Platelet Serology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines for Transfusions
Guidelines for Transfu- sion Prepared by: Community Transfusion Committee Lincoln, Nebraska CHAIR: Aina Silenieks, MD MEMBERS: L. Bausch, M.D. R. Burton, M.D. S. Dunder, M.D. D. Voigt, M.D. B. J. Wilson, M.D. COMMUNITY Becky Croner REPRESENTATIVES: Ellen DiSalvo Christa Engel Phyllis Ericson Kelly Gillaspie Pat Gilles Vic Grdina Jessica Henrichs Kelly Jensen Laurel McReynolds Christina Nickel Angela Novotny Kelley Thiemann Janet Wachter Jodi Wikoff Guidelines For Transfusion Community Transfusion Committee INTRODUCTION The Community Transfusion Committee is a multidisciplinary group that meets to monitor blood utilization practices, establish guidelines for transfusion and discuss relevant transfusion related topics. It is comprised of physicians from local hospitals, invited guests, and community representatives from the hospitals’ transfusion services, nursing services, perfusion services, health information management, and the Nebraska Community Blood Bank. These Guidelines for Transfusion are reviewed and revised biannually by the Community Trans- fusion Committee to ensure that the industry’s most current practices are promoted. The Guidelines are the standard by which utilization practices are evaluated. They are also de- signed to provide helpful information to assist physicians to provide appropriate blood compo- nent therapy to patients. Appendices have been added for informational purposes and are not to be used as guidance for clinical decision making. ADULT RED CELLS A. Indications 1. One of the following a. Hypovolemia and hypoxia (signs/symptoms: syncope, dyspnea, postural hypoten- sion, tachycardia, angina, or TIA) secondary to surgery, trauma, GI tract bleeding, or intravascular hemolysis, OR b. Evidence of acute loss of 15% of total blood volume or >750 mL blood loss, OR c. -

Introduction to Flow Cytometry Principles Data Analysis Protocols Troubleshooting
Flow Cytometry ipl.qxd 11/12/06 11:14 Page i Introduction to Flow Cytometry Principles Data analysis Protocols Troubleshooting By Misha Rahman, Ph.D. Technical advisors Andy Lane, Ph.D. Angie Swindell, M.Sc. Sarah Bartram, B.Sc. Your first choice for antibodies! Flow Cytometry ipl.qxd 11/12/06 11:14 Page ii Flow Cytometry ipl.qxd 11/12/06 11:14 Page iii Introduction to Flow Cytometry Principles Data analysis Protocols Troubleshooting By Misha Rahman, Ph.D. Technical advisors Andy Lane, Ph.D. Angie Swindell, M.Sc. Sarah Bartram, B.Sc. Flow Cytometry ipl.qxd 11/12/06 11:14 Page 2 Preface How can I explain what flow cytometry is to someone that knows nothing about it? Well, imagine it to be a lot like visiting a supermarket. You choose the goods you want and take them to the cashier. Usually you have to pile them onto a conveyor. The clerk picks up one item at a time and interrogates it with a laser to read the barcode. Once identified and if sense prevails, similar goods are collected together e.g. fruit and vegetables go into one shopping bag and household goods into another. Now picture in your mind the whole process automated; replace shopping with biological cells; and substitute the barcode with cellular markers – welcome to the world of flow cytometry and cell sorting! We aim to give you a basic overview of all the important facets of flow cytometry without delving too deeply into the complex mathematics and physics behind it all. For that there are other books (some recommended at the back). -

