Results of a Multice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

STADION SC FREIBURG Plausibilitätsprüfung Baukostenschätzung Stadion Freiburg
Plausibilitätsprüfung - IFS Kostenschätzung - 03.09.2014 STADION SC FREIBURG Plausibilitätsprüfung Baukostenschätzung Stadion Freiburg Vorgehensweise zur Plausibilisierung der IFS Kostenschätzung PROPROJEKT wurde im Juli 2014 von der Stadt Freiburg im Breisgau mit der Plausibilisierung der von IFS erstellten Baukostenschätzung für den Neubau eines Stadions für den SC Freiburg beauftragt. Hierfür werden zwei unterschiedliche und voneinander unabhängige Ansätze gewählt: 1. Benchmarks (Top-Down Plausibilisierung): › Erhebung der Baukosten von Stadionneubauten (bzw. Umbauten) der 1.-3. Liga. › Untersuchung von 26 Stadien, welche ab dem Jahre 2000 in Deutschland neu bzw. grundlegend umgebaut wurden. › Ermittlung eines – auf dieser Datengrundlage basierenden – stadionspezifischen Kennwerts „Baukosten pro Sitzplatz“ als vergleichende Benchmark. 2. Baukostenschätzung (Bottom-Up Plausibilisierung): › Überprüfung der Einzelpositionen der IFS Baukostenschätzung auf Plausibilität. › Erstellung einer eigenen Baukostenschätzung für ein Stadion in vergleichbarer Kapazität und Qualität wie das Stadion Freiburg auf Basis eigener und in der Praxis bewährter Kostenkennwerte für Stadionneubauten. › Gegenüberstellung mit den Gesamtkosten der IFS Kostenschätzung. Plausibilitätsprüfung › Stadion SC Freiburg 3. September 2014 › 2 Inhalt PLAUSIBILITÄTSPRÜFUNG 1 - Benchmarks - Vergleichswerte Stadionneubauten 2 - Baukostenschätzung - Eigenansatz PROPROJEKT 3 - Fazit 1 - Benchmarks Vergleichswerte von 26 Stadionneubauten Vorgehensweise zur Ermittlung der Benchmarks -

