Infectious Disease Cutaneous Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Naeglaria and Brain Infections
Can bacteria shrink tumors? Cancer Therapy: The Microbial Approach n this age of advanced injected live Streptococcus medical science and into cancer patients but after I technology, we still the recipients unfortunately continue to hunt for died from subsequent innovative cancer therapies infections, Coley decided to that prove effective and safe. use heat killed bacteria. He Treatments that successfully made a mixture of two heat- eradicate tumors while at the killed bacterial species, By Alan Barajas same time cause as little Streptococcus pyogenes and damage as possible to normal Serratia marcescens. This Alani Barajas is a Research and tissue are the ultimate goal, concoction was termed Development Technician at Hardy but are also not easy to find. “Coley’s toxins.” Bacteria Diagnostics. She earned her bachelor's degree in Microbiology at were either injected into Cal Poly, San Luis Obispo. The use of microorganisms in tumors or into the cancer therapy is not a new bloodstream. During her studies at Cal Poly, much idea but it is currently a of her time was spent as part of the undergraduate research team for the buzzing topic in cancer Cal Poly Dairy Products Technology therapy research. Center studying spore-forming bacteria in dairy products. In the late 1800s, German Currently she is working on new physicians W. Busch and F. chromogenic media formulations for Fehleisen both individually Hardy Diagnostics, both in the observed that certain cancers prepared and powdered forms. began to regress when patients acquired accidental erysipelas (cellulitis) caused by Streptococcus pyogenes. William Coley was the first to use New York surgeon William bacterial injections to treat cancer www.HardyDiagnostics.com patients. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Hawaii State Department of Health Tetanus Factsheet
TETANUS ABOUT THIS DISEASE Tetanus is an infection caused by a bacterium called Clostridium tetani. Spores of tetanus bacteria are everywhere in the environment, including soil, dust, and manure. These spores develop into bacteria when they enter the body through breaks in the skin, usually through injuries from contaminated objects. Clostridium tetani produce a toxin (poison) that causes painful muscle contractions. Tetanus is often called “lockjaw” because the first sign is most commonly spasms of the jaw muscles. Tetanus can lead to serious health problems, including being unable to open the mouth and having trouble swallowing and breathing, possibly leading to death (10% to 20% of cases). Tetanus is uncommon in the United States, with an average of 30 reported cases each year. Nearly all cases of tetanus in the U.S. are among people who have never received a tetanus vaccine, or adults who don’t stay up to date on their 10-year booster shots. SIGNS AND SYMPTOMS Symptoms of tetanus include: • Jaw cramping • Sudden, involuntary muscle tightening (muscle spasms) – often in the stomach • Painful muscle stiffness all over the body • Trouble swallowing • Jerking or staring (seizures) • Headache • Fever and sweating • Changes in blood pressure and a fast heart rate. Serious health problems that can happen because of tetanus include: • Laryngospasm (uncontrolled/involuntary tightening of the vocal cords) • Fractures (broken bones) • Hospital-acquired infections (Infections caught by a patient during a hospital stay) • Pulmonary embolism (blockage of the main artery of the lung or one of its branches by a blood clot that has travelled from elsewhere in the body through the bloodstream) • Aspiration pneumonia (lung infection that develops by breathing in foreign materials) • Breathing difficulty, possibly leading to death (1 to 2 in 10 cases are fatal) TRANSMISSION Tetanus is different from other vaccine-preventable diseases because it does not spread from person to person. -

Safety and Immunogenicity of Capsular Polysaccharide–Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib
142 Safety and Immunogenicity of Capsular Polysaccharide±Tetanus Toxoid Conjugate Vaccines for Group B Streptococcal Types Ia and Ib Carol J. Baker, Lawrence C. Paoletti, Section of Infectious Diseases, Departments of Pediatrics and of Michael R. Wessels, Hilde-Kari Guttormsen, Microbiology and Immunology, Baylor College of Medicine, Houston, Marcia A. Rench, Melissa E. Hickman, Texas; Channing Laboratory, Department of Medicine, Brigham and Women's Hospital, and Department of Microbiology and Molecular and Dennis L. Kasper Genetics, Harvard Medical School, Boston, Massachusetts About 40% of invasive group B streptococcal (GBS) isolates are capsular polysaccharide Downloaded from https://academic.oup.com/jid/article/179/1/142/877598 by guest on 01 October 2021 (CPS) types Ia or Ib. Because infant and maternal GBS infections may be preventable by maternal vaccination, individual GBS CPS have been coupled to tetanus toxoid (TT) to prepare vaccines with enhanced immunogenicity. Immunogenicity in rabbits and protective capacity in mice of a series of type Ia- and Ib-TT conjugates increased with the degree of polysaccharide-to-protein cross-linking. In total, 190 healthy, nonpregnant women aged 18±40 years were randomized in four trials to receive Ia- or Ib-TT conjugate (dose range, 3.75±63 mg of CPS component), uncoupled Ia or Ib CPS, or saline. All vaccines were well-tolerated. CPS-speci®c IgG serum concentrations peaked 4±8 weeks after vaccination and were signif- icantly higher in recipients of conjugated than of uncoupled CPS. Immune responses to the conjugates were dose-dependent and correlated in vitro with opsonophagocytosis. These re- sults support inclusion of Ia- and Ib-TT conjugates when formulating a multivalent GBS vaccine. -

Gonorrhea Can Be Easily Cured with Antibiotics from a If You Are Pregnant, It Is Even More Important to Get Health Care Provider
GET YOURSELF TESTED Testing is confidential. If you are under 18 years old, you can consent to be checked and treated for STIs. What if I don’t get treated? What if I am pregnant? Gonorrhea can be easily cured with antibiotics from a If you are pregnant, it is even more important to get health care provider. tested by your health care provider and treated if you have gonorrhea. Left untreated, gonorrhea can be However, if gonorrhea is not treated, it can cause Gonorrhea passed to your baby during vaginal delivery and can permanent damage: cause serious health problems. • Your risk of getting other STIs, like gonorrhea or • Babies are usually treated with an antibiotic HIV increases. shortly after birth. If a baby with gonorrhea isn’t • In females, untreated gonorrhea can increase the treated, they may become blind. chances of getting pelvic inflammatory disease (PID), an infection of the reproductive organs, which can make it hard to get pregnant or carry a To learn more baby full-term. Contact a health care provider or your local STI clinic. • In males, untreated gonorrhea can lead to sterility To learn more about STIs, or to find your local (inability to make sperm and have children). STI clinic, visit www.health.ny.gov/STD. You can find other STI testing locations at What about my sex partner(s)? https://gettested.cdc.gov. Gonorrhea is a sexually transmitted infection. If you have gonorrhea, your sex partner(s) should get tested. If they have gonorrhea, they will need to take medicine to cure it. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Get the Facts About Necrotizing Fasciitis: “Flesh-Eating Disease”
Get the facts about necrotizing fasciitis: “Flesh-eating Disease” What is necrotizing fasciitis? There are many strains of bacteria that can cause the flesh-eating disease known as necrotizing fasciitis, but most cases are caused by a bacteria called group A strep, or Streptococcus pyogenes. More common infections with group A strep are not only strep throat, but also a skin infection called impetigo. Flesh-eating strep infections or necrotizing fasciitis is considered rare. Necrotizing fasciitis is a treatable disease. Only certain rare bacterial strains are able to cause necrotizing fasciitis, but these infections progress rapidly so the sooner one seeks medical care, the better the chances of survival. The bacteria actually cause extensive tissue damage because the tissues under the skin and those surrounding muscle and body organs are destroyed; necrotizing fasciitis is extensive and can lead to death. Is this a new disease? No. The flesh-eating infections have been described as early as the fifth century B.C. based on written accounts of necrotizing fasciitis by Hippocrates. More than 2,000 cases of this condition were reported among soldiers during the Civil War. Cases in the U.S. are generally infrequent, although small epidemics have occurred, such as the 1996 outbreak in San Francisco among injection drug abusers using contaminated “black tar” heroin. What are the signs and symptoms? Persons with the flesh-eating infection know something is wrong because of extreme pain in the infected area. Generally, an infection begins at a surgical wound or because of accidental trauma—sometimes without an obvious break in the skin—accompanied by severe pain, followed by swelling, fever, and sometimes confusion. -

What Is Staphylococcus Aureus (Staph)?