A Multicenter Analysis of Subjectivity of Indirect Immunofluorescence Test in Antinuclear Antibody Screening
Arch Rheumatol 2019;34(3):326-333 doi: 10.5606/ArchRheumatol.2019.7310 ORIGINAL ARTICLE A Multicenter Analysis of Subjectivity of Indirect Immunofluorescence Test in Antinuclear Antibody Screening Vildan TURAN FARAŞAT1, Talat ECEMİŞ1, Yavuz DOĞAN2, Aslı Gamze ŞENER3, Gülfem TEREK ECE4, Pınar ERBAY DÜNDAR5, Tamer ŞANLIDAĞ6 1Department of Medical Microbiology, Manisa Celal Bayar University, Faculty of Medicine, Manisa, Turkey 2Department of Medical Microbiology, Dokuz Eylül University, Faculty of Medicine, Izmir, Turkey 3Department of Medical Microbiology, Katip Çelebi University, Faculty of Medicine, Izmir, Turkey 4Department of Medical Microbiology, Izmir Medicalpark Hospital, Izmir, Turkey 5Department of Public Health, Manisa Celal Bayar University, Faculty of Medicine, Manisa, Turkey 6Department of Medical Microbiology, Manisa Celal Bayar University, Faculty of Medicine, Manisa, Turkey ABSTRACT Objectives: This study aims to evaluate the interpretation of the antinuclear antibody (ANA)-indirect immunofluorescence (IIF) test results based on the interpreter-related subjectivity and to examine the inter-center agreement rates with the performance of each laboratory. Patients and methods: The ANA-IIF testing was carried out in a total of 600 sera and evaluated by four laboratories. The inter-center agreement rates were detected. The same results given by the four centers were accepted as gold standard and the predictive values of each center were calculated. Results: The inter-center agreement was reported for ANA-IIF test results from 392 of 600 (65.3%) sera, while 154 of 392 results were positive. Four study centers reported 213 (35.5%), 222 (37.0%), 266 (44.3%), and 361 (60.2%) positive test results, respectively. In terms of the patterns, the highest and lowest positive predictive values were 72.3% and 42.7%, respectively, while the highest and lowest negative predictive values were 99.6% and 61.5%, respectively. -
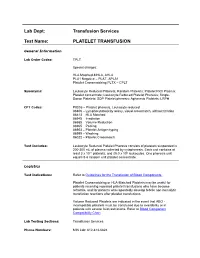
Platelet Transfusion
Lab Dept: Transfusion Services Test Name: PLATELET TRANSFUSION General Information Lab Order Codes: TPLT Special charges: HLA Matched-MHLA, AHLA PLA1 Negative – PLAT, APLA1 Platelet Crossmatching PLTX – CPLT Synonyms: Leukocyte Reduced Platelets; Random Platelets; Platelet Rich Plasma; Platelet concentrate; Leukocyte Reduced Platelet Pheresis; Single- Donor Platelets; SDP Platelet pheresis; Apheresis Platelets; LRPH CPT Codes: P9035 – Platelet pheresis, Leukocyte reduced 86806 – Lymphocytotoxicity assay, visual crossmatch, without titration 86813 – HLA Matched 86945 – Irradiation 86985 – Volume Reduction 86965 – Pooling 86903 – Platelet Antigen typing 86999 – Washing 86022 – Platelet Crossmatch Test Includes: Leukocyte Reduced Platelet Pheresis consists of platelets suspended in 200-300 mL of plasma collected by cytapheresis. Each unit contains at least 3 x 1011 platelets, and ≤5.0 x 106 leukocytes. One pheresis unit equals 5-6 random unit platelet concentrate. Logistics Test Indications: Refer to Guidelines for the Transfusion of Blood Components. Platelet Crossmatching or HLA-Matched Platelets may be useful for patients receiving repeated platelet transfusions who have become refractile, and for patients who repeatedly develop febrile non-hemolytic transfusion reactions after platelet transfusions. Volume Reduced Platelets are indicated in the event that ABO - incompatible platelets must be transfused due to availability or in patients with severe fluid restrictions. Refer to Blood Component Compatibility Chart Lab Testing Sections: Transfusion Services Phone Numbers: MIN Lab: 612-813-6824 STP Lab: 651-220-6558 Test Availability: Daily, 24 hours Turnaround Time: 1 - 2 hours Standard Dose/Volume: <10 kg: 10 – 15 mL/kg up to one unit or 50 mL maximum 10 – 15 kg: 1/3 pheresis unit 15 – 25 kg: 1/2 pheresis unit >25 kg: 1 pheresis unit Rate of Infusion: 10 minutes/unit, <4 hours Administration: Must be administered through a blood component administration filter. -

Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS
Journal of Blood Group Serology and Molecular Genetics VOLUME 34, N UMBER 1, 2018 This issue of Immunohematology is supported by a contribution from Grifols Diagnostics Solutions, Inc. Dedicated to advancement and education in molecular and serologic immunohematology Immunohematology Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS S EROLOGIC M ETHOD R EVIEW 1 Warm autoadsorption using ZZAP F.M. Tsimba-Chitsva, A. Caballero, and B. Svatora R EVIEW 4 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A brief overview of clinical significance of blood group antibodies M.J. Gandhi, D.M. Strong, B.I. Whitaker, and E. Petrisli C A S E R EPORT 7 Management of pregnancy sensitized with anti-Inb with monocyte monolayer assay and maternal blood donation R. Shree, K.K. Ma, L.S. Er and M. Delaney R EVIEW 11 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A review of in vitro methods to predict the clinical significance of red blood cell alloantibodies S.J. Nance S EROLOGIC M ETHOD R EVIEW 16 Recovery of autologous sickle cells by hypotonic wash E. Wilson, K. Kezeor, and M. Crosby TO THE E DITOR 19 The devil is in the details: retention of recipient group A type 5 years after a successful allogeneic bone marrow transplant from a group O donor L.L.W. -