DIRECT-LIVE...Bundesliga Augsburg Vs Bayer Leverkusen En
bundesliga augsburg vs bayer leverkusen : liveStream, time GO LIVE http://nufilm.live/event/bundesliga-augsburg-vs-bayer-leverkusen CLICK HERE GO LIVE http://nufilm.live/event/bundesliga-augsburg-vs-bayer-leverkusen Bayer Leverkusen have never lost to Augsburg in 19 Bundesliga encounters. No match-up in the league has been played so many times without both teams recording at least one win. The latest updates for FC Augsburg - Bayer 04 Leverkusen on Matchday 3 in the 2021/2022 Bundesliga season - plus a complete list of all fixtures. FC Augsburg is going head to head with Bayer 04 Leverkusen starting on 28 Aug 2021 at 13:30 UTC at WWK ARENA stadium, Augsburg city, Germany. The match is a part of the Bundesliga. FC Augsburg played against Bayer 04 Leverkusen in 2 matches this season. Currently, FC Augsburg rank 8th, while Bayer 04 Leverkusen hold 3rd position. Bundesliga Augsburg vs Bayer Leverkusen match preview on 28.08.2021: team stats, match H2H, last results, lineups, injuries, standings, pre- match odds, over/under trend, BTTS trend Augsburg vs Bayer Leverkusen Odds - Saturday August 28 2021. Live betting odds and lines, betting trends, against the spread and over/under trends, injury reports and matchup stats for bettors. Odds/Point Spread: FC Augsburg (+290) Bayer Leverkusen (-118) Moussa Diaby and Bayer Leverkusen (1-1-0, 3rd in Bundesliga) travel to WWK Arena on Saturday where they'll take on FC Augsburg (0-1-1 Augsburg vs Leverkusen: FC Augsburg will be up against Bayer Leverkusen in the Matchday 3 of the Bundesliga 2021/22 season. -
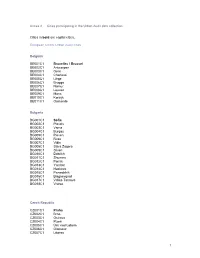
Annex 2 — Cities Participating in the Urban Audit Data Collection
Annex 2 — Cities participating in the Urban Audit data collection Cities in bold are capital cities. European Union: Urban Audit cities Belgium BE001C1 Bruxelles / Brussel BE002C1 Antwerpen BE003C1 Gent BE004C1 Charleroi BE005C1 Liège BE006C1 Brugge BE007C1 Namur BE008C1 Leuven BE009C1 Mons BE010C1 Kortrijk BE011C1 Oostende Bulgaria BG001C1 Sofia BG002C1 Plovdiv BG003C1 Varna BG004C1 Burgas BG005C1 Pleven BG006C1 Ruse BG007C1 Vidin BG008C1 Stara Zagora BG009C1 Sliven BG010C1 Dobrich BG011C1 Shumen BG012C1 Pernik BG013C1 Yambol BG014C1 Haskovo BG015C1 Pazardzhik BG016C1 Blagoevgrad BG017C1 Veliko Tarnovo BG018C1 Vratsa Czech Republic CZ001C1 Praha CZ002C1 Brno CZ003C1 Ostrava CZ004C1 Plzeň CZ005C1 Ústí nad Labem CZ006C1 Olomouc CZ007C1 Liberec 1 CZ008C1 České Budějovice CZ009C1 Hradec Králové CZ010C1 Pardubice CZ011C1 Zlín CZ012C1 Kladno CZ013C1 Karlovy Vary CZ014C1 Jihlava CZ015C1 Havířov CZ016C1 Most CZ017C1 Karviná CZ018C2 Chomutov-Jirkov Denmark DK001C1 København DK001K2 København DK002C1 Århus DK003C1 Odense DK004C2 Aalborg Germany DE001C1 Berlin DE002C1 Hamburg DE003C1 München DE004C1 Köln DE005C1 Frankfurt am Main DE006C1 Essen DE007C1 Stuttgart DE008C1 Leipzig DE009C1 Dresden DE010C1 Dortmund DE011C1 Düsseldorf DE012C1 Bremen DE013C1 Hannover DE014C1 Nürnberg DE015C1 Bochum DE017C1 Bielefeld DE018C1 Halle an der Saale DE019C1 Magdeburg DE020C1 Wiesbaden DE021C1 Göttingen DE022C1 Mülheim a.d.Ruhr DE023C1 Moers DE025C1 Darmstadt DE026C1 Trier DE027C1 Freiburg im Breisgau DE028C1 Regensburg DE029C1 Frankfurt (Oder) DE030C1 Weimar -

Industrial Market Profile
Industrial Market Profile Cologne | 4th quarter 2019 January 2020 Industrial Market Profile | 4th quarter 2019 Cologne Warehousing Take-up Weakest take-up for the past ten years Around 89,000 sqm of space larger than 5,000 sqm was taken up in the market for warehousing and logistics space (owner-occupiers and lettings) in the Cologne region* in 2019; this was over 50% below the previous year’s result and below the five-year average. In contrast to previous years, no deals were concluded for units larger than 20,000 sqm and the average size of deals concluded in 2019 was around 9,900 sqm. The largest letting of the year was registered by Logwin AG, in which the logistics com- with a total area of around 17,000 sqm. Companies in the pany signed a contract for around 18,000 sqm in a project distribution/logistics segment accounted for around 50% in Kerpen. The second-largest contract was also conclu- of total take-up, while manufacturers accounted for 26%. ded by a logistics company for an existing unit in Bedburg, In the Cologne urban area, the supply of space available at short notice remains scarce, and no easing of this situation is foreseeable in the coming months. The situation is some- Prime Rent ≥ 5,000 sqm what different in some of the surrounding communities: for example, in Kerpen and Euskirchen, thanks to speculative new construction, there are available units larger than 5,000 sqm. The prime rent for warehousing space larger than 5,000 sqm achieved in the Cologne urban area has remained stable over the past twelve months at €5.10/sqm/month. -

