TUCOM 2016-2020 Residency Match Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COMLEX-USA for Residency Program Directors
COMLEX-USA FOR RESIDENCY PROGRAM DIRECTORS COMLEX-USA Evidence–based assessment designed specifically for osteopathic medical students and residents that measures competencies required for the provision of safe and effective osteopathic medical care to patients. It is recommended but not required that COMLEX-USA Level 3 be taken after a minimum of six months in residency. The attestation process for COMLEX-USA Level 3 helps to fulfill the NBOME mission to DO candidates are not required to pass the United States protect the public, and adds value and entrustability to state licensing Medical Licensing Examination (USMLE®) to be eligible to boards and patients. Additionally, attestation provides COMLEX-USA apply to ACGME-accredited residency programs. The score reports to residency program directors and faculty. ACGME does not specify which licensing board exam(s) (i.e., COMLEX-USA, USMLE) applicants must take to be eligible COMPETENCY AND EVIDENCE-BASED DESIGN for appointment in ACGME-accredited residency programs. In 2019, COMLEX-USA completed a transition to a contemporary, two Frequently Asked Questions: Single Accreditation System decision-point, competency-based exam blueprint and evidence- Accreditation Council for Graduate Medical Education, 20191 based design informed by extensive research on osteopathic physician practice, expert consensus and stakeholder surveys.3 The enhanced COMLEX-USA blueprint4 assesses measurable outcomes PATHWAY TO LICENSURE of seven Fundamental Osteopathic Medical Competency Domains5 COMLEX-USA, the Comprehensive Osteopathic Medical Licensing and focuses on high-frequency, high-impact health issues and clinical Examination of the United States, is the exam series used by all presentations that affect patients. medical licensing authorities to make licensing decisions for osteopathic physicians. -
Community Benefit Report for Fiscal Year 2015 and 2016 Implementation Strategy
Community Benefit Report for Fiscal Year 2015 and 2016 Implementation Strategy 2 stanfordchildrens.org Contents Welcome: a Letter from Community Health Initiative: 3 our President and CEO � � � � � � � � � � � � � � � � � � � � � � � � 3 Improve the Social, Emotional and Mental Health of Children and Youth � � � � � � � � 18 Programs 19 In Depth: Reach & Rise 20 About Us � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 6 Other FY2015 Community Patient Care Highlights 2015 � � � � � � � � � � � � � � � � � � 7 Benefit Activities � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 21 In the Community: Programs that benefit the broader community 21 Community Benefit Report Overview � � � � � � � � � 8 Keeping Kids Safe: Programs that build safe communities 21 Community Benefit Defined 8 Advocacy and Outreach: A voice for children and families 22 Community Benefit Implementation Strategy 8 Workforce Development: Programs that train the next Community Health Needs Assessment 8 generation of health professionals 24 Community Benefit Oversight 8 Stanford Children’s Health Network Community Investment � � � � � � � � � � � � � � � � � � � � � � � 9 Overview � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � �26 Our Community 9 Joint Ventures 27 Our Investments 9 California Pacific Medical Center 27 John Muir Health 27 Community Health Initiatives � � � � � � � � � � � � � � � � 10 Our Bay Area Network � � � � � � � � � � � � � � � � � � � � � � �28 Our network locations by primary and secondary -

Psychiatry Residency + Phd Track
Psychiatry Residency + PhD Track Psychiatry Residency + PhD Track The Department of Psychiatry at Mount Sinai has been awarded NIMH support for this extraordinary and groundbreaking program—unique in the nation—offering a 2nd path to MD/PhD training for up to 2 residents per year. Designed for residents ready to commit to both psychiatry and research, the “PhD+” program longitudinally integrates clinical and research training over 7 years. It also offers the possibility of substantial financial advantages through NIH’s Loan Repayment Program (up to $35,000 per year for up to 6 years). As the fields of neuroscience and genetics have advanced in knowledge base and research strategies and techniques, PhD-level training may be a necessity for both effective translational research and obtaining research funding. Unfortunately, the number of psychiatrist MD/PhD researchers is small. Additionally, while the NIH has long supported Medical Scientist Training Programs, the established method of combined MD/PhD training is inefficient, in that the period of intense research and PhD completion is followed by many years of clinical training, meaning a long separation from research, a decline in research skills, a distance from the knowledge base and collaborators, and a need to retrain after residency. Our PhD+ track participates as Residency + PhD (1490400C3) in the offerings of the Icahn School of Medicine at Mount Sinai’s Psychiatry Residency Training Program, so that applicants may enter the program via the NRMP as PGY-1s. Current PGY-1s may also transfer into this track, from within our residency or from elsewhere. The PhD+ program consists of 5 components: 1) Completion of all clinical rotations/experiences required for Board Certification by the American Board of Psychiatry and Neurology; attendance at core didactics of the Residency Program. -
