Dengue Epidemic 2017: Evidence and Lessons Learnt — Part 3 This Article, Discussed Here As the Third Deaths in 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tender ID Link to Download Information Copy of Addendum 1
Distribution Division 02 Link to download Area Tender ID information copy of Addendum 1 DGM (East)/Area(Trincomalee)/ CSC(Trinco Town)/001/ ETD 154 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/002/ ETB 080 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/003/ ETB 024 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/004/ ETB 025 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/005/ ETB 045 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/006/ ETB 009 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/007/ ETB 062 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/008/ ETB 023 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/009/ ETB 079 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/010/ ETB 002 Click Here Trincomalee DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/011/ ETB 068 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/012/ ETB 003 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kanthale)/013/ ETB 047 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/014/ ETE 055 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/015/ ETE 013 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/016/ ETE 032 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/017/ ETE 009 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/018/ ETE 037 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/019/ ETE 030 Click Here DGM (East)/Area(Trincomalee)/ CSC(Kinniya)/020/ ETE 036 Click Here Link to download Area Tender ID information copy of Addendum 1 DGM (East)/Area(Batticaloa)/CSC(Vaharai)/001/ -

(Lates Calcarifer) in Net Cages in Negombo Lagoon, Sri Lanka: Culture Practices, Fish Production and Profitability
Journal of Aquatic Science and Marine Biology Volume 1, Issue 2, 2018, PP 20-26 Farming of Seabass (Lates calcarifer) in net cages in Negombo Lagoon, Sri Lanka: Culture practices, fish production and profitability H.S.W.A. Liyanage and K.B.C.Pushpalatha National Aquaculture Development Authority of Sri Lanka, 41/1, New Parliament Road, Pelawatta, Battaramulla, Sri Lanka *Corresponding Author: K.B.C.Pushpalatha, National Aquaculture Development Authority of Sri Lanka, 41/1, New Parliament Road, Pelawatta, Battaramulla, Sri Lanka. ABSTRACT Shrimp farming is the main coastal aquaculture activity and sea bass cage farming also recently started in Sri Lanka. Information pertaining to culture practices, fish production, financial returns and costs involved in respect of seabass cage farms operate in the Negombo lagoon were collected through administering a questionnaire. The survey covered 13 farms of varying sizes. The number of cages operated by an individual farmer or a family ranged from 2 – 13. Almost all the farmers in the lagoon used floating net cages, except for very few farmers, who use stationary cages. Net cages used by all the farmers found to be of uniform in size (3m x 3m x 2m) and stocking densities adapted in cages are also similar. Production of fish ranged between 300 to 400 Kg per grow-out cage. All seabass farmers in the Negombo lagoon entirely depend on fish waste/trash fish available in the Negombo fish market to feed the fish. Availability of these fish waste/trash fish at no cost to the farmers has made small scale seabass farming financially very attractive. -

Epidemiological Bulletin Sri Lanka
Veterinary Epidemiological Bulletin Sri Lanka Volume 6 No 01 ISSN:1800-4881 January - March 2013 Department of Animal Production and Health, P.O.Box 13, Peradeniya, Sri Lanka. [email protected] Contents Control of Infectious Bursal 1 Control of Infectious Bursal Disease Disease (Gumboro) (Gumboro) 1.1 Introduction 1.1 Introduction 1.2 Epidemiology 1.3 Clinical Signs Infectious Bursal Disease (IBD) is a highly contagious viral infection of young chicken. The disease was first recognized 1.4 Diagnosis in Gumboro, Delaware, USA in 1962. The disease is very 1.5 Control and Prevention important to the poultry industry worldwide since the virus 2 Status of Livestock Diseases cause immunosuppression in birds leading to increased susceptibility to other diseases and negative interference 2.1 Bovine Disease with effective vaccination. Very virulent strains of IBD virus 2.1.1 Bovine Babesiosis has been spreading in Europe, Latin America, South-East 2.1.2 Bovine Brucellosis Asia, Africa and Middle East countries in recent years. 2.1.3 Foot and Mouth Disease 1.2 Epidemiology 2.1.4 Mastitis 2.2 Caprine Diseases Gumboro disease is caused by a virus of the genus Avibimavirus of the family Birnaviridae. The disease is 2.2.1 Contagious Pustular Dermatitis characterized by destruction of lymphocytes in the bursa (CPD) of fabricius and to lesser extent in other lymphoid organs. 2.3 Rabies The chicks around 3-6 weeks old show severe acute disease 2.4 Poultry Diseases with high mortality. Occurrence in younger birds is usually asymptomatic but cause permanent and severe damage 2.4.1 Fowl pox to bursa of fabricius. -
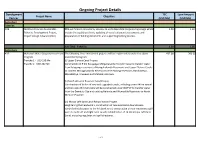
Ongoing Project Details
Ongoing Project Details Development TEC Loan Amount Project Name Objective Partner (USD Mn) (USD Mn) Agriculture Fisheries ADB Northern Province Sustainable PDA will finance consultancy services to undertake detail engineering design which 1.59 1.30 Fisheries Development Project, include the updating of cost, updating of social safeguard assessments and Project Design Advance (PDA) preparation of bidding documents and supporting bidding process. Sub Total - Fisheries 1.59 1.30 Agriculture ADB Mahaweli Water Security Investment The following three investment projects will be implemented under the above 432.00 360.00 Program investment program. Tranche 1 - USD 190 Mn (i) Upper Elahera Canal Project Tranche 2- USD 242 Mn Construction of 9 km Kaluganga-Morgahakanda Transfer Canal to transfer water from Kaluganga reservoir to Moragahakanda Reservoirs and Upper Elehera Canals to connect Moragahakanda Reservoir to the existing reservoirs; Huruluwewa, Manakattiya, Eruwewa and Mahakanadarawa. (ii) North Western Province Canal Project Construction of 96 km of new and upgraded canals, including a new 940 m tunnel and two new 25 m tall dams will be constructed under NWPCP to transfer water from the Dambulu Oya and existing Nalanda and Wemedilla Reservoirs to North Western Province. (iii) Minipe Left Bank Canal Rehabilitation Project Heightening the headwork’s, construction of new automatic downstream- controlled intake gates to the left bank canal; construction of new emergency spill weirs to both left and right bank canals; rehabilitation of 74 km Minipe Left Bank Canal, including regulator and spill structures. 1 of 24 Ongoing Project Details Development TEC Loan Amount Project Name Objective Partner (USD Mn) (USD Mn) IDA Agriculture Sector Modernization Objective is to support increasing Agricultural productivity, improving market 125.00 125.00 Project access and enhancing value addition of small holder farmers and agribusinesses in the project areas. -
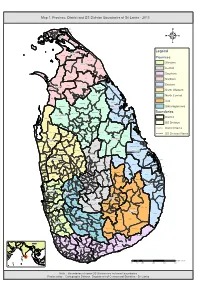
Map 1: Province, District and DS Division Boundaries of Sri Lanka - 2013
Map 1: Province, District and DS Division Boundaries of Sri Lanka - 2013 Vadam aradchi North (P oint Pedro) Valikam am North (Tellipallai) Valikam am S outh- West ( Sandilipay ) Vadam aradchi South-W es t (K araveddy) Valikam am W est (Chankanai) Karainagar Valikam am E ast (K opay) Valikam am S outh ( Uduv il) Jaffna Is land North (K ayts ) Thenm aradchi (Chavak achcheri) Jaffna Nallur Is land S outh (V elanai) Vadam aradchi Eas t Pachc hilaipalli 4 Delft Kandavalai Legend Kilinochchi Poonakary Karac hchi Provinces Puthukk udiyiruppu Mullaitivu Western Thunuk kai Maritim epattu Oddus uddan Central Mannar Town Southern Manthai W es t Manthai E ast Vav uniy a Nor th Welioya Northern Padavi Sr i P ura Madhu Eastern Mannar Vavuniya Padaviya Nanattan Vav uniy a Kuchc haveli North Western Vav uniy a S outh Gom ar ank adawala Kebithigollewa North Central Mus ali Vengalacheddik ulam Uva Morawewa Medawachc hiya Tr inc omalee Town and Gr av ets Mahawilachc hiy a Trincomalee Hor owpothana Sabaragamuwa Tham balagam uwa Ram bewa Kahatagas digiliya Kinniya Muttur Nuwar agam Palatha Central Boundaries Anuradhapura Mihinthale Kanthale Vanathawilluwa Noc hchiyagama District Nuwar agam Palatha E ast Seruv ila Verugal (E achc hilam pattu) Galenbindunuwewa Nac hchaduwa DS Division Thirappane Thalawa Medirigiriya Rajanganay a Colombo Tham buttegam a District Name Karuwalagas wewa Gir ibawa Hingurakgoda Ipalogam a Palugas wewa Kolonnawa Lank apura DS Division Name Welikanda Koralai P attu North (V aharai) Puttalam Galnewa Nawagattegam a Galgam uwa Kekirawa -