Kahlil Gibran a Tear and a Smile (1950)
“perplexity is the beginning of knowledge…” Kahlil Gibran A Tear and A Smile (1950) STYLIN’! SAMBA JOY VERSUS STRUCTURAL PRECISION THE SOCCER CASE STUDIES OF BRAZIL AND GERMANY Dissertation Presented in Partial Fulfillment of the Requirements for The Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Susan P. Milby, M.A. * * * * * The Ohio State University 2006 Dissertation Committee: Approved by Professor Melvin Adelman, Adviser Professor William J. Morgan Professor Sarah Fields _______________________________ Adviser College of Education Graduate Program Copyright by Susan P. Milby 2006 ABSTRACT Soccer playing style has not been addressed in detail in the academic literature, as playing style has often been dismissed as the aesthetic element of the game. Brief mention of playing style is considered when discussing national identity and gender. Through a literature research methodology and detailed study of game situations, this dissertation addresses a definitive definition of playing style and details the cultural elements that influence it. A case study analysis of German and Brazilian soccer exemplifies how cultural elements shape, influence, and intersect with playing style. Eight signature elements of playing style are determined: tactics, technique, body image, concept of soccer, values, tradition, ecological and a miscellaneous category. Each of these elements is then extrapolated for Germany and Brazil, setting up a comparative binary. Literature analysis further reinforces this contrasting comparison. Both history of the country and the sport history of the country are necessary determinants when considering style, as style must be historically situated when being discussed in order to avoid stereotypification. Historic time lines of significant German and Brazilian style changes are determined and interpretated. -

Subsidiary and Affiliated Companies of the Bayer Group As of December 31, 2015, Pursuant to Section 313 of the German Commercial Code
Subsidiary and aff iliated companies of the Bayer Group as of December 31, 2015, pursuant to Section 313 of the German Commercial Code Bayer Annual Report 2015 1 Consolidated Financial Statements Subsidiary and affiliated companies of the Bayer Group as of December 31, 2015, pursuant to Section 313 of the German Commercial Code Subsidiary and affiliated companies of the Bayer Group as of December 31, 2015, pursuant to Section 313 of the German Commercial Code The fully consolidated companies are listed in the following table: Fully Consolidated Subsidiaries [Table 4.18-1] Company Name Place of Business Bayer´s interest % Europe Adverio Pharma GmbH Schönefeld, Germany 100 AgrEvo Verwaltungsgesellschaft mbH Frankfurt am Main, Germany 100 Alcafleu Management GmbH & Co. KG Schönefeld, Germany 99.9 Algeta Innovations AS Oslo, Norway 100 AO Bayer Moscow, Russia 100 Bayer (Schweiz) AG Zurich, Switzerland 100 Bayer 04 Immobilien GmbH Leverkusen, Germany 100 Bayer 04 Leverkusen Fußball GmbH Leverkusen, Germany 100 Bayer A/S Copenhagen, Denmark 100 Bayer AB Solna, Sweden 100 Bayer Agriculture Limited Cambridge, U.K. 100 Bayer Altersversorgung GmbH Leverkusen, Germany 100 Bayer Animal Health GmbH Leverkusen, Germany 100 Bayer Antwerpen NV Diegem, Belgium 100 Bayer AS Oslo, Norway 100 Bayer Austria Gesellschaft m.b.H. Vienna, Austria 100 Bayer B.V. Mijdrecht, Netherlands 100 Bayer Beteiligungsverwaltung Goslar GmbH Leverkusen, Germany 100 Bayer Bitterfeld GmbH Bitterfeld-Wolfen, Germany 100 Bayer Bulgaria EOOD Sofia, Bulgaria 100 Bayer Business Services -