Blood Product Modifications: Leukofiltration, Irradiation and Washing
Blood Product Modifications: Leukofiltration, Irradiation and Washing 1. Leukocyte Reduction Definitions and Standards: o Process also known as leukoreduction, or leukofiltration o Applicable AABB Standards, 25th ed. Leukocyte-reduced RBCs At least 85% of original RBCs < 5 x 106 WBCs in 95% of units tested . Leukocyte-reduced Platelet Concentrates: At least 5.5 x 1010 platelets in 75% of units tested < 8.3 x 105 WBCs in 95% of units tested pH≥6.2 in at least 90% of units tested . Leukocyte-reduced Apheresis Platelets: At least 3.0 x 1011 platelets in 90% of units tested < 5.0 x 106 WBCs 95% of units tested pH≥6.2 in at least 90% of units tested Methods o Filter: “Fourth-generation” filters remove 99.99% WBCs o Apheresis methods: most apheresis machines have built-in leukoreduction mechanisms o Less efficient methods of reducing WBC content . Washing, deglycerolizing after thawing a frozen unit, centrifugation . These methods do not meet requirement of < 5.0 x 106 WBCs per unit of RBCs/apheresis platelets. Types of leukofiltration/leukoreduction o “Pre-storage” . Done within 24 hours of collection . May use inline filters at time of collection (apheresis) or post collection o “Pre-transfusion” leukoreduction/bedside leukoreduction . Done prior to transfusion . “Bedside” leukoreduction uses gravity-based filters at time of transfusion. Least desirable given variability in practice and absence of proficiency . Alternatively performed by transfusion service prior to issuing Benefits of leukoreduction o Prevention of alloimmunization to donor HLA antigens . Anti-HLA can mediate graft rejection and immune mediated destruction of platelets o Leukoreduced products are indicated for transplant recipients or patients who are likely platelet transfusion dependent o Prevention of febrile non-hemolytic transfusion reactions (FNHTR) . -

Comparison of Histopathology, Immunofluorescence, and Serology
Global Dermatology Cae Report ISSN: 2056-7863 Comparison of histopathology, immunofluorescence, and serology for the diagnosis of autoimmune bullous disorders: an update Seline Ali E1, Seline Lauren N1, Sokumbi Olayemi1* and Motaparthi Kiran2,3 1Department of Dermatology, Medical College of Wisconsin, Milwaukee, WI, USA 2Dermatopathology, Miraca Life Sciences, USA 3Department of Dermatology, University of Texas Southwestern Medical Center, Dallas, TX, USA Introduction In an ELISA, the target antigen of interest (such as the NC16a domain of BP180) is immobilized by physical adsorption or by The diagnosis of autoimmune bullous disorders (AIBDs) relies on antibody capture. When antibody capture is utilized, this is referred to several different diagnostic methods. These include histopathology, as “sandwich ELISA” because the target antigen is bound between the direct immunofluorescence (DIF), indirect immunofluorescence immobilizing antibody and the primary antibody. Primary antibodies (IIF), enzyme-linked immunosorbent assay (ELISA) and are present in the patient’s serum. Enzyme-linked secondary antibodies immunoblotting. When faced with a presumptive AIBD, the are then added which bind the Fc region of primary antibodies. most widely employed method for diagnosis by dermatologists is Substrate is added and converted by the enzyme into a signal. A a combination of histopathology and DIF. While DIF is still the resulting color change, fluorescence, or electrochemical signal is diagnostic method of choice for linear IgA bullous disease and IgA quantitatively measured and reported [5]. pemphigus, ELISA is a more accurate, cost-effective and less invasive method of diagnosis for several AIBDs including pemphigus vulgaris Western blot is synonymous with immunoblot. For this method, and foliaceus, based on currently available evidence [1-3]. -

