Carrollton 2017 BEST
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Still the Leading Antidepressant After 40
BRITISH JOURNAL OF PSYCHIATRY "2001), 178, 129^144 REVIEW ARTICLE Amitriptyline vv.therest:stilltheleading METHOD Inclusion criteria antidepressant after 40 years of randomised All RCTs comparing amitriptyline with any y other tricyclic,heterocyclic or SSRI were in- controlled trials cluded. Crossover studies were excluded. Studies adopting any criteria to define CORRADO BARBUI and MATTHEW HOTOPF patients suffering from depression were included; a concurrent diagnosis of another psychiatric disorder was not considered an exclusion criterion. Trials in patients with depression with a concomitant medical ill- Background Tricyclic antidepressants Amitriptyline is one of the first `reference' ness were not included in this review. have similar efficacy and slightly lower tricyclic antidepressants TCAs). Over the past 40 years a number of newer tricyclics, tolerability than selective serotonin Search strategy heterocyclics and selective serotonin re- Relevant studies were located by searching reuptakeinhibitorsreuptake inhibitors SSRIs).However, uptake inhibitors SSRIs) have been intro- the Cochrane Collaboration Depression, there are no systematic reviews assessing duced Garattini et aletal,1998). Despite Anxiety and Neurosis Controlled Trials several large systematic reviews comparing amitriptyline, the reference tricyclic drug, Register CCDANCTR). This specialised tricyclics and SSRIs there is no clear agree- vv. other tricyclics and SSRIs directly. register is regularly updated by electronic ment over first-line treatment of depression Medline,Embase,PsycINFO,LILACS, SongSong et aletal,1993; Anderson & Tomenson, Aims ToreviewTo review the tolerability and Psyndex,CINAHL,SIGLE) and non-electro- 1995; Montgomery & Kasper,1995; efficacy of amitriptyline inthe nicnicliterature searches. The register was HotopfHotopf et aletal,1996; Canadian Coordinating management of depression. searched using the following terms: Office for Health Technology Assessment, AMITRIPTYLIN**AMITRIPTYLIN oror AMITRILAMITRIL oror ELA-ELA- 19971997aa). -

Strategies for Managing Sexual Dysfunction Induced by Antidepressant Medication
King’s Research Portal DOI: 10.1002/14651858.CD003382.pub3 Document Version Publisher's PDF, also known as Version of record Link to publication record in King's Research Portal Citation for published version (APA): Taylor, M. J., Rudkin, L., Bullemor-Day, P., Lubin, J., Chukwujekwu, C., & Hawton, K. (2013). Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database of Systematic Reviews, (5). https://doi.org/10.1002/14651858.CD003382.pub3 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

(12) Patent Application Publication (10) Pub. No.: US 2005/0065218A1 Migeon Et Al
US 2005.0065218A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0065218A1 Migeon et al. (43) Pub. Date: Mar. 24, 2005 (54) UTILIZATION OF ALVERINE, ALONE OR IN (30) Foreign Application Priority Data COMBINATION WITH TRICYCLC ANTDEPRESSANT OR A SPECIFIC Jun. 13, 2003 (FR).............................................. O307176 SEROTONIN REUPTAKE INHIBITOR FOR Apr. 30, 2004 (FR).............................................. O404639 THE TREATMENT OF DEPRESSION Publication Classification (76) Inventors: Jacques Migeon, Seattle, WA (US); Frederic Revah, Paris (FR) (51) Int. C.7 - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - A61K 31/137 (52) U.S. Cl. .............................................................. 514/649 Correspondence Address: SESD LARDNER (57) ABSTRACT 3000 KSTREET NW WASHINGTON, DC 20007 (US) The present invention relates to the utilization of Alverine or its metabolites, alone or in combination with a tricyclic (21) Appl. No.: 10/866,079 antidepressant or a Specific Serotonin reuptake inhibitor, for the preparation of pharmaceutical compositions for the (22) Filed: Jun. 14, 2004 treatment of depression. 80 120 OO 8 O 6 O 40 20 t Excipicnts Alverine Alverine Alverine Imiprannine (1% methylcellulose) Citate Citrate Citrate 10 mg/kg 3 mg/kg 10 mg/kg 30 mg/kg Patent Application Publication Mar. 24, 2005 Sheet 1 of 4 US 2005/0065218 A1 Excipients Alverine Alveline Alveline Inipramine (1% methylcellulose) Citrate Citrate Citrate 10 mg/kg 3 mg/kg 10 mg/kg 30 mg/kg Fi gure US 2005/0065218A1 Imipramine 30 mg/kg Figure 2 Patent Application Publication Mar. 24, 2005 Sheet 3 of 4 US 2005/0065218A1 20 Vehicle + Whicule -- Averine Alvérine Vehicule + Alverine Vehicule imipramine 3 ring/kg it 3 mg/kg t- Impramine 10 mg/kg + 3 mg/kg Wellicule imipramine 10 mg/kg Vehicule 3 mg/kg Figure 3 Patent Application Publication Mar. -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/107 (2006.01) A61K 9/00 (2006.01) kind of national protection available): AE, AG, AL, AM, A 61 47/10 (2006.0V) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, PCT/US2012/034361 HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (22) International Filing Date: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 20 April 2012 (20.04.2012) MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/480,259 28 April 201 1 (28.04.201 1) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant (for all designated States except US): BOARD UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, OF REGENTS, THE UNIVERSITY OF TEXAS SYS¬ TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, TEM [US/US]; 201 West 7th St., Austin, TX 78701 (US). -

Patient Assessment?
EMERGENCY MEDICAL TECHNICIAN ‐ BASIC What is Patient Assessment? Why is Patient Assessment important? MECTA EMS Learning Assistant 2 What are the phases of patient assessment? Review of Dispatch Information Scene Survey Initial Assessment Focused History and Physical Exam Detailed Physical Exam Ongoing Assessment Communication Documentation MECTA EMS Learning Assistant 3 Why is the order of Patient Assessment important? Why is it necessary to develop a method of assessment and use that method on all patients? MECTA EMS Learning Assistant 4 SCENE SIZE‐UP INITIAL ASSESSMENT Trauma FOCUSED HISTORY & FOCUSED HISTORY & PHYSICAL EXAM PHYSICAL EXAM Patient Patient DETAILED DETAILED PHYSICAL EXAM PHYSICAL EXAM Medical ON‐GOING ASSESSMENT MECTA EMS Learning Assistant 5 Begin with receipt of call Location Incident Injured/Injuries MECTA EMS Learning Assistant 6 Continue En Route Further info from dispatcher Observe ▪ Smoke? ▪ Fire? ▪ High line wires? ▪ Railroads? ▪ Water? ▪ Industry? ▪ Other Public Safety units? MECTA EMS Learning Assistant 7 Upon Arrival Observe ▪ Overall scene ▪ Location of victim(s) ▪ Possible Mechanisms of Injury MECTA EMS Learning Assistant 8 Upon Arrival Observe ▪ Hazards ▪ Crowds ▪ HazMat ▪ Electricity ▪ Gas ▪ Fire ▪ Glass ▪ Jagged metal ▪ Stability of environment ▪ Traffic ▪ Environment MECTA EMS Learning Assistant 9 Ensure Safety ▪ Yourself ▪ Partner ▪ Other rescuers/Bystanders ▪ Patient MECTA EMS Learning Assistant 10 Call for assistance ▪ Other EMS Units ▪ Law Enforcement ▪ Fire Department ▪ -
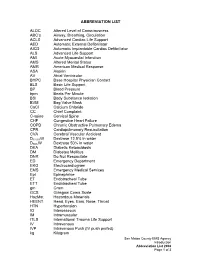
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

2019 Instrumentation and Consumable Catalog 2 INSTRUMENTATION and CONSUMABLE CATALOG
PRODUCT CATALOG 2019 Instrumentation and Consumable Catalog 2 INSTRUMENTATION AND CONSUMABLE CATALOG Resolvex® A200 Part Numbers: A200 96: 253-1160 Resolvex® A200 96 Resolvex A200 Standalone work station for automated sample preparation. The compact benchtop offers the one stop solution for automating sample preparation utilizing creation of multiple work flows, and programmable dispensing of up to 11 solvents. Along with its innovative positive pressure system leading to clean samples, improving accuracy, throughput and enhancing the Life time of your analytical instrument. The A200 comes with an easy to use touch screen interface allowing for easy set up of multiple work flows. In addition the light curtain safety feature will release gas pressure when manifold is activated to prevent any injuries. INSTRUMENTATION AND CONSUMABLE CATALOG 3 Resolvex® A100 Part Numbers: A100 96: 253-0019 A100 48: 253-0014 Resolvex® A100 Standalone work station for automated sample preparation. The compact benchtop offers the one stop solution for automating sample preparation utilizing creation of multiple work flows, and programmable dispensing of up to 11 solvents. Along with its innovative positive pressure system leading to clean samples, improving accuracy, throughput and enhancing the Life time of your analytical instrument. The A100 comes in 96 and 4 configuration allowing for for automated Work Flow solutions in multiple SPE formats. 4 INSTRUMENTATION AND CONSUMABLE CATALOG Resolvex® M10 96/M10 96 XT/M10 48 Part Numbers: M10 96 XT: 288-0006 M10 96: 288-0001 M10 48: 289-0004 Resolvex® M10 Standalone work station for Positive Pressure solid phase extraction. The manual Resolvex M10 48 and 96 are positive pressure manifold for 1, 3, and 6 ml cartridges, or 1ml 96 well plates. -

Career Technical Credit Transfer (CT²) Emergency Medical Technician-Basic (EMT-B) Career Technical Assurance Guide (CTAG) October 17, 2008
Adopted Career Technical Credit Transfer (CT²) Emergency Medical Technician-Basic (EMT-B) Career Technical Assurance Guide (CTAG) October 17, 2008 The following course or Career-Technical Assurance Number (CTAN) is eligible for transfer between career-technical education, adult workforce education, and post-secondary education. CTEMTB002 – Emergency Medical Technician – Basic (EMT-B) Credits: 7 Semester/10 Quarter Hours Advising Notes: Submitted course work must include proof of laboratory and clinical components. Those persons holding current Ohio certification as an EMT-Basic will be given what the receiving institution is offering as credit for its CT² approved EMT-B course. The awarding of credit for the EMT-B course of s t u d y m a y decrease the time to associate degree completion, when such a degree is offered, but will not replace any portion of the EMT-Intermediate or EMT- Paramedic curricula as the later two are separate courses of study. Prerequisite: Current Ohio EMT-Basic Certification Module I Preparatory Module II Patient Assessment Module III Airway and Cardiac Arrest Management Module IV Trauma Patient Management Module V Medical Patient Management Clinical Experience and/or Pre-Hospital Internship Minimum Hours = 120 Didactic 10 Clinical Experience and/or Pre-Hospital Internship Note: Credit hours assigned to CTANs are “relative values,” which are used to help determine the equivalency of submitted coursework or content. Once approved by a validation panel as a CT² course, students will be given what the receiving institution is offering as credit for its CT² approved course. The CTAN illustrates the learning outcomes that are equivalent or common in introductory technical courses. -

Gps' Drug Treatment for Depression by Patients' Educational Level
RESEARCH GPs’ drug treatment for depression by patients’ educational level: registry- based study Anneli Borge Hansen, MD1,2*, Valborg Baste, MSc. Statistics, PhD1, Oystein Hetlevik, MD, PhD1,2, Inger Haukenes, MSc. Philosophy, PhD1,2, Tone Smith- Sivertsen, MD, PhD1,3, Sabine Ruths, MD, PhD1,2 1Research Unit for General Practice, NORCE Norwegian Research Centre, Bergen, Norway; 2Department of Global Public Health and Primary Care, University of Bergen, Bergen, Norway; 3Division of Psychiatry, Haukeland University Hospital, Bergen, Norway Abstract Background: Antidepressant drugs are often prescribed in general practice. Evidence is conflicting on how patient education influences antidepressant treatment. Aim: To investigate the association between educational attainment and drug treatment in adult patients with a new depression diagnosis, and to what extent sex and age influence the association. Design & setting: A nationwide registry- based cohort study was undertaken in Norway from 2014– 2016. Method: The study comprised all residents of Norway born before 1996 and alive in 2015. Information was obtained on all new depression diagnoses in general practice in 2015 (primary care database) and data on all dispensed depression medication (Norwegian Prescription Database [NorPD]) 12 months after the date of diagnosis. Independent variables were education, sex, and age. Associations with drug treatment were estimated using a Cox proportional hazard model and performed separately for sex. *For correspondence: ahan@ Results: Out of 49 967 patients with new depression (61.6% women), 15 678 were dispensed drugs norceresearch. no (30.4% women, 33.0% men). Highly educated women were less likely to receive medication (hazard ratio [HR] = 0.93; 95% confidence interval [CI] = 0.88 to 0.98) than women with low education. -

Still the Leading Antidepressant After 40 Years of Randomised Controlle
BRITISH JOURNAL OF PSYCHIATRY "2001), 178, 129^144 REVIEW ARTICLE Amitriptyline vv.therest:stilltheleading METHOD Inclusion criteria antidepressant after 40 years of randomised All RCTs comparing amitriptyline with any y other tricyclic,heterocyclic or SSRI were in- controlled trials cluded. Crossover studies were excluded. Studies adopting any criteria to define CORRADO BARBUI and MATTHEW HOTOPF patients suffering from depression were included; a concurrent diagnosis of another psychiatric disorder was not considered an exclusion criterion. Trials in patients with depression with a concomitant medical ill- Background Tricyclic antidepressants Amitriptyline is one of the first `reference' ness were not included in this review. have similar efficacy and slightly lower tricyclic antidepressants TCAs). Over the past 40 years a number of newer tricyclics, tolerability than selective serotonin Search strategy heterocyclics and selective serotonin re- Relevant studies were located by searching reuptakeinhibitorsreuptake inhibitors SSRIs).However, uptake inhibitors SSRIs) have been intro- the Cochrane Collaboration Depression, there are no systematic reviews assessing duced Garattini et aletal,1998). Despite Anxiety and Neurosis Controlled Trials several large systematic reviews comparing amitriptyline, the reference tricyclic drug, Register CCDANCTR). This specialised tricyclics and SSRIs there is no clear agree- vv. other tricyclics and SSRIs directly. register is regularly updated by electronic ment over first-line treatment of depression Medline,Embase,PsycINFO,LILACS, SongSong et aletal,1993; Anderson & Tomenson, Aims ToreviewTo review the tolerability and Psyndex,CINAHL,SIGLE) and non-electro- 1995; Montgomery & Kasper,1995; efficacy of amitriptyline inthe nicnicliterature searches. The register was HotopfHotopf et aletal,1996; Canadian Coordinating management of depression. searched using the following terms: Office for Health Technology Assessment, AMITRIPTYLIN**AMITRIPTYLIN oror AMITRILAMITRIL oror ELA-ELA- 19971997aa). -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.