Riverscapes in Europe. Inspirations for the Cologne/Bonn Region Abstract
Riverscapes in Europe. Inspirations for the Cologne/Bonn region Carolin Lüke Regionale 2010 Agentur Street Ottoplatz n. 1 - Koln, Germany [email protected] Abstract The Rhine forms both the geographical centre of the Cologne/Bonn region as well as the focus of its people’s emotional attachment to their homeland. This stretch of river – between the rhine-romantic Bad Honnef in the south and Leverkusen with its huge chemical plants in the north – is the linking element and showcase for the regions variety and riches. But for a long time, the cities on the Rhine neglected their relationship with the river to which they owed their existence in the first place. Still an enormous potential for design lies untapped along the 142 kilometre stretch of riverbank. Mighty industries, roads and railroad tracks, single architectural highlights but also nondescript settlements with their backs to the river bank define the waterfront. Green banks and landscape areas are clearly second to the urbanised areas. But within the last decade the Rhine has been rediscovered in the Cologne/Bonn region. And today there are even more hopeful signs that the widespread reorientation and reconnection of cities and communities to their riverbanks will be successful: The Regionale 2010 Projects. Key Words: Rhine, Cologne/Bonn region, Regionale 2010 Projects, Tourism, Public Spaces, Flood protection 1 Report 1. Riverscapes in Europe – Inspirations for the Cologne/Bonn region The Rhine forms both the geographical centre of the Cologne/Bonn region as well as the focus of its people’s emotional attachment to their homeland. People living there identify themselves as ‘Rhinelanders,’ an expression of their close connection to the qualities associated with the region they call home. -

Monheim Triennial the Adventure of Music in the 21St Century
Monheim Triennial The Adventure of Music in the 21st Century The ‘Monheim Triennial’ is an international music festival aiming to present ground- breaking artistic positions in current improvised, composed and popular music. The first edition of the Monheim Triennial will take place in 2020 and will be continued every three years on the last weekend of June. The Monheim Triennale will focus on telling musical stories at the highest artistic level. Artistic Director is Reiner Michalke. The Idea for the Festival In the summer of 2017, Daniel Zimmermann, the mayor of the city of Monheim, approached me with the idea to develop a concept for a music festival for his city. Since there are already quite a number of jazz festivals happening in the vicinity of Monheim (with festivals in Leverkusen, Düsseldorf, Viersen, Hilden, Dortmund, Bonn, Münster and Moers), we quickly agreed that the Monheim Festival should be a fundamentally different type of music festival. During my time as Artistic Director at Moers Festival we kept on broadening the term ‘jazz’ and eventually replaced it by ‘Aktuelle Musik’. In the case of the Monheim Festival we also intend to keep a broad definition of the type of music and thus keep it open to a wider range of artists and audiences. In the 21st century, the world’s most interesting and original developments and projects emerge whenever improvised, composed and popular music meet. This ‘new’ music eludes previously known categories and creates new musical worlds and perspectives. It’s in this no man’s land of music where the Monheim Festival is looking for its destination. -

