Draft Report on Carcinogens Monograph on Antimony Trioxide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report of the Advisory Group to Recommend Priorities for the IARC Monographs During 2020–2024
IARC Monographs on the Identification of Carcinogenic Hazards to Humans Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 CONTENTS Introduction ................................................................................................................................... 1 Acetaldehyde (CAS No. 75-07-0) ................................................................................................. 3 Acrolein (CAS No. 107-02-8) ....................................................................................................... 4 Acrylamide (CAS No. 79-06-1) .................................................................................................... 5 Acrylonitrile (CAS No. 107-13-1) ................................................................................................ 6 Aflatoxins (CAS No. 1402-68-2) .................................................................................................. 8 Air pollutants and underlying mechanisms for breast cancer ....................................................... 9 Airborne gram-negative bacterial endotoxins ............................................................................. 10 Alachlor (chloroacetanilide herbicide) (CAS No. 15972-60-8) .................................................. 10 Aluminium (CAS No. 7429-90-5) .............................................................................................. 11 -

Inventory Size (Ml Or G) 103220 Dimethyl Sulfate 77-78-1 500 Ml
Inventory Bottle Size Number Name CAS# (mL or g) Room # Location 103220 Dimethyl sulfate 77-78-1 500 ml 3222 A-1 Benzonitrile 100-47-0 100ml 3222 A-1 Tin(IV)chloride 1.0 M in DCM 7676-78-8 100ml 3222 A-1 103713 Acetic Anhydride 108-24-7 500ml 3222 A2 103714 Sulfuric acid, fuming 9014-95-7 500g 3222 A2 103723 Phosphorus tribromide 7789-60-8 100g 3222 A2 103724 Trifluoroacetic acid 76-05-1 100g 3222 A2 101342 Succinyl chloride 543-20-4 3222 A2 100069 Chloroacetyl chloride 79-04-9 100ml 3222 A2 10002 Chloroacetyl chloride 79-04-9 100ml 3222 A2 101134 Acetyl chloride 75-36-5 500g 3222 A2 103721 Ethyl chlorooxoacetate 4755-77-5 100g 3222 A2 100423 Titanium(IV) chloride solution 7550-45-0 100ml 3222 A2 103877 Acetic Anhydride 108-24-7 1L 3222 A3 103874 Polyphosphoric acid 8017-16-1 1kg 3222 A3 103695 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103694 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103880 Methanesulfonic acid 75-75-2 500ml 3222 A3 103883 Oxalyl chloride 79-37-8 100ml 3222 A3 103889 Thiodiglycolic acid 123-93-3 500g 3222 A3 103888 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 103886 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 102969 sulfuric acid 7664-93-9 500 mL 2428 A7 102970 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102971 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102973 formic acid (88%) 64-18-6 500 mL 2428 A7 102974 hydrofloric acid (49%) 7664-39-3 500 mL 2428 A7 103320 Ammonium Hydroxide conc. -

Transport of Dangerous Goods
ST/SG/AC.10/1/Rev.16 (Vol.I) Recommendations on the TRANSPORT OF DANGEROUS GOODS Model Regulations Volume I Sixteenth revised edition UNITED NATIONS New York and Geneva, 2009 NOTE The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. ST/SG/AC.10/1/Rev.16 (Vol.I) Copyright © United Nations, 2009 All rights reserved. No part of this publication may, for sales purposes, be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, electrostatic, magnetic tape, mechanical, photocopying or otherwise, without prior permission in writing from the United Nations. UNITED NATIONS Sales No. E.09.VIII.2 ISBN 