project x D. Environment Management Plan xi E. Institutional Arrangements and Responsibilities xiv F. Monitoring and Reporting xiv G. Public Consultation and Information Disclosure xv H. Grievance Redress Mechanism xv 1 INTRODUCTION 1 1.1 Overview 1 1.2 Project Goal and Objective 2 1.3 Purpose of IEE Study 2 1.4 Scope of the IEE 2 1.5 Report Structure 2 2 POLICY -

List of 1833 Candidates Debarred by RRC/ECR in Last Four Recruitment
East Central Railway (Railway Recruitment Cell) Polson Complex, Digha Ghat, Patna – 11 Telephone No. 0612-2560029, 2560035 Website: www.rrcecr.gov.in Email: [email protected] Notice No. 02/2016 dated 08.02.2016 List of 1833 candidates debarred by RRC/ECR in last 4 recruitments (ENN-01/07 (Gr. ‘D’), RRC/ECR/Group-D/1/2010, RRC/ECR/GP1800/1/2012 & RRC/ECR/GP1800/1/2013 1833 Candidates were found indulged in arranging impersonation in the last 4 recruitments (Employment Notice No- 01/07 Gr.‘D’, RRC/ECR/Group- D/1/2010, RRC/ECR/GP1800/1/2012 & RRC/ECR/GP1800/1/2013). So in terms of Railway Board’s letter No. E(RRB)/2001/25/1 dt. 14.02.02 & E(RRB)/2004/16/6 dt. 02.02.05, 1833 candidates have been debarred by RRC/ECR from all RRBs/RRCs examination for life time on the ground of impersonation. This action has been taken after adverse report against them in forsensic examination (Finger Print Expert/ Government Examiner of Questionable Documents) and after giving them show cause notice. The concerned candidates have alredy been suitably informed through separate letters. The Employment Notice-wise break-up of candidates is as under: Sl.No Employment Notice No Number of candidates debarred 1 01/07 (Gr. ‘D’) 901 2 RRC/ECR/Group-D/1/2010 524 3 RRC/ECR/GP1800/1/2012 229 4 RRC/ECR/GP1800/1/2013 179 TOTAL 1833 Chairman Railway Recruitment Cell, East Central Railway Combined list of ( 901+524+229+179) Total-1833 candidates debarred for life by RRC/ECR pertaining to Employment Notice No. -

Agricultural Development in Bihar
t: PAL AGRICUL TURAL DEVELOPMENT IN BIHAR ,... I I ,I ,'V'-I Challenges Fig. 2.1: Trends in Productivity of Foodgrains in Bihar and India & 2~.-~------------------~------- Opportunities 000 - .t:. ~~----~~------------~~ x -:2 >- 000r----------------------------- By 500 T. Haque :I Q Council for Social Development New Delhi • • • [~ ..- ~ AGRICULTURAL DEVELOPMENT IN BIHAR CHALLENGES AND OPPORTUNITIES By T. HAQUE About the author Dr. T. Haque is a well known Agricultural Economist. He is currently Director, Council for Social Development, New Delhi, Senior Adviser, LANDESA (Rural Development Institute), New Delhi, and Vice-Chairman, Council for Development of Bihar and Jharkhand, New Delhi. Earlier he served as Chairman, Commission for Agricultural Costs and Prices, Govt. of India, ICAR National Fellow at the National Centre for Agricultural Economics and Policy Research, New Delhi and Director, Centre for Agrarian Studies, NIRD, Hyderabad and Senior Scientist at the Indian Agricultural Research Institute, New Delhi. His email [email protected] Acknowledgements The author is grateful to Dr. P.K. Joshi, Director, IFPRI in South Asia, New Delhi for his help and support in preparing an earlier research report, based on which this Policy paper has been produced. The help received from Gaurav Tripathi of IFPRI in South Asia and Gitesh Sinha of CSD, New Delhi in compilation of data is also thankfully acknowledged. T. Haque CONTENT Page No. 1.0 Overview 1 2.0 Agricultural Growth and Variability 6 2.1 Crop Production 6 2.2 Horticulture 12 -
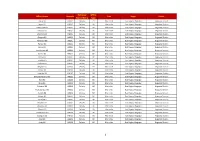
Office Name Pincode Delivery
Delivery/ Office Office Name Pincode Circle Region Division Non Delivery Type BBazar SO 848201 Delivery PO Bihar Circle East Region, Bhagalpur Begusarai Division Bagras BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Chak Hamid BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Deopura BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Gamharia BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Ghagrha BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Mohanpur BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Rampur BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Samsa BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Sital Rampur BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Sonihar BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Sonma BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Sumbha BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Parihara BO 848201 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Meghaul SO 848202 Delivery PO Bihar Circle East Region, Bhagalpur Begusarai Division Akopur BO 848202 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Amaridih BO 848202 Delivery BO Bihar circle East Region, Bhagalpur Begusarai Division Bariarpurtola Sirsi BO 848202 Delivery -

Droughts, Distress and a Conditional Cash Transfer Program to Mitigate the Impact of Drought in Bihar, India
Droughts, Distress and a Conditional Cash Transfer Program to Mitigate the Impact of Drought in Bihar, India Avinash Kishore ([email protected]), PK Joshi ([email protected]) and Divya Pandey ([email protected]) International Food Policy Research Institute NASC Complex, CG Block Dev Prakash Shastri Road (Opp. Todapur) Pusa, New Delhi 110012 India Fax: +91 11 2584.8008 / 2584.657 Abstract Paddy—Bihar’s staple crop—is vulnerable to droughts, primarily due to high cost of irrigation. In 2008, Bihar government launched a conditional cash transfer scheme to subsidise diesel for irrigation in drought affected areas. We show that this scheme has not been effective in mitigating the impact of drought on paddy production. A primary survey of potential and actual beneficiaries shows that low awareness and penetration among smallholders, alongside uncertainties and delays in the disbursal of the subsidy, make it ineffective. We suggest that in states with limited capacity, such ad-hoc subsidies are unlikely to protect smallholders from weather shocks. 1 1. Introduction Agriculture in India has always been vulnerable to the vagaries of monsoon (Kumar et al., 2004). The rainfall related volatility in agricultural production is a big concern for food security, economic development, and household welfare in India and other tropical countries (Rosenzweig & Hillel, 2008; World Bank, 2007). These concerns have grown in recent years as altered rainfall patterns have become frequent, resulting in short run crop failures and long run production declines. Bihar, the third largest and the poorest state of India, has been facing such heightened concerns in recent yearsi. -
Annual Report Nalanda University
Annual Report Nalanda University 2010-2011 & 2011-2012 NEW DELHI OFFICE 2st Floor, Council for Social Development Sangha Rachna, 53, Lodhi Estate, New Delhi – 110 003 Tel. +91-11 24618352, +91-11 26172328 Fax: +91-11 24618351 RAJGIR OFFICE Rajgir, District Nalanda, Pin: 803 115 Bihar, India www.nalandauniv.edu.in Annual Report 2010-2011 & 2011-2012 CONTENTS Foreword 1 Nalanda University: Past & Present 2 Governing Board 10 Vision Statement 13 Our Logo and Identity 15 Chairperson’s Message 17 Vice Chancellor’s Report 22 Academic Planning 39 Financial Management 45 Campus 47 Officers and Employees 50 NEW DELHI OFFICE 2st Floor, Council for Social Development Sangha Rachna, 53, Lodhi Estate, New Delhi – 110 003 Tel. +91-11 24618352, +91-11 26172328 Fax: +91-11 24618351 RAJGIR OFFICE Rajgir, District Nalanda, Pin: 803 115 Bihar, India www.nalandauniv.edu.in Foreword We are pleased to present the first Annual Report of Nalanda University. The report covers the period November 2010 to March 2012, i.e. part of the financial year 2010-2011 and the full financial year 2011-2012. The report outlines in detail the developments at Nalanda University in addition to providing a vision statement. Further, it also provides a brief historical background of ancient Nalanda University and its revival as a modern University in November 2010. The Annual Report comprises a message from the Chairperson and reports from the Vice Chancellor, the Officer on Special Duty (OSD) University Development and Academic Affairs and Officer on Special Duty (OSD) Finance on various aspects of the development of the University. -
Technical Assistance Consultant's Report
Technical Assistance Consultant’s Report Project Number: 43166-062 May 2013 India: Advanced Project Preparedness for Poverty Reduction - Institutional Development for a Value Chain Approach to Agribusiness in Bihar (Financed by the Government of the United Kingdom) Prepared by IL&FS Cluster Development Initiative Ltd. In collaboration with Agrifood Consulting International For Bihar Department of Agriculture This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. Advanced Project Preparedness for Poverty Reduction - Institutional Development for a Value Chain Approach to Agribusiness in Bihar (Contract No. : 100146-S41802) Final Report Submitted to: Asian Development Bank Prepared by: In collaboration with: Agrifood Consulting International 1 Knowledge Summary ....................................................................................... 10 1. Introduction .................................................................................................. 13 1.1 Background - Technical Assistance Programme ................................. 13 1.2 Approach of TA Programme ................................................................. 14 1.2.1 Field Survey .................................................................................... 14 1.2.2 Stakeholders’ Consultations ......................................................... 15 1.2.3 Capacity Building Initiatives .......................................................