John Muir and UCSF Expand Network to Form Canopy Health
August 8, 2016 | VOLUME 23 | NUMBER 31 TOP STORIES John Muir and UCSF Expand Published Monday, California Healthfax is Network to Form Canopy Health copyrighted by HealthLeaders Media, a division of BLR, 35 Village Road, Suite 200, Middleton, Health plan to launch this fall with Health Net MA 01949 and is transmitted solely to the sub- scriber. Any unauthorized copying, duplication or The Bay Area Accountable Care Network established by John Muir Health transmission is strictly prohibited. Subscriptions and UCSF Health has added seven new hospitals to its network and changed its are $179 for 48 issues. For group and bulk sub- name to Canopy Health as it prepares to launch this fall. scriptions, call 800-650-6787. Canopy Health also added three new medical groups to its network to bolster a provider base that now includes more than 4,000 physicians. “We’ve CUSTOMER SERVICE CENTER made significant strides in a short amount of time as we work to provide Bay Email Subscribers: If you do not receive your copy of HealthFax, Area residents with an option to choose Canopy Health during open enrollment in send a request to: [email protected]. the fall of 2016,” said Canopy Health CEO Joel Criste. For renewals or other subscription questions, As part of its expansion, Canopy Health added Marin General Hospital, please call: 800-650-6787. By fax: 866-592-7573. Sonoma Valley Hospital, San Ramon Regional Medical Center, Washington By email: [email protected] Hospital Healthcare System, Alameda Hospital, Highland Hospital, and San Leandro Hospital. Medical groups joining the network are Hill Physicians EDITORIAL SUBMISSIONS Medical Group, which has more than 2,250 physicians in the Bay Area, the John To submit an item for consideration, con- Muir Physician Network, and Meritage Medical Network. -
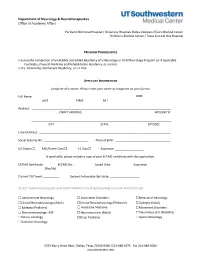
Neurology Fellowship Application
Department of Neurology & Neurotherapeutics Office of Academic Affairs Parkland Memorial Hospital / University Hospitals Dallas Veterans Affairs Medical Center Children's Medical Center / Texas Scottish Rite Hospital PROGRAM PREREQUISITES • Successful completion of an ACGME accredited Residency of a Neurology or Child Neurology Program (or if applicable Psychiatry, Physical Medicine and Rehabilitation Residency, or similar). • U.S. Citizenship, Permanent Residency, or J-1 Visa APPLICANT INFORMATION Complete all sections. Please enter your name as it appears on your license. Full Name: DOB: LAST FIRST M.I. Address: STREET ADDRESS APT/UNIT # ______________________________________________________________________________________ CITY STATE ZIP CODE Email Address: _________________________________________________________________________________ Social Security No.: ___________________________ Place of Birth: __________________________________ US Citizen ☐ EAD/Green Card ☐ J-1 Visa ☐ Expiration __________________ If applicable, please include a copy of your ECFMG certificate with this application. ECFMG Certificate: ________ ECFMG No.: ____________ Issued Date: _____________ Expiration ______________ (Yes/No) Current PGY level: __________ Desired Fellowship start date: __________________ SELECT WHICH NEUROLOGY & NEUROTHERAPEUTICS FELLOWSHIP(S) YOU ARE APPLYING FOR: ☐ Autoimmune Neurology ☐ Autonomic Disorders ☐Behavioral Neurology ☐Clinical Neurophysiology (Adult) ☐Clinical Neurophysiology (Pediatric) ☐ Epilepsy (Adult) ☐ Epilepsy (Pediatric) -

Boston Children's Hospital / Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health
Boston Children’s Hospital/Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health Speaker Alan Woolf, MD, MPH, FAACT, FAAP, FACMT Director, Pediatric Environmental Health Center, Boston Children’s Hospital Director, Region 1 New England PEHSU Director, Fellowship Training Program Professor, Harvard Medical School School Physician Acknowledgments & Disclosures This material was supported by the American Academy of Pediatrics (AAP) and funded (in part) by the cooperative agreement FAIN: 5 NU61TS000237-05 from the Agency for Toxic Substances and Disease Registry (ATSDR). Funding for this seminar was made possible (in part) by the cooperative agreement award number 1U61TS000237- 05 from the Agency for Toxic Substances and Disease Registry (ATSDR). The views expressed in written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services. •The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government •Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications. •In the past 12 months, we have had no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed -
Medical Scientist Training Program
The University of Michigan MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines A Handbook for Fellows https://www.medicine.umich.edu/medschool/education/md-phd- program/current students/ August 2018 CONTENTS 1. MSTP Office 2. Communication 3. Academic Advising 4. I.D. and Computer Access 5. Course of Study 6. Biological Chemistry Requirement 7. Medical School Registration 8. Medical and Graduate School Grading Systems 9. Graduate School Registration 10. Research Rotations 11. Selecting a Doctoral Field and the Thesis Research Mentor 12. Graduate School Residency Requirements 13. Research Responsibility and Ethics Requirements 14. Research Phase: External Funding Sources 15. Advancement to Candidacy 16. Precandidate Year to Candidacy Transition: Funding and Insurance Issues 17. Research Phase to M3 Transition 18. M4 Year 19. Transition to Post Graduate Training, Residency 20. Dean’s Letters 21. Simultaneous Awarding of Dual Degrees 22. United States Medical Licensure Examination Step 1 and Step 2 (Clinical Knowledge and Clinical Skills) 23. Rackham Graduate School Policies 24. Medical School Policies and Procedures 25. The Fellowship Award and the Stipend Level 26. Monthly Stipend Check 27. Taxability of NRSA Stipends 28. NIH Funding Trainee Appointment Forms and Trainee Termination Notice Forms 29. Tuition Payment, Billing Procedures, and Registration 30. Travel Funds and Expense Forms 31. Health Care Insurance 32. Health Service 33. CV and Publication File 34. Individual Development Pan (IDP) 35. Vacations and Other Absences 36. MSTP Scientific Retreat 37. MSTP Seminars 38. Citizenship 39. MSTP Committees: Operating Committee (OC) and Program Activities Committee (PAC) A Handbook for MSTP Fellows MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines for Fellows 1. -
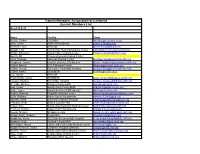
Trauma Managers Association of California Current Members List As of 10-8-15
Trauma Managers Association of California Current Members List As of 10-8-15 Name Facility Email Becker, Debra CCEMSA [email protected] Behr, Lynne Kaiser Permanente [email protected] Bennink, Lynn (Retired) [email protected] Blough, Lois Community Regional Medical Center [email protected] Bowlin, Maureen Inland Valley Medical Center [email protected] Bunch, Bill Colusa Regional Medical Center Case, Melinda Palomar Medical Center [email protected] Chapman, Joanne Coastal Valleys EMS Agency [email protected] Cohen, Marilyn UCLA Medical Center [email protected] Collins, Georgi Riverside Community Hospital [email protected] Collins, Kathy SSVEMSA [email protected] Cox, Susan (Retired) Crain-Riddle, Karen SSVEMSA [email protected] Crowley, Melanie Northridge Hospital [email protected] De Laby, Michael Orange County EMS [email protected] Diaz, Linda Santa Clara County EMS [email protected] Doyle, Lance Mountain-Valley EMS Agency [email protected] Dudley, Pamela Regional Medical Center [email protected] Duffy, Barbara Kaiser South Sacramento [email protected] Earnest, Karla Stanford Childrens Hospital [email protected] Erickson, Keith Solano County EMS [email protected] Fortier, Sue Sierra Vista Regional Medical Center [email protected] Frecceri, Christy Kaiser South Sacramento [email protected] Gawlik, Melanie Scripps La Jolla [email protected] Gough-Smith, -
2019‐2020 Internal Medicine Residency Handbook Table of Contents Contacts
2019‐2020 Internal Medicine Residency Handbook Table of Contents Contacts ............................................................................................................................................ 1 Introduction ...................................................................................................................................... 2 Compact ............................................................................................................................................ 2 Core Tenets of Residency ……………………………………………………………………………………………………………3 Program Requirements ……………………………………………………………………………………………………………….6 Resident Recruitment/Appointments .............................................................................................. 9 Background Check Policy ................................................................................................................ 10 New Innovations ............................................................................................................................. 11 Social Networking Guidelines ......................................................................................................... 11 Dress Code ...................................................................................................................................... 12 Resident’s Well Being ...................................................................................................................... 13 Academic Conference Attendance ................................................................................................ -

Primer for Applying to Internal Medicine Residency Programs A
Primer for Applying to Internal Medicine Residency Programs A) Fourth-Year Schedule: • Ideally, schedule the internal medicine sub-internship during July or August in order to procure a letter of recommendation (if needed). • Alternative clinical experiences to consider in place of the sub-internship include: o Away rotations: ▪ Away rotations are NOT required for IM. The majority of students applying to IM across the country do not partake in visiting rotations. Visiting rotations are most helpful if students demonstrate a significant interest in a particular program or location. ▪ Away rotations may increase the chance of an invitation to interview at the hosting institution, but this is NOT guaranteed. ▪ Visiting subspecialty electives are preferred over visiting sub- internships, which require strong institutional systems knowledge to optimize clinical performance. o Critical Care Clerkship o Subspecialty Rotations at Cooper • IM residency interviews often start in mid-October and extend to the end of January with the majority of interviews occurring in November and December. Therefore, plan accordingly. • Schedule a more rigorous clinical experience in the spring to enhance clinical skills prior to graduation in preparation for residency. B) Timeline: C) Curriculum Vitae & ERAS Application: • Timeline: Should include all longitudinal, meaningful experiences from the first day of college until present day. • Experience Boxes: o Research Experience: ▪ Include all meaningful research at both the undergraduate and medical school level -
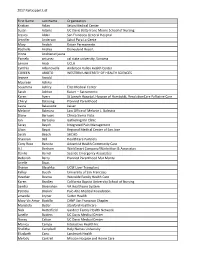
2017 Participant List First Name Last Name Organization Kristian Aclan
2017 Participant List First Name Last Name Organization Kristian Aclan Seton Medical Center Susan Adams UC Davis Betty Irene Moore School of Nursing Jessica Aldaz San Francisco General Hospital Jennifer Anderson Salud Para La Gente Mary Andich Kaiser Permanente Rochelle Andres Disneyland Resort Irinna Andrianarijaona Pamela antunez cal state university, Sonoma Lenore Arab UCLA Cynthia Arbanovella Anderson Valley Health Center COREEN ARIOTO WESTERN UNIVERSITY OF HEALTH SCIENCES Jeanne Arnold Maureen Ashiku Sosamma Ashley Elite Medical Center Sarah Ashton Kaiser -- Sacramento Karen Ayers St Joseph Hospital, Hospice of Humboldt, ResolutionCare Palliative Care Cheryl Balaoing Planned Parenthood Laura Balassone kaiser Melanie Balestra Law Office of Melanie L. Balestra Diane Barrows Clinica Sierra Vista Jan Bartuska Gathering Inn Clinic Seray Bayoh Integrated Pain Management Lilian Bayot Regional Medical Center of San Jose Sarah Beach SHCHD Shannon Bell HealthCare Partners Cony Rose Bencito Adventist Health Community Care A.J. Benham WorkSmart Company/Warbritton & Associates Danilo Bernal Seaside Emergency Associates Deborah Berry Planned Parenthood Mar Monte Arielle Bivas Sharon Blaschka UCSF Liver Transplant Kelley Booth University of San Francisco Heather Bosma Westside Family Health Care Karen Bradley California Baptist University School of Nursing Sandra Bresnahan VA Healthcare System Patricia Briskin` Palo Alto Medical Foundation amanda bryner Sutter Health Mary Vic Amor Bustillo CANP San Francisco Chapter Maristela Butler Stanford Healthcare -
SAP Crystal Reports
Results of the 2016 NRMP Program Director Survey Specialties Matching Service October 2016 www.nrmp.org Requests for permission to use these data as well as questions about the content of this publication or the National Resident Matching Program data and reports may be directed to Mei Liang, Director of Research, NRMP, at [email protected]. Questions about the NRMP should be directed to Mona M. Signer, President and CEO, NRMP, at [email protected]. Suggested Citation National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey, Specialties Matching Service. National Resident Matching Program, Washington, DC. 2016. Copyright © 2016 National Resident Matching Program. All rights reserved. Permission to use, copy and/or distribute any documentation and/or related images from this publication shall be expressly obtained from the NRMP. Table of Contents Introduction .................................................................................................................................................... 1 Response rates ................................................................................................................................................. 2 All Specialties................................................................................................................................................. 3 Charts for Individual Specialties Abdominal Transplant Surgery ....................................................................................................................