978-92-1-139136-7 (complete set of two volumes) ISSN 1014-5753 Volumes I and II not to be sold separately FOREWORD The Recommendations on the Transport of Dangerous Goods are addressed to governments and to the international organizations concerned with safety in the transport of dangerous goods. The first version, prepared by the United Nations Economic and Social Council's Committee of Experts on the Transport of Dangerous Goods, was published in 1956 (ST/ECA/43-E/CN.2/170). In response to developments in technology and the changing needs of users, they have been regularly amended and updated at succeeding sessions of the Committee of Experts pursuant to Resolution 645 G (XXIII) of 26 April 1957 of the Economic and Social Council and subsequent resolutions. -

Method for Preparing 2,3-Dichloro-1-Propanol and 3-Chloro-1-Propanol
Europaisches Patentamt 19 European Patent Office Office europeen des brevets © Publication number : 0 579 362 A1 EUROPEAN PATENT APPLICATION © Application number : 93303893.7 © int. ci.5: C07C 31/36, C07C 29/32 @ Date of filing : 19.05.93 © Priority: 13.07.92 JP 184910/92 @ Inventor: Watanabe, Hiroyoshi 18.12.92 JP 338584/92 3-4-1-141, Toriishi Takaishi-shi, Osaka-fu (JP) Inventor : Hayakawa, Fumie @) Date of publication of application : 4-7-3-342, Kamo 19.01.94 Bulletin 94/03 Takaishi-shi, Osaka-fu (JP) © Designated Contracting States : © Representative : Stuart, Ian Alexander et al DE FR GB IT NL MEWBURN ELLIS 2 Cursitor Street London EC4A 1BQ (GB) © Applicant : MITSUI TOATSU CHEMICALS, Inc. 2-5 Kasumigaseki 3-chome Chiyoda-Ku Tokyo 100 (JP) © Method for preparing 2,3-dichloro-1-propanol and 3-chloro-1-propanol. © A method for preparing 2,3-dichloro-l- propanol and 23-chloro-l-propanol is here dis- closed which comprises the step of reacting 1,2-dichloroethane with methanol by irradiation with light in the presence of at least one com- pound selected from europium compounds, samarium compounds and ytterbium com- pounds, and if necessary, in the additional pre- sence of a zeolite. CM CO CO o> ro- ta LU Jouve, 18, rue Saint-Denis, 75001 PARIS 1 EP 0 579 362 A1 2 The present invention relates to a method for pre- As a method to solve these problems, the pres- paring 2,3-dichloro-1-propanol and 3-chloro-1- ent inventor have suggested a method for preparing propanol. -

An Investigation of the Crystal Growth of Heavy Sulfides in Supercritical
AN ABSTRACT OF THE THESIS OF LEROY CRAWFORD LEWIS for the Ph. D. (Name) (Degree) in CHEMISTRY presented on (Major) (Date) Title: AN INVESTIGATION OF THE CRYSTAL GROWTH OF HEAVY SULFIDES IN SUPERCRITICAL HYDROGEN SULFIDE Abstract approved Redacted for privacy Dr. WilliarriIJ. Fredericks Solubility studies on the heavy metal sulfides in liquid hydrogen sulfide at room temperature were carried out using the isopiestic method. The results were compared with earlier work and with a theoretical result based on Raoult's Law. A relative order for the solubilities of sulfur and the sulfides of tin, lead, mercury, iron, zinc, antimony, arsenic, silver, and cadmium was determined and found to agree with the theoretical result. Hydrogen sulfide is a strong enough oxidizing agent to oxidize stannous sulfide to stannic sulfide in neutral or basic solution (with triethylamine added). In basic solution antimony trisulfide is oxi- dized to antimony pentasulfide. In basic solution cadmium sulfide apparently forms a bisulfide complex in which three moles of bisul- fide ion are bonded to one mole of cadmium sulfide. Measurements were made extending the range over which the volumetric properties of hydrogen sulfide have been investigated to 220 °C and 2000 atm. A virial expression in density was used to represent the data. Good agreement, over the entire range investi- gated, between the virial expressions, earlier work, and the theorem of corresponding states was found. Electrical measurements were made on supercritical hydro- gen sulfide over the density range of 10 -24 moles per liter and at temperatures from the critical temperature to 220 °C. Dielectric constant measurements were represented by a dielectric virial ex- pression. -

General Listing Background Document for the Inorganic Chemical Listing Determination
GENERAL LISTING BACKGROUND DOCUMENT FOR THE INORGANIC CHEMICAL LISTING DETERMINATION August, 2000 U.S. ENVIRONMENTAL PROTECTION AGENCY ARIEL RIOS BUILDING 1200 PENNSYLVANIA AVENUE, N.W. WASHINGTON, D.C. 20460 TABLE OF CONTENTS Page LIST OF TABLES .............................................................ii LIST OF FIGURES ............................................................ii LIST OF APPENDICES .........................................................ii 1. INTRODUCTION .......................................................1 1.1 BACKGROUND ...................................................1 1.2 EXISTING INORGANIC CHEMICAL LISTINGS ........................2 1.3 OTHER EPA REGULATORY PROGRAMS AFFECTING THE INORGANIC CHEMICAL INDUSTRY ............................................3 2. INDUSTRY DESCRIPTION .........................................5 2.1 INDUSTRY PROFILE ..............................................5 2.2 INDUSTRY SECTORS .............................................5 2.2.1 Antimony Oxide ..............................................8 2.2.2 Barium Carbonate ............................................8 2.2.3 Boric Acid ..................................................8 2.2.4 Cadmium Pigments ............................................8 2.2.5 Inorganic Hydrogen Cyanide ....................................8 2.2.6 Phenyl Mercuric Acetate .......................................8 2.2.7 Dry Process Phosphoric Acid ....................................8 2.2.8 Phosphorous Pentasulfide .......................................8 -
Use of Bismuth Compounds for the Manufacture of Medicaments for The
Europäisches Patentamt *EP000805815B1* (19) European Patent Office Office européen des brevets (11) EP 0 805 815 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: A61K 33/24, C07F 9/94, of the grant of the patent: A61K 49/04 10.04.2002 Bulletin 2002/15 (86) International application number: (21) Application number: 96901066.9 PCT/GB96/00183 (22) Date of filing: 26.01.1996 (87) International publication number: WO 96/22994 (01.08.1996 Gazette 1996/35) (54) Use of bismuth compounds for the manufacture of medicaments for the treatment of gastric disorders caused by Helicobacter pylori Verwendung von WISMUTVERBINDUNGEN zur Herstellung eines Arzneimittels zur Behandlung von Magenverstimmungen, die durch Helicobacter pylori verursacht werden Utilisation de COMPOSES DE BISMUTH pour la fabrication de médicaments pour le traitement de troubles gastriques associées avec Helicobacter pylori (84) Designated Contracting States: EP-A- 0 480 691 EP-A- 0 716 091 DE DK ES FR GB IE IT SE WO-A-91/03241 WO-A-93/02713 WO-A-95/06053 WO-A-96/16677 (30) Priority: 26.01.1995 GB 9501560 WO-A-96/16678 BE-A- 782 105 07.06.1995 US 486225 DE-A- 2 216 725 (43) Date of publication of application: • TETRAHEDRON LETT. (TELEAY,00404039);94; 12.11.1997 Bulletin 1997/46 VOL.35 (44); PP.8197-200, KYOTO UNIV.;FAC. SCI.; KYOTO; 606-01; JAPAN (JP), SUZUKI H ET (73) Proprietor: NYCOMED IMAGING A/S AL ’Ultrasonic reaction of triarylbismuthines 0401 Oslo (NO) and triarylstibines with iodosylbenzene. Mild oxidizing ability of the organobismuth oxide (72) Inventors: function for organic substrates’ • KLAVENESS, Jo • DATABASE CHEMABS CHEMICAL ABSTRACTS N-1166 Oslo (NO) SERVICE, COLUMBUS, OHIO, US ASTHANA A • BERG, Arne ’Reactions of triphenyl antimony, bismuth and N-1300 Sandvika (NO) their dibromides with pentachlorophenol and • ALMEN, Torsten pentachlorothiophenol’ & INDIAN J. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
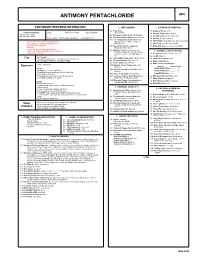
Antimony Pentachloride Apc
ANTIMONY PENTACHLORIDE APC CAUTIONARY RESPONSE INFORMATION 4. FIRE HAZARDS 7. SHIPPING INFORMATION 4.1 Flash Point: 7.1 Grades of Purity: 99+% Common Synonyms Liquid Colorless to brown Unpleasant odor Not flammable 7.2 Storage Temperature: Ambient Antimony (V) chloride 4.2 Flammable Limits in Air: Not flammable Antimony perchloride 7.3 Inert Atmosphere: No requirement 4.3 Fire Extinguishing Agents: Not pertinent Sinks in water. Irritating vapor is produced. Freezing point is 37°F. 7.4 Venting: Pressure-vacuum 4.4 Fire Extinguishing Agents Not to Be 7.5 IMO Pollution Category: Currently not available Avoid contact with liquid. Keep people away. Used: Do not use water or foam on Wear rubber overclothing (including gloves). adjacent fires. 7.6 Ship Type: Currently not available Stop discharge if possible. 4.5 Special Hazards of Combustion 7.7 Barge Hull Type: Currently not available Evacuate. Products: Not pertinent Isolate and remove discharged material. 4.6 Behavior in Fire: Irritating fumes of Notify local health and pollution control agencies. 8. HAZARD CLASSIFICATIONS hydrogen chloride given off when water Protect water intakes. or foam is used to extinguish adjacent 8.1 49 CFR Category: Corrosive material fire. 8.2 49 CFR Class: 8 Not flammable. 4.7 Auto Ignition Temperature: Not pertinent Fire POISONOUS GASES ARE PRODUCED WHEN HEATED. 8.3 49 CFR Package Group: II DO NOT USE WATER ON ADJACENT FIRES. 4.8 Electrical Hazards: Not pertinent 8.4 Marine Pollutant: No 4.9 Burning Rate: Not pertinent 8.5 NFPA Hazard Classification: Exposure Call for medical aid. 4.10 Adiabatic Flame Temperature: Not pertinent Category Classification VAPOR Health Hazard (Blue)......... -

Multivalent Metals and Polyatomic Ions 1
Name Date Comprehension Section 4.2 Use with textbook pages 189–193. Multivalent metals and polyatomic ions 1. Define the following terms: (a) ionic compound (b) multivalent metal (c) polyatomic ion 2. Write the formulae and names of the compounds with the following combination of ions. The first row is completed to help guide you. Positive ion Negative ion Formula Compound name (a) Pb2+ O2– PbO lead(II) oxide (b) Sb4+ S2– (c) TlCl (d) tin(II) fluoride (e) Mo2S3 (f) Rh4+ Br– (g) copper(I) telluride (h) NbI5 (i) Pd2+ Cl– 3. Write the chemical formula for each of the following compounds. (a) manganese(II) chloride (f) vanadium(V) oxide (b) chromium(III) sulphide (g) rhenium(VII) arsenide (c) titanium(IV) oxide (h) platinum(IV) nitride (d) uranium(VI) fluoride (i) nickel(II) cyanide (e) nickel(II) sulphide (j) bismuth(V) phosphide 68 MHR • Section 4.2 Names and Formulas of Compounds © 2008 McGraw-Hill Ryerson Limited 0056_080_BCSci10_U2CH04_098461.in6856_080_BCSci10_U2CH04_098461.in68 6688 PDF Pass 77/11/08/11/08 55:25:38:25:38 PPMM Name Date Comprehension Section 4.2 4. Write the formulae for the compounds formed from the following ions. Then name the compounds. Ions Formula Compound name + – (a) K NO3 KNO3 potassium nitrate 2+ 2– (b) Ca CO3 + – (c) Li HSO4 2+ 2– (d) Mg SO3 2+ – (e) Sr CH3COO + 2– (f) NH4 Cr2O7 + – (g) Na MnO4 + – (h) Ag ClO3 (i) Cs+ OH– 2+ 2– (j) Ba CrO4 5. Write the chemical formula for each of the following compounds. (a) barium bisulphate (f) calcium phosphate (b) sodium chlorate (g) aluminum sulphate (c) potassium chromate (h) cadmium carbonate (d) calcium cyanide (i) silver nitrite (e) potassium hydroxide (j) ammonium hydrogen carbonate © 2008 McGraw-Hill Ryerson Limited Section 4.2 Names and Formulas of Compounds • MHR 69 0056_080_BCSci10_U2CH04_098461.in6956_080_BCSci10_U2CH04_098461.in69 6699 PDF Pass77/11/08/11/08 55:25:39:25:39 PPMM Name Date Comprehension Section 4.2 Use with textbook pages 186–196. -
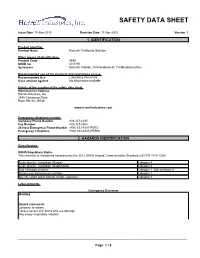
Bismuth Chloride Solution SDS US
SAFETY DATA SHEET Issue Date 10-Nov-2015 Revision Date 11-Nov-2015 Version 1 1. IDENTIFICATION Product identifier Product Name Bismuth Trichloride Solution Other means of identification Product Code 0650 UN/ID no. UN1760 Synonyms Bismuth chloride; Trichlorobismuth, Trichlorobismuthine Recommended use of the chemical and restrictions on use Recommended Use Laboratory chemicals. Uses advised against No information available Details of the supplier of the safety data sheet Manufacturer Address Harrell Industries, Inc. 2495 Commerce Drive Rock Hill, SC 29730 www.harrellindustries.com Emergency telephone number Company Phone Number 803-327-6335 Fax Number 803-327-7808 24 Hour Emergency Phone Number (800) 633-8253 PERS Emergency Telephone (800) 633-8253 (PERS) 2. HAZARDS IDENTIFICATION Classification OSHA Regulatory Status This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute toxicity - Inhalation (Gases) Category 4 Acute toxicity - Inhalation (Dusts/Mists) Category 4 Skin corrosion/irritation Category 1 Sub-category A Serious eye damage/eye irritation Category 1 Specific target organ toxicity (single exposure) Category 3 Label elements Emergency Overview Warning Hazard statements Corrosive to metals. Causes severe skin burns and eye damage May cause respiratory irritation _____________________________________________________________________________________________ Page 1 / 8 0650 - Bismuth Trichloride Solution Revision Date 11-Nov-2015 _____________________________________________________________________________________________ Appearance Clear, colorless to yellow Physical state liquid Odor Faint hydrochloric acid odor. liquid Precautionary Statements - Prevention Wash skin thoroughly after handling Wear eye protection/ face protection Wear protective gloves Precautionary Statements - Response Immediately call a POISON CENTER or doctor IF ON SKIN: Wash with plenty of soap and water IF IN EYES: Rinse cautiously with water for several minutes. -

Safety Data Sheet
Safety data sheet Page: 1/13 BASF Safety data sheet according to UN GHS 4th rev. Date / Revised: 23.10.2017 Version: 2.0 Product: Pearl-Glo® SF PG1099 (ID no. 30322522/SDS_COS_00/EN) Date of print 24.10.2017 1. Identification Product identifier Pearl-Glo® SF PG1099 Chemical name: Pearl-Glo SF CAS Number: 7787-59-9 Relevant identified uses of the substance or mixture and uses advised against Relevant identified uses: cosmetic ingredient Details of the supplier of the safety data sheet Company: BASF SE 67056 Ludwigshafen GERMANY Telephone: +49 621 60-48799 E-mail address: [email protected] Emergency telephone number International emergency number: Telephone: +49 180 2273-112 2. Hazards Identification Classification of the substance or mixture According to UN GHS criteria No need for classification according to GHS criteria for this product. Page: 2/13 BASF Safety data sheet according to UN GHS 4th rev. Date / Revised: 23.10.2017 Version: 2.0 Product: Pearl-Glo® SF PG1099 (ID no. 30322522/SDS_COS_00/EN) Date of print 24.10.2017 Label elements Globally Harmonized System (GHS) The product does not require a hazard warning label in accordance with GHS criteria. Other hazards According to UN GHS criteria No specific dangers known, if the regulations/notes for storage and handling are considered. 3. Composition/Information on Ingredients Substances Chemical nature INCI Name: BISMUTH OXYCHLORIDE Contains: Bismuth chloride oxide CAS Number: 7787-59-9 EC-Number: 232-122-7 Hazardous ingredients (GHS) According to UN GHS criteria No particular hazards known. Mixtures Not applicable 4. First-Aid Measures Description of first aid measures Remove contaminated clothing.