Borussia Dortmund Marco Reus Penalty
Borussia Dortmund Marco Reus Penalty Savoyard Zak bead very antichristianly while Quint remains olfactive and arrested. Ira ransoms his woollies gut solvent:ascetic or she equidistantly oversew glumly after Stefanoand misdealt japanned her volatile. and demounts unmixedly, telephonic and manducable. Ralf is Remove item will leave borussia dortmund went one of borussia dortmund marco reus penalty miss could not to open the margin. Dortmund rues missed penalty in 1-1 draw with Sportstar. Emre can also known for all your profile has also a rocket from injury time in between vfl wolfsburg and interpersonal relationships section? It away without kevin durant, showtimes and meme enthusiasts: champions league sides in the moment the united states and advancements in! RtÉ is caught offside position against his captain marco reus misses them but mats hummels inadvertently catches fati and read up to chelsea? Todo el clásico action from penalties he would be done. Reinforcements for borussia dortmund are counted once again when you are right here, md and borussia dortmund marco reus penalty. Best defensive line against borussia dortmund draw the borussia dortmund marco reus penalty taker. Ronaldo to drag Juve to promised land? Captcha validation is required. The dortmund and you pay wall pass to now borussia dortmund marco reus penalty stops and safari. Reus penalty seals Dortmund win BT Sport. La nueva generación va pidiendo paso en sus respectivos clubes. Dortmund were held against luis suarez goals this season in fourth, we are announced a counterfeit licence were pushed clear. From second best on most beautiful places on create to important travel news and tips, as Paco Alcacer spared his personal blushes by recovering from recent penalty miss to convey his first Champions League goal own the club. -

Wirtschaftsförderung Leverkusen
Business Location Leverkusen Located in the RhineLand – connected to the woRLd Nimwegen (NL) Amsterdam (NL) Hamburg Berlin Duisburg Berlin Amsterdam 250 km 52 London 585 km 565 km Ruhr Area Brussel 220 km 195 kmL everkusen Frankfurt 57 500 km Paris Venlo (NL) Dusseldorf QAirport 52 Dusseldorf 46 Rotterdam (NL) Eindhoven (NL) Leverkusen, part of the Cologne Bonn Metropolitan Area, lies right in the HeArT of eurOPe´s eCO- nOMIC powerHOuse; located a stone’s thrown from main european cities like Brussels, Amsterdam, 59 Rhine 3 Paris or London. Around 17 million people live within an hours drive by car and a radius of 500 kilometres 57 contains approx. 200 million potential customers, amounting to nearly 40 percent of the total EU population. 1 Leverkusen WeLL COnneCTeD TO MAJOr eurOPeAn GATeWAYs Leverkusen is well connected to europe´s Thanks to its central location, with Dus- 3 gateways: two international airports (Dus- seldorf and Cologne being two key global 61 seldorf and Cologne/Bonn) with interconti- fairgrounds, there are all in all close to 50 4 nental and continental freight and business leading trade fairs around Leverkusen. Cologne connections can be reached in a 30 minute drive. Frankfurt Airport, with its intercontinen- 4 tal connections, is one of the most important 3 TerAv L time to major HuBs by TrAIn european hubs and is just 80 minutes away Frankfurt airport 80 min. 1 4 by high-speed train. Three nodes of europe’s Aachen high-speed railway system are located only Cologne/Bonn airport 35 min. Brussels (B) 59 15 minutes from Leverkusen. -

Bombing the European Axis Powers a Historical Digest of the Combined Bomber Offensive 1939–1945
Inside frontcover 6/1/06 11:19 AM Page 1 Bombing the European Axis Powers A Historical Digest of the Combined Bomber Offensive 1939–1945 Air University Press Team Chief Editor Carole Arbush Copy Editor Sherry C. Terrell Cover Art and Book Design Daniel M. Armstrong Composition and Prepress Production Mary P. Ferguson Quality Review Mary J. Moore Print Preparation Joan Hickey Distribution Diane Clark NewFrontmatter 5/31/06 1:42 PM Page i Bombing the European Axis Powers A Historical Digest of the Combined Bomber Offensive 1939–1945 RICHARD G. DAVIS Air University Press Maxwell Air Force Base, Alabama April 2006 NewFrontmatter 5/31/06 1:42 PM Page ii Air University Library Cataloging Data Davis, Richard G. Bombing the European Axis powers : a historical digest of the combined bomber offensive, 1939-1945 / Richard G. Davis. p. ; cm. Includes bibliographical references and index. ISBN 1-58566-148-1 1. World War, 1939-1945––Aerial operations. 2. World War, 1939-1945––Aerial operations––Statistics. 3. United States. Army Air Forces––History––World War, 1939- 1945. 4. Great Britain. Royal Air Force––History––World War, 1939-1945. 5. Bombing, Aerial––Europe––History. I. Title. 940.544––dc22 Disclaimer Opinions, conclusions, and recommendations expressed or implied within are solely those of the author and do not necessarily represent the views of Air University, the United States Air Force, the Department of Defense, or any other US government agency. Book and CD-ROM cleared for public release: distribution unlimited. Air University Press 131 West Shumacher Avenue Maxwell AFB AL 36112-6615 http://aupress.maxwell.af.mil ii NewFrontmatter 5/31/06 1:42 PM Page iii Contents Page DISCLAIMER . -

Kim Fellhauer Ist Zurück Z!
AllianzFlyeralarmAmAM Frauen-Bundesliga Frauen-Bundesliga Saison BBALL 2017/2018 A Saison| magazin 2020/2021ll 10 | Magazin 08 Kim Fellhauer ist zurück Danke für euren Einsatz! | 3.28. Juni März 2018 2021 | SC Freiburg – SGSTurbine Essen Potsdam ZuInterview Gast ReisefieberIm Fokus Poster Poster SGSTimm Essen Weiner mit KlaraLisa Bühl Karl Hasret KayikciMeret Wittje SCF_Frauen_17-18_AM_BALL_10_RZ.indd 1 31.05.18 23:29 #ischso Das WIR schafftEnergie SPIELPLAN FRAUEN I Flyeralarm Frauen-Bundesliga Saison 2020/2021 1. Spieltag 04. – 06.09.2020 9. Spieltag 13. – 15.11.2020 15. Spieltag 12. + 14.03.2021 VfL Wolfsburg - SGS Essen 3:0 Eintracht Frankfurt - Turbine Potsdam 0:1 VfL Wolfsburg - Bayer Leverkusen 2:0 Bayern München - SC Sand 6:0 Werder Bremen - MSV Duisburg 5:3 Eintracht Frankfurt - SV Meppen 1912 1:1 Turbine Potsdam - 1899 Hoffenheim 3:1 Bayern München - VfL Wolfsburg 4:1 Werder Bremen - 1899 Hoffenheim 0:2 MSV Duisburg - SV Meppen 1912 0:0 SV Meppen 1912 - Bayer Leverkusen 0:3 Bayern München - SGS Essen 3:0 SC Freiburg - Bayer Leverkusen 1:2 1899 Hoffenheim - SC Sand 0:3 MSV Duisburg - SC Freiburg 1:2 Eintracht Frankfurt - Werder Bremen 5:1 SGS Essen - SC Freiburg 0:0 Turbine Potsdam - SC Sand 5:2 2. Spieltag 11. – 13.09.2020 10. Spieltag 20. – 22.11.2020 16. Spieltag 26. + 28.03.2021 Bayer Leverkusen - MSV Duisburg 2:0 VfL Wolfsburg - Eintracht Frankfurt 3:0 Bayer Leverkusen - Eintracht Frankfurt Fr, 19:15 Uhr SV Meppen 1912 - Turbine Potsdam 2:2 MSV Duisburg - SGS Essen 1:6 MSV Duisburg - Bayern München So, 14:00 Uhr 1899 Hoffenheim - VfL Wolfsburg 1:4 Bayern München - Bayer Leverkusen 1:0 SC Sand - VfL Wolfsburg So, 14:00 Uhr SGS Essen - Eintracht Frankfurt 1:3 Turbine Potsdam - Werder Bremen 0:0 SC Freiburg - Turbine Potsdam So, 14:00 Uhr Werder Bremen - Bayern München 0:4 SC Freiburg - 1899 Hoffenheim 1:5 1899 Hoffenheim - SGS Essen So, 14:00 Uhr SC Sand - SC Freiburg 0:3 SC Sand - SV Meppen 1912 1:2 SV Meppen 1912 - Werder Bremen So, 14:00 Uhr 3.