Online-Only Appendix: List of Inclusion and Exclusion Criteria
ONLINE-ONLY APPENDIX: LIST OF INCLUSION AND EXCLUSION CRITERIA INCLUSION CRITERIA [1] Male subjects between the ages of 35 and 70 years, inclusive, with Type 2 diabetes mellitus as defined by the American Diabetes Association (Diabetes care, Vol. 21: S5- S19, 1998) for more than one year. [2] Subjects must have Body Mass Index (BMI) < 36 kg/m². [3] Stable glycemic control (Hb A1C <11%). [4] Subjects must be off all oral hypoglycemic agents 24 hours prior to each study dosing day and off any investigational drug for at least four weeks. [5] Subjects must refrain from strenuous physical activity beginning 72 hours prior to admission and through the duration of the study. [6] Subjects must be willing and able to be confined to the Clinical Research Unit as required by the protocol. [7] Subjects must be willing and able to provide written informed consent. EXCLUSION CRITERIA [1] History or presence of clinically significant cardiovascular, respiratory, hepatic, renal, gastrointestinal, neurological or infectious disorders capable of altering the absorption, metabolism or elimination of drugs, or of constituting a risk factor when taking the study medication. [2] Subjects with gastroparesis, orthostatic hypotension and hypoglycemia unawareness (autonomic neuropathy). [3] Subjects with “brittle” diabetes or predisposition to severe hypoglycemia, e.g., 2 or more serious hypoglycemic episodes (requiring another’s assistance) within the past year, or any hospitalization or emergency room visit due to poor diabetic control within the past 6 months. [4] Evidence of significant active hematological disease and/or cumulative blood donation of 1 unit (500 mL) or more including blood drawn during clinical trials in the last 3 months. -

Application of Quantitative Immunofluorescence to Clinical Serology: Antibody Levels of Treponema Pallidum GRACE L
JOURNAL OF CLINICAL MICROBIOLOGY, May 1992, p. 1294-1296 Vol. 30, No. 5 0095-1137/92/051294-03$02.00/0 Copyright C 1992, American Society for Microbiology Application of Quantitative Immunofluorescence to Clinical Serology: Antibody Levels of Treponema pallidum GRACE L. PICCIOLO* AND DAVID S. KAPLAN Center for Devices and Radiological Health, Food and Drug Administration, 12200 Wilkins Avenue, Rockville, Maryland 20852 Received 27 March 1991/Accepted 20 January 1992 A previously reported method of quantitative immunofluorescence, employing a calibrated photometric system and chemically stabilized fluorescence intensity, was used to replace the subjective, visual method of endpoint determination with a quantitative, calibrated measurement of antibodies to Treponema paUlidum in serum. The results of the quantitative immunofluorescence method showed a 90% correlation with the subjective determinations of the visual method. A quantitative immunofluorescence (QIF) method to de- measured by using an acridine orange filter set, with a 400- to termine immunofluorescence with a quantitative, calibrated 440-nm excitation and LP 470 emission filters. photometric intensity of the fluorescent reaction product has Reducing agent. Dithioerythritol (DTE) (Sigma Chemical been reported previously by us (4). This method used uranyl Co., St. Louis, Mo.) was prepared as stock solution contain- glass slides in the calibration and standardization of the ing 0.3 M reducing agent in 0.5 M Tris buffer, pH 8.2 (Sigma microscope-photometer voltage measurements. To stabilize Chemical Co.). DTE was diluted 1:9 with standard buffered the fluorescence emission, dithioerythritol (DTE) was incor- glycerol mounting medium (Clinical Sciences, Inc., Whip- porated into the buffered glycerol mounting medium of the pany, N.J.) (4, 8). -

Transfusion Triggers for Platelets and Other Blood Products Sunil Karanth Indian Journal of Critical Care Medicine (2019): 10.5005/Jp-Journals-10071-23250
INVITED ARTICLE Transfusion Triggers for Platelets and Other Blood Products Sunil Karanth Indian Journal of Critical Care Medicine (2019): 10.5005/jp-journals-10071-23250 INTRODUCTION Department of Intensive Care Unit, Manipal Hospital, Bengaluru, Transfusion of whole blood is not associated with any significant Karnataka, India benefit, rather can be harmful. Significant advances have been Corresponding Author: Sunil Karanth, Department of Intensive made in transfusion medicine, facilitating the use of blood product Care Unit, Manipal Hospital, Bengaluru, Karnataka, India, e-mail: or component therapy than use of whole blood (Fig. 1). In 2009, a [email protected] report on Serious Hazards of Transfusion in the UK, estimated that How to cite this article: Karanth S. Transfusion Triggers for Platelets a total of 3 million units of blood components were released. The and Other Blood Products. Indian J Crit Care Med 2019;23(Suppl requirement of the same in South-East Asia is much higher to the 3):S189–S190. tune of 15 million units annually. The current recommendation Source of support: Nil is to use blood only in life-threatening situations, rather than to Conflict of interest: None normalize abnormal numbers. PLATELETS Platelets are derived from the buffy coat of whole blood donations. A pooled platelet concentrate includes pooled buffy-coat derived platelets from four whole-blood donations suspended in platelet additive solution and plasma of one of the four donors. It contains 240000 platelets pooled from 4–6 donors. A Single donor platelet is derived from a single-donor by a process of apheresis. In view of the lesser number of donors and the theoretical advantage of involving a single-donor platelet (SDP) may be preferred over the use of platelets from multiple donors. -

Blood-Platelet-Orders-Outpatient-V3
Blood / Platelet Orders Outpt v3 USE THIS ORDER SET FOR OUTPATIENT NON URGENT BLOOD OR PLATELET TRANSFUSION 24 Hours advanced notice required for infusion center NO MORE THAN 2 UNITS OF RED BLOOD CELLS CAN BE INFUSED IN THE INFUSION CENTER PER DAY BMH Outpatient Infusion Center: Fax completed order set to 843-522-7313/Phone 843-522-7680 Hospital Outpatient: Fax Completed order set to Registration at 843-522-5741 and notify Nursing Supervisor at 843-522-7653 Service Designation THIS IS NOT AN ADMISSION SET Patient Name ___________________________________ Patient DOB ____________ Service Designation Blood Platelet Outpatient Attending ___________________________________ Date Requested ___________________________________ Status Outpatient Check Appropriate Diagnosis Below: [ Anemia of chronic renal disease Anemia related to chemotherapy Aplastic anemia Anemia related to cancer Anemia related to blood loss Sickle cell disease Anemia unspecified Thombocytopenia (platelets) Other _________________________ ] Allergies Update Allergies in the Summary Panel in MEDITECH Special Requirement: (REQUIRES SPECIAL ORDER ONE DAY IN ADVANCE) Special Requirement RBC or Platelets REQUIRES SPECIAL ORDER ONE DAY IN ADVANCE [ Irradiated CMV Negative HgBS Negative ] Medications diphenhydrAMINE HCl (Benadryl) 25 mg orally single dose premedicate prior to transfusion diphenhydrAMINE HCl (Benadryl) 50 mg orally single dose premedicate prior to transfusion diphenhydrAMINE HCl (Benadryl) 25 mg intravenously single dose premedicate prior to transfusion diphenhydrAMINE -

Platelet Transfusion Refractoriness
Evaluation of the Patient with Suspected Platelet Refractory State NOTE: While evaluating the patient for suspected immune refractory state, provide ABO matched platelets if available. 1. Determine if the Alloimmunization may be directed against platelet specific antigens or, more commonly HLA patient is at risk for antigens. Current leukoreduction methods are generally effective at preventing HLA alloimmunization: alloimmunization. Alloimmunization may occur in multiply transfused patients. A. Multiparous female? B. Multiple nonleukoreduced transfusions? C. Organ transplant? Assess previous platelet transfusions: TWO previous ABO compatible/ABO matched transfusions fail to yield an increase in platelet count >10K or a CCI >5-7500 Platelet counts should be performed 10 – 60 minutes post transfusion and 24 hour post transfusion. One hour post transfusion platelet counts that fail to demonstrate a >10K increase in platelets is suggestive of immune destruction. Adequate one hour post transfusion platelet counts and decreased 24 hour post transfusion platelet counts are suggestive of consumption/utilization/sequestration. Condition Presentation Laboratory Findings 2. Exclude non- alloimmune causes Leukocytosis, +cultures Sepsis Fever, tachycardia, tachypnea, etc. of a platelet refractory state: Thrombocytopenia, elevated PT, APTT, decreased DIC Bleeding, oozing These are generally fibrinogen, + fibrin degradation disorders of platelet products consumption. Sequestration Splenomegaly . Antibiotics (esp Vancomycin) Drugs are an often . Heparin (Heparin induced Thrombocytopenia, diminished overlooked cause of Drugs thrombocytopenia)* response to transfusion platelet destruction. Amphotericin . Purpura, esp of lower extremities Thrombocytopenia Auto-Immune . Easy bruising Auto antibodies to platelet thrombocytopenia* Nose bleeds glycoprotein IIb/IIIa (aka ITP) . Bleeding gums Significant bleeding may consume Thrombocytopenia, diminished Bleeding platelets response to transfusion Continued on next page TS 017 (Rev.