The Care of Your Back
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Linked: Breathing & Postural Control
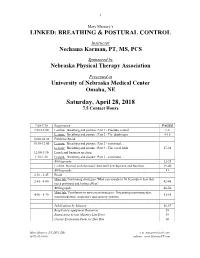
i Mary Massery’s LINKED: BREATHING & POSTURAL CONTROL Instructor Nechama Karman, PT, MS, PCS Sponsored by Nebraska Physical Therapy Association Presented at University of Nebraska Medical Center Omaha, NE Saturday, April 28, 2018 7.5 Contact Hours 7:00-7:30 Registration PAGES 7:30-10:00 Lecture: Breathing and posture: Part 1 - Pressure control 1-8 Lecture: Breathing and posture: Part 2 - The diaphragm 9-16 10:00-10:30 Exhibitor Break 10:30-12:00 Lecture: Breathing and posture: Part 2 - continued… Lecture: Breathing and posture: Part 3 - The vocal folds 17-21 12:00-1:30 Lunch and business meeting 1:30-2:30 Lecture: Breathing and posture: Part 3 - continued… Bibliography 22-28 Lecture: Normal and abnormal chest wall development and function 29-40 Bibliography 41 2:30 - 2:45 Break Mini-lab: Positioning strategies: What can you do in 90 Seconds or less that 2:45 - 4:00 42-45 has a profound and lasting effect? Bibliography 46-50 Mini-lab: Ventilatory or movement strategies: Integrating neuromuscular, 4:00 - 5:30 51-55 musculoskeletal, respiratory and sensory systems Publications by Massery 56-57 Respiratory equipment Resources 58 Instructions to join Massery List Serve 59 Course Evaluation Form for Day One 60 Mary Massery, PT, DPT, DSc e-m: [email protected] (847) 803-0803 website: www.MasseryPT.com ii COURSE DESCRIPTION This course will challenge the practitioner to make a paradigm shift: connecting breathing mechanics and postural control with management of trunk pressures. Through Dr. Massery’s model of postural control (Soda Pop Can Model), the speaker will link breathing mechanics with motor and physiologic behaviors (a multi-system perspective). -

Posture Alignment and the Surrounding Musculature An
Posture Alignment and the Surrounding Musculature An Honors Thesis (HONR 499) by Brittany Moffett Thesis Advisor Mary Winfrey-Kovell Ball State University Muncie, Indiana November 2019 Expected Date of Graduation December 2019 Abstract It is reported that musculoskeletal conditions are the most common reason to seek medical consultations in the U.S., therefore, it is important to find the underlying cause of the pain and discomfort that society is experiencing (Osar, 2012). When examining the musculoskeletal system and how it is interconnected with the nervous system, it can be found that society as a whole experiences dysfunction from simple everyday movement patterns that can lead to injury and pain (Page, 2014). One’s posture is critical to health and wellness, and activities of daily living as the core and the spine are crucial in determining how the rest of the body moves and functions. The position of the spine is determined by the neuromuscular system surrounding the spine and along the kinetic chain which affects an individual’s movement patterns. Evidence indicates any small deviation along the kinetic chain will result in change to the neuromuscular system and the increased risk of injury or pain. Because posture and the risk of injury or pain are correlated, it is critical to be able to differentiate between good posture and the different types of posture deviations. The purpose of this paper is to define good posture and provide an understanding of the underlying causes of postural deviations. An analysis of the four types of postural deviations – lordosis, kyphosis, flat back, and sway back will provide the ability to recognize the common types of postural deviations and provide a structured approach to correcting each type of postural deviation. -
Postural Deviations
Postural Deviations Kinesiology RHS 341 Lecture 11 Dr. Einas Al-Eisa Faulty posture Postural deviation can happen with either an increase or decrease of the normal body curves, leading to: • Uneven pressure within the joint surfaces • Ligaments will be under strain • Muscles may need to work harder (to hold the body upright) •Painmay occur Postural assessment • In standing: straight vertical alignment of the body from the top of the head, through the body's center, to the bottom of the feet • From a side view: imagine a vertical line through the ear, shoulder, hip, knee, and ankle. In addition, the three natural curves in the back can be imagined Postural assessment • From a back view: the spine and head are straight, not curved to the right or left • From the front: appears equal heights of shoulders, hips, and knees. The head is held straight, not tilted or turned to one side Scoliosis • = lateral curvature of the spine: • The scoliotic curve may be: ¾a single curve (C shaped) Or ¾two curves (S shaped) Scoliosis Types 1. Idiopathic scoliosis: • The most common type • Unknown cause • Sometimes called “adolescent” scoliosis because it occurs most often in adolescents (80% of all idiopathic scoliosis cases) • The other 20% are either “infantile” (from birth to 3 years old), or “juvenile” (from 3 to 9 years old) Scoliosis Types 2. Degenerative scoliosis: • Sometimes called “adult” scoliosis because it is associated with aging (develops as the person gets older) • Due to degeneration of the intervertebral discs and facet joints Scoliosis Types 3. Neuromuscular (myopathic) scoliosis: • Patients often can not walk as a result of a neuromuscular condition • Develops due to: ¾weakness of the spinal muscles (e.g., muscular dystrophy) ¾neurological problem (e.g., cerebral palsy) Scoliosis Types 4. -

Kinesiology Taping with Exercise Does Not Provide Additional Improvement in Round Shoulder Subjects with Impingement Syndrome: A
Physical Therapy in Sport 40 (2019) 99e106 Contents lists available at ScienceDirect Physical Therapy in Sport journal homepage: www.elsevier.com/ptsp Original Research Kinesiology taping with exercise does not provide additional improvement in round shoulder subjects with impingement syndrome: A single-blinded randomized controlled trial * Fu-Jie Kang a, Yuan-Chun Chiu a, Shu-Chi Wu a, Tyng-Guey Wang b, Jing-lan Yang b, , ** Jiu-Jenq Lin a, b, a School and Graduate Institute of Physical Therapy, College of Medicine, National Taiwan University, Taiwan b Division of Physical Therapy, Department of Physical Medicine and Rehabilitation, National Taiwan University Hospital, Taiwan article info abstract Article history: Objective: Round shoulder posture (RSP) may exaggerate symptoms of subacromial impingement. The Received 27 June 2019 effects of kinesiology taping with exercise on posture, pain, and functional performance were investi- Received in revised form gated in subjects with impingement and RSP. 2 September 2019 Design: This study was a single-blinded randomized controlled trial. Accepted 2 September 2019 Setting: An outpatient rehabilitation clinic in a university hospital. Participants: Thirty-four subjects with subacromial impingement and RSP. Keywords: Interventions: Kinesiology taping with and without tension was applied 2 times per week for 4 weeks. Shoulder impingement syndrome Posture Both groups also performed strengthening and stretching exercises 3 times per week for 4 weeks. Kinesio tape Main outcome measurements: The pain level, shoulder angle and self-reported score were evaluated at pre-intervention, 2-week post-intervention and 4-week post-intervention time points. Results: Functional performance improved after intervention in both groups (p ¼ 0.027). -

Treatment of the Sportsman's Groin' British Hernia Society Position
Consensus statement Br J Sports Med: first published as 10.1136/bjsports-2013-092872 on 22 October 2013. Downloaded from ‘Treatment of the Sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference Aali J Sheen,1 B M Stephenson,2 D M Lloyd,3 P Robinson,4 D Fevre,5 H Paajanen,6 A de Beaux,7 A Kingsnorth,8 O J Gilmore,9 D Bennett,10 I Maclennan,1 PO’Dwyer,11 D Sanders,8 M Kurzer12 For numbered affiliations see ABSTRACT groin.6 Chronic groin pain is most often found in end of article. Introduction The aim was to produce a athletes who undertake sports involving kicking 7 Correspondence to multidisciplinary consensus to determine the current and twisting movements while running. The pain Aali J Sheen, Honorary Senior position on the nomenclature, definition, diagnosis, is often experienced at the common point of origin Lecturer, University of imaging modalities and management of Sportsman’s of the rectus abdominis muscle and the adductor Manchester and Consultant groin (SG). longus tendon on the pubic bone and the insertion Surgeon, Department of Methods Experts in the diagnosis and management of of the inguinal ligament on the pubic bone.5 Surgery, Central Manchester Foundation Trust, Manchester SG were invited to participate in a consensus conference Furthermore, it is important to remember that Royal Infirmary, Manchester held by the British Hernia Society in Manchester, UK on there is to date no clear consensus as to what spe- M13 9WL, UK; 11–12 October 2012. Experts included a physiotherapist, cifically constitutes this diagnosis8 and in addition [email protected] a musculoskeletal radiologist and surgeons with a proven it has been recognised that treatment relies on both track record of expertise in this field. -

What Is Scoliosis?
Back Problems Screening & Prevention Tips Backache Each year as many as 25 million Americans seek a doctor’s care for backache Good fitness can help the back work efficiently Some back problems are related to poor posture Back Problems Backache is a health problem caused by not doing enough physical activity (hypokinetic condition), because weak and short muscles are linked to some types of back problems Poor posture is associated with muscles that are not strong or long enough Sometimes backache can be caused by doing too much physical activity (hyperkinetic condition - overuse injury) How does the back operate Body parts are efficiently? balanced like blocks on legs. The pelvis is a first block on legs. The chest hangs from spine and is balanced over the pelvis. The spine connects head and legs. The head sits on top of the spine and is balanced over the other blocks in the stack. Since the spine is flexible and can move back and forth, the pull of muscles keeps the body parts balanced. Muscles play an important role in holding a balance . If muscles on one side are weak and long, while muscles on the opposite side are strong and short, the body parts are pulled off balance. Posture Problems Too much arch in the lower back is LORDOSIS, also called swayback, results when the abdominal muscles are weak and the iliopsoas muscles are too strong and too short. It can lead to backache. KYPHOSIS occur in thoracic part of the spine, by poor posture: rounded back. What is Scoliosis? Everyone's spine has natural curves. -

Posture Types – Part 3
Posture types – Part 3 Flat-back posture Flat-back posture is the lack of mobility and flattening of the lumbar spine. The features are as follows: Head is forward Cervical spine is slightly extended The rectus abdominis and external obliques (EO) are tight and become the most dominant of the abdominal muscles The hamstrings are tight The one-joint hip flexors are found to be long and weak The pelvis is posteriorly tilted Back erectors are slightly stretched Knees are slightly flexed Flat-back posture is common in: People who tend to perform lots of ‘sit-up’ type of exercises Boxers People with poor core and back stability and who have had long periods of inactivity Guidelines for the correction of flat-back posture: Regain mobility in the lumbar spine Use strengthening exercises for the lower back Stretch the hamstrings Strengthen/shorten the hip flexors Stretch the rectus abdominis – ideally over a stability ball Suitable Pilates exercises: Pelvic tilts, Shoulder bridge, rolling back Swan dive, swimming, spine twist Half and full Roll up, chest opener Focus on set up position and realigning cervical spine Focus on stretching hamstrings Sway-back posture Posture features are as follows: Head/chin is held forward Cervical spine is slightly extended; neck flexors are weak Thoracic spine has increased flexion (kyphotic); thoracic extensors are weak Lumbar spine is flexed (flat lower back) Posterior tilted pelvis – pelvis is swayed forward in relation to the feet Hip flexors are long and weak Obliques (upper fibres) -

Postural Aberrations in Low Back Pain Heather J
218 Postural Aberrations in Low Back Pain Heather J. Christie, MSc(PT), Shrawan Kumar, PhD, Sharon A. Warren, PhD ABSTRACT. Christie H J, Kumar S, Warren S. Postural aberrations in low back pain. Arch Phys Med Rehabil 1995;76:218-24. • The purpose of this study was to measure and describe postural aberrations in chronic and acute low back pain in search of predictors of low back pain. The sample included 59 subjects recruited to the following three groups: chronic, acute, or no low back pain. Diagnoses included disc disease, mechanical back pain, and osteoarthritis. Lumbar lordosis, thoracic kyphosis, head position, shoulder position, shoulder height, pelvic flit, and leg length were measured using a photographic technique. In standing, chronic pain patients exhibited an increased lumbar lordosis compared with controls (p < .05). Acute patients had an increased thoracic kyphosis and a forward head position compared with controls (p < .05). In sitting, acute patients had an increased thoracic kyphosis compared with controls (p < .05). These postural parameters identified discrete postural profiles but had moderate value as predictors of low back pain. Therefore other unidentified factors are also important in the prediction of low back pain. © 1995 by the American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation Low back pain is a significant problem in today's society, forces) on the joints that lead to excessive wear of the articu- with lifetime incidence rates reported between 50% and lar surfaces. 1°'16 With postural changes, a change in align- 90%. 1-3 Low back pain has recurrence rates of up to 90% 4,5 ment with respect to the line of gravity occurs that may lead even though many cases are self-limiting and require mini- to other adaptive postural changesJ 6'17 mal treatment. -

Bachelor of Science in Athletic Training Student Handbook 2018-2019 Academic Year
Bachelor of Science in Athletic Training Student Handbook 2018-2019 Academic Year Policies in this handbook are for all Pre-Athletic Training, and Athletic Training Majors In addition to this handbook, students are to refer to the College of Health and Human Services Student Handbook and the UNC Charlotte Undergraduate Catalog Table of Contents UNC Charlotte’s Athletic Training Education Program 4 Vision Statement 4 Mission Statement 4 Program Goals and Objectives 5 Accreditation Status 20 Faculty Information 21 Introduction to Athletic Training 22 The Athletic Training Profession 22 Regulation of Athletic Training 22 Essential Functions of an Athletic Trainer 23 UNC Charlotte’s Athletic Training Education Program Curriculum 24 Prerequisite Requirements 24 Course Sequence – Upper Division Athletic Training Major 25 Suggested 4 – year Course Sequence 26 Course Descriptions 28 Athletic Training Education Program Clinical Coursework 30 Athletic Training Education Program Clinical Education Faculty 32 Athletic Training Education Program Affiliated Clinical Sites 33 Athletic Training Program Student Policies and Procedures 34 Academic Advising 34 Athletic Training Education Program General Admission Requirements 35 Athletic Training Education Program Application Requirements 36 Athletic Training Education Program Procedures for Admission 37 Athletic Training Education Program Required Costs 38 Athletic Training Education Program Progression and Retention Policy 39 Bachelor of Science in Athletic Training Degree Graduation 41 Requirements Athletic -

The Anatomical “Core”: a Definition and Functional Classification
Osteopathic Family Physician (2011) 3, 239-245 The anatomical “core”: a definition and functional classification John J. Dougherty, DO, FACOFP, FAOASM From the Department of Family Medicine, Kansas City University of Medicine and Biosciences, Kansas City, MO. KEYWORDS: The anatomic core is important in the functional stabilization of the body during static and dynamic Core; movement. This functional stabilization is an integral component of proprioception, balance perfor- Static function; mance, and compensatory postural activation of the trunk muscles. The structures that define the core Dynamic function; and its functions are presented here. By understanding the contributing components and responsibilities Sensory-motor control of the core, it is hoped that the physician will have a better understanding of core function as it relates to the performance of their patients’ activities of daily living. © 2011 Elsevier Inc. All rights reserved. Core training has found its way into the lexicon of functional unit, synergistically adjusting the entire body to countless exercise regimens. However, clinically there has maintain balance, postural stabilization, and mobility. These been little comprehensive definition and even less practical abilities are essential in the performance of basic activities characterization of this “core.” The word core derives from of daily living (ADLs).7 the Greek word kormos, which loosely translates to “trunk Neurologic and musculoskeletal impairments can alter of a tree.” An additional word origin comes from the Span- these normal biomechanical relationships.8-10 Such impair- ish word for heart, corazon. George Lucas selected “Cora- ment effects a functional shift of the structural burden to the zon” as the name for the planet at the center of his “Star components of the core.1 The resultant alterations impose Wars” universe. -

Low Back Pain Sometime During Their Lifetime
DESCRIPTION: Eighty percent of adults will experience significant low back pain sometime during their lifetime. Low back pain usually involves muscle spasm of the supportive muscles along the spine. Also, pain, numbness and tingling in the buttocks or lower extremity can be related to the back. There are multiple causes of low back pain (see below). Prevention of low back pain is extremely important, as symptoms can recur on more than one occasion. COMMON CAUSES: Muscle strain. The muscles of the low back provide the strength and mobility for all activities of daily living. Strains occur when a muscle is overworked or weak. Ligament sprain. Ligaments connect the spinal vertebrae and provide stability for the low back. They can be injured with a sudden, forceful movement or prolonged stress. Poor posture. Poor postural alignment (such as slouching in front of the TV or sitting hunched over a desk) creates muscular fatigue, joint compression, and stresses the discs that cushion your vertebrae. Years of abuse can cause muscular imbalances such as tightness and weakness, which also cause pain. Age. “Wear and tear” and inherited factors may cause degenerative changes in the discs (called degenerative disc disease), and joint degeneration of the facet joints of the spine (called degenerative joint disease). Normal aging causes decreased bone density, strength and elasticity of muscles and ligaments. These effects can be minimized by regular exercise, proper lifting and moving techniques, proper nutrition and body composition, and avoidance of smoking. Disc bulge. or herniation, can cause pressure on a nerve, which can radiate pain down the leg. -

Role of Global Postural Re-Education in Non Specific Low Back Pain
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.10.001901 Arvind Kumar. Biomed J Sci & Tech Res Mini Review Open Access Role of Global Postural Re-Education in Non Specific Low Back Pain Arvind Kumar* MPT(Orthopedics), Swarnim Startup & Innovation University, India Received: : October 03, 2018; Published: : October 16, 2018 *Corresponding author: Arvind Kumar, MPT(Orthopedics), Swarnim Startup & Innovation University, Gujarat, India Abstract Past injuries and repetitive activities lead to accumulated muscle tension and strain, forcing us to create compensations to avoid pain. Static muscles are responsible to keep these compensations, and as a result, they stiffen up, get shortened, and become defectively recruited by poor and misalignment, soft tissue stiffness, nerve entrapment, and altered posture awareness. coordination. If their proper function and flexibility are not restored, they progress to further muscular tension, causing aches, joint compression Introduction Global Postural Re-Education (GPR) is a therapeutic method Non-Specific Low Back Pain - which is exclusively manual for the correction and treatment of Approximately 70-85% of individuals will experience low pathologies in the musculoskeletal system. GPR was created in 1980 back pain (LBP) during their lifetime, and over 80% of them will by the French physiotherapist Philippe Emmanuel Souchard. RPG is report recurrent episodes. It is estimated that 80-90% of subjects a treatment approach that aims to evaluate and manually treat the will recover within 6 weeks, regardless of the type of treatment; human body as a whole. The goal is to track back from the symptoms to the cause by following the muscular chains, and correcting it little pain is characterized by the absence of structural change; that is however, 5-15% will develop chronic LBP.