What is Staphylococcus aureus (staph)? Staphylococcus aureus, often referred to simply as "staph," are bacteria commonly carried on the skin or in the nose of healthy people. Approximately 25% to 30% of the population is colonized (when bacteria are present, but not causing an infection) in the nose with staph bacteria. Sometimes, staph can cause an infection. Staph bacteria are one of the most common causes of skin infections in the United States. Most of these skin infections are minor (such as pimples and boils) and can be treated without antibiotics (also known as antimicrobials or antibacterials). However, staph bacteria also can cause serious infections (such as surgical wound infections, bloodstream infections, and pneumonia). What is MRSA (methicillin-resistant Staphylococcus aureus)? Some staph bacteria are resistant to antibiotics. MRSA is a type of staph that is resistant to antibiotics called beta-lactams. Beta-lactam antibiotics include methicillin and other more common antibiotics such as oxacillin, penicillin and amoxicillin. While 25% to 30% of the population is colonized with staph, approximately 1% is colonized with MRSA. Who gets staph or MRSA infections? Staph infections, including MRSA, occur most frequently among persons in hospitals and healthcare facilities (such as nursing homes and dialysis centers) who have weakened immune systems. These healthcare-associated staph infections include surgical wound infections, urinary tract infections, bloodstream infections, and pneumonia. Are people who are positive for the human immune deficiency virus (HIV) at increased risk for MRSA? Should they be taking special precautions? People with weakened immune systems, which include some patients with HIV infection, may be at risk for more severe illness if they get infected with MRSA. -

Cutaneous Melioidosis Dermatology Section
DOI: 10.7860/JCDR/2016/18823.8463 Case Report Cutaneous Melioidosis Dermatology Section BASAVAPRABHU ACHAPPA1, DEEPAK MADI2, K. VIDYALAKSHMI3 ABSTRACT Melioidosis is an emerging infection in India. It usually presents as pneumonia. Melioidosis presenting as cutaneous lesions is uncommon. We present a case of cutaneous melioidosis from Southern India. Cutaneous melioidosis can present as an ulcer, pustule or as crusted erythematous lesions. A 22-year-old gentleman known case of diabetes mellitus was admitted in our hospital with an ulcer over the left thigh. Discharge from the ulcer grew Burkholderia pseudomallei. He was successfully treated with ceftazidime. Melioidosis must be considered in the differential diagnosis of nodular or ulcerative cutaneous lesion in a diabetic patient. Keywords: B. pseudomallei, Diabetes Mellitus, Skin ulcer CASE REPORT melioidosis is a rare entity. Cutaneous melioidosis may be primary A 22-year-old gentleman was admitted in our hospital with (presenting symptom is skin infection) or secondary (melioidosis complaints of an ulcer over the left thigh of seven days duration. at other sites in the body with incidental skin involvement) [3]. History of fever was present for four days. He also complained of There is limited published data from India documenting cutaneous pain in the thigh. The patient initially noticed a nodule on the left melioidosis. thigh which eventually progressed to form a discharging ulcer. He B. pseudomallei reside in soil and water [4]. Inoculation, inhalation was a known case of diabetes mellitus (type 1) on insulin. Clinical or ingestion of infected food or water are the modes of transmission examination revealed a 5cm× 5cm ulcer on the left thigh with [5]. -
Necrotizing Fasciitis
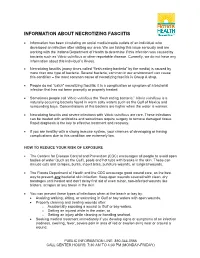
INFORMATION ABOUT NECROTIZING FASCIITIS • Information has been circulating on social media/media outlets of an individual who developed an infection after visiting our area. We are taking this issue seriously and are working with the Indiana Department of Health to determine if this infection was caused by bacteria such as Vibrio vulnificus or other reportable disease. Currently, we do not have any information about this individual’s illness. • Necrotizing fasciitis (many times called “flesh eating bacteria” by the media) is caused by more than one type of bacteria. Several bacteria, common in our environment can cause this condition – the most common cause of necrotizing fasciitis is Group A strep. • People do not “catch” necrotizing fasciitis; it is a complication or symptom of a bacterial infection that has not been promptly or properly treated. • Sometimes people call Vibrio vulnificus the “flesh eating bacteria.” Vibrio vulnificus is a naturally occurring bacteria found in warm salty waters such as the Gulf of Mexico and surrounding bays. Concentrations of this bacteria are higher when the water is warmer. • Necrotizing fasciitis and severe infections with Vibrio vulnificus are rare. These infections can be treated with antibiotics and sometimes require surgery to remove damaged tissue. Rapid diagnosis is the key to effective treatment and recovery. • If you are healthy with a strong immune system, your chances of developing or having complications due to this condition are extremely low. HOW TO REDUCE YOUR RISK OF EXPOSURE • The Centers for Disease Control and Prevention (CDC) encourages all people to avoid open bodies of water (such as the Gulf), pools and hot tubs with breaks in the skin. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA).