TRPV1 Channels Contribute to Behavioral Hypersensitivity and Spontaneous Activity in Nociceptors After Spinal Cord Injury Zizhen Wu
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Targeting the Endocannabinoid System to Reduce Nociception
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2011 Targeting the endocannabinoid system to reduce nociception Lamont Booker Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2419 This Dissertation is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. Targeting the Endocannabinoid System to Reduce Nociception A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at Virginia Commonwealth University. By Lamont Booker Bachelor’s of Science, Fayetteville State University 2003 Master’s of Toxicology, North Carolina State University 2005 Director: Dr. Aron H. Lichtman, Professor, Pharmacology & Toxicology Virginia Commonwealth University Richmond, Virginia April 2011 Acknowledgements The author wishes to thank several people. I like to thank my advisor Dr. Aron Lichtman for taking a chance and allowing me to work under his guidance. He has been a great influence not only with project and research direction, but as an excellent example of what a mentor should be (always willing to listen, understanding the needs of each student/technician, and willing to provide a hand when available). Additionally, I like to thank all of my committee members (Drs. Galya Abdrakmanova, Francine Cabral, Sandra Welch, Mike Grotewiel) for your patience and willingness to participate as a member. Our term together has truly been memorable! I owe a special thanks to Sheryol Cox, and Dr. -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -

Transient Receptor Potential Channels As Drug Targets: from the Science of Basic Research to the Art of Medicine
1521-0081/66/3/676–814$25.00 http://dx.doi.org/10.1124/pr.113.008268 PHARMACOLOGICAL REVIEWS Pharmacol Rev 66:676–814, July 2014 Copyright © 2014 by The American Society for Pharmacology and Experimental Therapeutics ASSOCIATE EDITOR: DAVID R. SIBLEY Transient Receptor Potential Channels as Drug Targets: From the Science of Basic Research to the Art of Medicine Bernd Nilius and Arpad Szallasi KU Leuven, Department of Cellular and Molecular Medicine, Laboratory of Ion Channel Research, Campus Gasthuisberg, Leuven, Belgium (B.N.); and Department of Pathology, Monmouth Medical Center, Long Branch, New Jersey (A.S.) Abstract. ....................................................................................679 I. Transient Receptor Potential Channels: A Brief Introduction . ...............................679 A. Canonical Transient Receptor Potential Subfamily . .....................................682 B. Vanilloid Transient Receptor Potential Subfamily . .....................................686 C. Melastatin Transient Receptor Potential Subfamily . .....................................696 Downloaded from D. Ankyrin Transient Receptor Potential Subfamily .........................................700 E. Mucolipin Transient Receptor Potential Subfamily . .....................................702 F. Polycystic Transient Receptor Potential Subfamily . .....................................703 II. Transient Receptor Potential Channels: Hereditary Diseases (Transient Receptor Potential Channelopathies). ......................................................704 -

Pharmacology and Antitussive Efficacy of 4-(3-Trifluoromethyl-Pyridin
JPET Fast Forward. Published on August 9, 2007 as DOI: 10.1124/jpet.107.127258 JPET FastThis article Forward. has not beenPublished copyedited on and Augustformatted. 9,The 2007 final version as DOI:10.1124/jpet.107.127258 may differ from this version. JPET # 127258 Pharmacology and antitussive efficacy of 4-(3-trifluoromethyl-pyridin- 2-yl)-piperazine-1-carboxylic acid (5-trifluoromethyl-pyridin-2-yl)- amide (JNJ17203212), a TRPV1 antagonist in guinea pigs Downloaded from Anindya Bhattacharya, Brian P. Scott, Nadia Nasser, Hong Ao, Michael P. Maher, Adrienne E. Dubin, Devin M. Swanson, Nigel P. Shankley, Alan D. Wickenden, Sandra jpet.aspetjournals.org R. Chaplan Department of Pain and Related Disorders (A.B., B.P.S., N.N., H.A., M.P.M., A.E.D., A.D.W., S.R.C.), Neuroscience (D.M.S.) and Physiological Systems (N.P.S.) Johnson and Johnson Pharmaceutical Research & Development LLC. at ASPET Journals on September 26, 2021 3210 Merryfield Row, San Diego, CA 92121 1 Copyright 2007 by the American Society for Pharmacology and Experimental Therapeutics. JPET Fast Forward. Published on August 9, 2007 as DOI: 10.1124/jpet.107.127258 This article has not been copyedited and formatted. The final version may differ from this version. JPET # 127258 Running title: TRPV1 antagonism and cough Corresponding author: Anindya Bhattacharya, Ph.D. Johnson and Johnson Pharmaceutical Research & Development 3210 Merryfield Row Downloaded from San Diego, CA 92121 [email protected] Phone: (858) 320-3429 Fax: (858) 450-2040 jpet.aspetjournals.org Number of -

Cannabinoids Using ALZET Osmotic Pumps
ALZET® Bibliography References on the Administration of Cannabinoids Using ALZET Osmotic Pumps Q5966: P. Weydt. Mechanisms and Modifiers of Energy Metabolism in ALS and Huntington Disease. Open Access Repositorium der Universität Ulm 2016; ALZET Comments: Cannabinol; PEG 400; SC; Mice; 2004; 4 weeks; animal info (SOD 1 transgenic); pumps replaced every 28 days; Therapeutic indication (amyotrophic lateral sclerosis); Dose (5 mg/kg);. Q3610: E. J. Rahn, et al. Prophylactic cannabinoid administration blocks the development of paclitaxel-induced neuropathic nociception during analgesic treatment and following cessation of drug delivery. Molecular Pain 2014;10(U1-U19 ALZET Comments: AM1710; Taxol-WIN-55212-2; AM251; AM630; DMSO; PEG 400; SC; Rat; 2ML4; 28 days; Controls received mp w/ saline; animal info (male, Sprague Dawley, 300-400g); functionality of mp verified by residual volume; 50% PEG 400 used; 50% DMSO used; Multiple pumps per animal (2); stress/adverse reaction: (see pg.15); behavioral testing (mechanical threshold, cold withdrawal, locomotor activity); AM1710 is a cannabilactone CB2-selective agonist; pumps removed on day 22; WIN55,212-2 is a CB1/CB2 agonist;. Q4814: Heloísa Helena Vilela Costa, et al. Continuous central infusion of cannabinoid receptor agonist WIN 55,212-2 decreases maternal care in lactating rats: Consequences for fear conditioning in adulthood males. Behav. Brain Res 2013;257(31-38 ALZET Comments: WIN-55212-2; NaCl; tween, DMSO; CSF/CNS; Rat; 1007D; 7 days; Controls received mp w/ vehicle; animal info (female, Wistar, 9 weeks old); 10% DMSO used; dose-response (pg 34); behavioral testing (fear conditioning, maternal behavior); teratology; “The continuous infusion of WIN in the CNS using an osmotic minipump in lactating dams eliminates the possibility that WIN affects the behavior of the offspring when offered in the milk. -

Antitussive Activity of Iodo-Resiniferatoxin in Guinea Pigs M Trevisani, a Milan, R Gatti, a Zanasi, S Harrison, G Fontana, a H Morice, P Geppetti
769 COUGH Thorax: first published as 10.1136/thx.2003.012930 on 27 August 2004. Downloaded from Antitussive activity of iodo-resiniferatoxin in guinea pigs M Trevisani, A Milan, R Gatti, A Zanasi, S Harrison, G Fontana, A H Morice, P Geppetti ............................................................................................................................... Thorax 2004;59:769–772. doi: 10.1136/thx.2003.012930 See end of article for authors’ affiliations ....................... Background: Iodo-resiniferatoxin (I-RTX) has recently been described as an ultra potent antagonist of the Correspondence to: transient receptor potential vanilloid-1 (TRPV1). M Trevisani, PhD, Methods: The ability of I-RTX to inhibit cough induced by inhalation of two putative TRPV1 stimulants Center of Excellence for the Study of Inflammation, (capsaicin and citric acid) was tested in non-anaesthetised guinea pigs. University of Ferrara, Results: Pretreatment with I-RTX either intraperitoneally (0.03–0.3 mmol/kg) or by aerosol (0.1–3 mM) 44100 Ferrara, Italy; reduced the number of coughs produced by inhalation of citric acid (0.25 M) and capsaicin (30 mM) in a [email protected] dose dependent manner. Capsazepine (CPZ) also reduced citric acid and capsaicin induced cough, but Received 17 July 2003 the activity of I-RTX was 10–100 times more potent than CPZ in all the experimental conditions tested. Accepted 10 March 2004 Conclusions: I-RTX is a novel and potent antitussive drug which inhibits cough mediated by agents possibly ....................... acting via TRPV1 activation. ough is one of the most common reasons for medical I-RTX behaves as an ultra potent antagonist at the native rat consultation. In most cases, however, drugs currently and guinea pig TRPV1 and at the recombinant human Cavailable for antitussive treatment are only partially TRPV1.20 effective. -

Calcium Entry Through TRPV1: a Potential Target for the Regulation of Proliferation and Apoptosis in Cancerous and Healthy Cells
International Journal of Molecular Sciences Review Calcium Entry through TRPV1: A Potential Target for the Regulation of Proliferation and Apoptosis in Cancerous and Healthy Cells Kevin Zhai 1 , Alena Liskova 2, Peter Kubatka 3 and Dietrich Büsselberg 1,* 1 Department of Physiology and Biophysics, Weill Cornell Medicine-Qatar, Education City, Qatar Foundation, Doha, PO Box 24144, Qatar; [email protected] 2 Clinic of Obstetrics and Gynecology, Jessenius Faculty of Medicine, Comenius University in Bratislava, 03601 Martin, Slovakia; [email protected] 3 Department of Medical Biology, Jessenius Faculty of Medicine, Comenius University in Bratislava, 03601 Martin, Slovakia; [email protected] * Correspondence: [email protected]; Tel.: +974-4492-8334 Received: 14 May 2020; Accepted: 8 June 2020; Published: 11 June 2020 2+ 2+ Abstract: Intracellular calcium (Ca ) concentration ([Ca ]i) is a key determinant of cell fate and is implicated in carcinogenesis. Membrane ion channels are structures through which ions enter or exit the cell, depending on the driving forces. The opening of transient receptor potential vanilloid 1 (TRPV1) ligand-gated ion channels facilitates transmembrane Ca2+ and Na+ entry, which modifies the delicate balance between apoptotic and proliferative signaling pathways. Proliferation is upregulated through two mechanisms: (1) ATP binding to the G-protein-coupled receptor P2Y2, commencing a kinase signaling cascade that activates the serine-threonine kinase Akt, and (2) the transactivation of the epidermal growth factor receptor (EGFR), leading to a series of protein signals that activate the extracellular signal-regulated kinases (ERK) 1/2. The TRPV1-apoptosis pathway involves Ca2+ influx and efflux between the cytosol, mitochondria, and endoplasmic reticulum (ER), the release of apoptosis-inducing factor (AIF) and cytochrome c from the mitochondria, caspase activation, and DNA fragmentation and condensation. -

5-Iodoresiniferatoxin Evokes Hypothermia in Mice and Is a Partial TRPV1 Agonist in Vitro
JPET Fast Forward. Published on June 9, 2005 as DOI: 10.1124/jpet.105.084277 JPETThis Fast article Forward. has not been Published copyedited and on formatted. June 9, The 2005 final asversion DOI:10.1124/jpet.105.084277 may differ from this version. JPET #84277 TITLE: 5-Iodoresiniferatoxin evokes hypothermia in mice and is a partial TRPV1 agonist in vitro Isao Shimizu1, Tohko Iida1, Nobuhiko Horiuchi, and Michael J. Caterina Downloaded from Departments of Biological Chemistry and Neuroscience Johns Hopkins School of Medicine, Baltimore, MD 21205 USA (I.S., T.I., and M.J.C.) jpet.aspetjournals.org and Dainippon Pharmaceutical Company, Limited, Suita/Osaka 564-0053 Japan (I.S. and N.H.) at ASPET Journals on September 27, 2021 1 Copyright 2005 by the American Society for Pharmacology and Experimental Therapeutics. JPET Fast Forward. Published on June 9, 2005 as DOI: 10.1124/jpet.105.084277 This article has not been copyedited and formatted. The final version may differ from this version. JPET #84277 RUNNING TITLE: IRTX activates TRPV1 in vivo and in vitro Address correspondence to: Michael J. Caterina, M.D., Ph.D., Associate Professor, Department of Biological Chemistry, Johns Hopkins School of Medicine, 725 North Wolfe Street, Baltimore, MD 21205 email: [email protected]. Downloaded from Phone: (410) 502-5457 FAX: (410) 955-5759 jpet.aspetjournals.org Number of text pages: 31 (including title pages and figure legends) Number of tables: 0 at ASPET Journals on September 27, 2021 Number of figures: 4 Number of References: 33 Words in Abstract: 149 Words in Introduction: 607 Words in Discussion: 1289 Nonstandard Abbreviations: TRPV1, transient receptor potential vanilloid 1; I-RTX, 5-iodoresiniferatoxin, (6,7-deepoxy-6,7-didehydro-5-deoxy-21-dephenyl-21-(phenylmethyl)-daphnetoxin,20-(4-h ydroxy-5-iodo-3-ethoxybenzeneacetate,; RTX, resiniferatoxin, 6,7-deepoxy-6,7-didehydro-5-deoxy-21-dephenyl-21-(phenylmethyl)-daphnetoxin,20-(4-hy 2 JPET Fast Forward. -

Brain Research Bulletin Sensitization of Voltage Activated Calcium Channel Currents for Capsaicin in Nociceptive Neurons by Tumo
Brain Research Bulletin 81 (2010) 157–163 Contents lists available at ScienceDirect Brain Research Bulletin journal homepage: www.elsevier.com/locate/brainresbull Research report Sensitization of voltage activated calcium channel currents for capsaicin in nociceptive neurons by tumor-necrosis-factor-␣ T. Hagenacker a,b,∗, J.C. Czeschik b, M. Schäfers a, D. Büsselberg b,c a Universitätsklinikum Essen, Klinik für Neurologie, Hufelandstr. 55, 45122 Essen, Germany b Universitätsklinikum Essen, Institut für Physiologie, Hufelandstr. 55, 45122 Essen, Germany c Texas Tech University, Health Science Center, Paul L. Foster School of Medicine, 5001 El Paso Drive, El Paso, TX 79905, USA article info abstract Article history: It is known that application of tumor-necrosis-factor-␣ (TNF-␣) sensitizes neuronal calcium channels Received 9 July 2009 for heat stimuli in rat models of neuropathic pain. This study examines whether TNF-␣ modulates the Received in revised form capsaicin-induced effects after transient receptor potential vanilloid (TRPV)-1 receptor activation on 16 September 2009 voltage activated calcium channel currents (I ). Accepted 27 September 2009 Ca(V) TRPV-1 receptors are activated by heat and play an important role in the pathogenesis of thermal hyper- Available online 7 October 2009 algesia in neuropathic pain syndromes, while voltage activated channels are essential for transmission of neuronal signals. Keywords: Voltage activated calcium channels Eliciting ICa(V) in DRG neurons of rats by a depolarization from the resting potential to 0 mV, TNF- ␣ ± ± Tumor-necrosis-factor-␣ (100 ng/ml) reduces ICa(V) by 16.9 2.2%, while capsaicin (0.1 M) decreases currents by 27 4.3%. Capsaicin Pre-application of TNF-␣ (100 ng/ml) for 24 h results in a sensitization of ICa(V) to capsaicin (0.1 M) Neuropathic pain with a reduction of 42.8 ± 4.4% mediated by TRPV-1. -
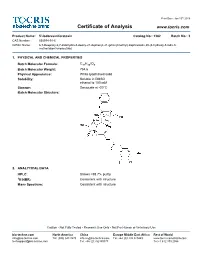
Certificate of Analysis
Print Date: Jan 13th 2016 Certificate of Analysis www.tocris.com Product Name: 5'-Iodoresiniferatoxin Catalog No.: 1362 Batch No.: 3 CAS Number: 535974-91-5 IUPAC Name: 6,7-Deepoxy-6,7-didehydro-5-deoxy-21-dephenyl-21-(phenylmethyl)-daphnetoxin,20-(4-hydroxy-5-iodo-3- methoxybenzeneacetate) 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C37H39IO9 Batch Molecular Weight: 754.6 Physical Appearance: White lyophilised solid Solubility: Soluble in DMSO ethanol to 100 mM Storage: Desiccate at -20°C Batch Molecular Structure: 2. ANALYTICAL DATA HPLC: Shows >98.7% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 13th 2016 Product Information www.tocris.com Product Name: 5'-Iodoresiniferatoxin Catalog No.: 1362 Batch No.: 3 CAS Number: 535974-91-5 IUPAC Name: 6,7-Deepoxy-6,7-didehydro-5-deoxy-21-dephenyl-21-(phenylmethyl)-daphnetoxin,20-(4-hydroxy-5-iodo-3- methoxybenzeneacetate) Description: Storage: Desiccate at -20°C Potent and silent vanilloid receptor antagonist, 40-fold more CAUTION - This product is light sensitive and we recommend potent than capsazepine (Cat. No. 0464). Binds to TRPV1 (VR1) that the solid material and any solutions obtained are protected receptors expressed in HEK293 cells with a Ki of 5.8 nM. -

TRPV1: Role in Skin and Skin Diseases and Potential Target for Improving Wound Healing
International Journal of Molecular Sciences Review TRPV1: Role in Skin and Skin Diseases and Potential Target for Improving Wound Healing Michelle D. Bagood 1 and R. Rivkah Isseroff 1,2,* 1 Department of Dermatology, School of Medicine, UC Davis, Sacramento, CA 95816, USA; [email protected] 2 Dermatology Section, VA Northern California Health Care System, Mather, CA 95655, USA * Correspondence: [email protected]; Tel.: +1-(916)-551-2606 Abstract: Skin is innervated by a multitude of sensory nerves that are important to the function of this barrier tissue in homeostasis and injury. The role of innervation and neuromediators has been previously reviewed so here we focus on the role of the transient receptor potential cation channel, subfamily V member 1 (TRPV1) in wound healing, with the intent of targeting it in treatment of non-healing wounds. TRPV1 structure and function as well as the outcomes of TRPV1-targeted therapies utilized in several diseases and tissues are summarized. In skin, keratinocytes, sebocytes, nociceptors, and several immune cells express TRPV1, making it an attractive focus area for treating wounds. Many intrinsic and extrinsic factors confound the function and targeting of TRPV1 and may lead to adverse or off-target effects. Therefore, a better understanding of what is known about the role of TRPV1 in skin and wound healing will inform future therapies to treat impaired and chronic wounds to improve healing. Keywords: TRPV1; wound healing; skin; keratinocytes; pilosebaceous unit; nociceptors Citation: Bagood, M.D.; Isseroff, R.R. TRPV1: Role in Skin and Skin Diseases and Potential Target for 1. Introduction Improving Wound Healing. -

Blocking the Transient Receptor Potential Vanilloid-1 Does Not
Blocking the transient receptor potential vanilloid-1 does not reduce the exercise pressor reflex in healthy rats Guillaume Ducrocq, Juan Estrada, Joyce Kim, Marc Kaufman To cite this version: Guillaume Ducrocq, Juan Estrada, Joyce Kim, Marc Kaufman. Blocking the transient receptor po- tential vanilloid-1 does not reduce the exercise pressor reflex in healthy rats. AJP - Regulatory, Integrative and Comparative Physiology, American Physiological Society, 2019, 317 (4), pp.576 - 587. 10.1152/ajpregu.00174.2019. hal-02969591 HAL Id: hal-02969591 https://hal.archives-ouvertes.fr/hal-02969591 Submitted on 16 Oct 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Am J Physiol Regul Integr Comp Physiol 317: R576–R587, 2019. First published July 31, 2019; doi:10.1152/ajpregu.00174.2019. RESEARCH ARTICLE Neural Control Blocking the transient receptor potential vanilloid-1 does not reduce the exercise pressor reflex in healthy rats X Guillaume P. Ducrocq, Juan A. Estrada, X Joyce S. Kim, and Marc P. Kaufman Heart and Vascular Institute, Pennsylvania State University College of Medicine, Hershey, Pennsylvania Submitted 12 June 2019; accepted in final form 26 July 2019 Ducrocq GP, Estrada JA, Kim JS, Kaufman MP.