SITUATION REPORT # 140 JAFFNA, KILINOCHCHI, MULLAITIVU, MANNAR, VAVUNIYA, TRINCOMALEE, BATTICALOA and AMPARA DISTRICTS 14-21
SITUATION REPORT # 140 JAFFNA, KILINOCHCHI, MULLAITIVU, MANNAR, VAVUNIYA, TRINCOMALEE, BATTICALOA and AMPARA DISTRICTS 14-21 August 2008 IDP situation as reported this week by GAs Displacement after April 2006 Location Number of Families Number of Individuals Jaffna 6,129 20,736 Kilinochchi 35,353 134,868 Mullaitivu 8,917 31,080 Vavuniya 5,199 18,403 Mannar 2,774 8,709 Trincomalee 1571 5254 Batticaloa 4,274 16,213 Ampara 1,162 4,278 JAFFNA DISTRICT Situation update • Minor confrontations between the SLA and LTTE around the FDLs in Muhamalai and Nagarkovil were reported. • Damages to electricity transformers were once again reported in the Kokuvil area in Nallur DS Division. • On August 19, staff from Jaffna University held a silent protest to show solidarity with Vanni civilians and called for an end to the fighting. • The curfew which was relaxed by 30 minutes for the Nallur temple festival remains is still in place from 2100 - 0400 hours Displacement/ Returns • No major movements were observed this week. Sector Developments/Gaps • Security Forces have released 103 acres of paddy land within the High Security Zone for cultivation. The land belongs to 73 civilians, who are reportedly to receive special identity cards to facilitate access to the area. • The civilian population in Jaffna has been facing power and energy issues since June 1990, when the Northern Province was cut off from the main national electrical grid. Since then, the Northern population has been using alternate energy sources for both homes and industries. The energy supply has improved since the 1996 returns when the main supply was through generators in Kankasanthurai, generally providing supply every other day to various areas. -

Y%S ,Xld M%Cd;Dka;%Sl Iudcjd§ Ckrcfha .Eiü M;%H W;S Úfyi the Gazette of the Democratic Socialist Republic of Sri Lanka EXTRAORDINARY
Y%S ,xld m%cd;dka;%sl iudcjd§ ckrcfha .eiÜ m;%h w;s úfYI The Gazette of the Democratic Socialist Republic of Sri Lanka EXTRAORDINARY wxl 2072$58 - 2018 uehs ui 25 jeks isl=rdod - 2018'05'25 No. 2072/58 - FRIDAY, MAY 25, 2018 (Published by Authority) PART I : SECTION (I) — GENERAL Government Notifications SRI LANKA Coastal ZONE AND Coastal RESOURCE MANAGEMENT PLAN - 2018 Prepared under Section 12(1) of the Coast Conservation and Coastal Resource Management Act, No. 57 of 1981 THE Public are hereby informed that the Sri Lanka Coastal Zone and Coastal Resource Management Plan - 2018 was approved by the cabinet of Ministers on 25th April 2018 and the Plan is implemented with effect from the date of Gazette Notification. MAITHRIPALA SIRISENA, Minister of Mahaweli Development and Environment. Ministry of Mahaweli Development and Environment, No. 500, T. B. Jayah Mawatha, Colombo 10, 23rd May, 2018. 1A PG 04054 - 507 (05/2018) This Gazette Extraordinary can be downloaded from www.documents.gov.lk 1A 2A I fldgi ( ^I& fPoh - YS% ,xld m%cd;dka;s%l iudcjd§ ckrcfha w;s úfYI .eiÜ m;%h - 2018'05'25 PART I : SEC. (I) - GAZETTE EXTRAORDINARY OF THE DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA - 25.05.2018 CHAPTER 1 1. INTRODUCTION 1.1 THE SCOPE FOR COASTAL ZONE AND COASTAL RESOURCE MANAGEMENT 1.1.1. Context and Setting With the increase of population and accelerated economic activities in the coastal region, the requirement of integrated management focused on conserving, developing and sustainable utilization of Sri Lanka’s dynamic and resources rich coastal region has long been recognized. -

Humanitarian Operation Factual Analysis July 2006 – May 2009
HUMANITARIAN OPERATION FACTUAL ANALYSIS JULY 2006 – MAY 2009 MINISTRY OF DEFENCE DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA HUMANITARIAN OPERATION FACTUAL ANALYSIS JULY 2006 – MAY 2009 MINISTRY OF DEFENCE JULY 2011 DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA Humanitarian Operation—Factual Analysis TABLE OF CONTENTS Page I. EXECUTIVE SUMMARY 1 A. Overview of this Report 1 B. Overview of the Humanitarian Operation 1 PART ONE II. BACKGROUND 4 A. Overview of the LTTE 4 B. LTTE Atrocities against Civilians 6 C. Use of Child Soldiers by the LTTE 10 D. Ethnic Cleansing Carried out by the LTTE 10 E. Attacks on Democracy by the LTTE 11 F. The Global Threat posed by the LTTE 11 G. Proscription of the LTTE 12 III. SIZE AND SCOPE OF THE LTTE 13 A. Potency of the LTTE 13 B. Number of Cadres 14 C. Land Fighting Forces 14 D. The Sea Tiger Wing 17 E. The Air Tiger Wing 20 F. Black Tiger (Suicide) Wing 22 G. Intelligence Wing 22 H. Supply Network 23 I. International Support Mechanisms 25 J. International Criminal Network 27 – iii – Humanitarian Operation—Factual Analysis Page IV. GOVERNMENT EFFORTS FOR A NEGOTIATED SETTLEMENT 28 A. Overview 28 B. The Thimpu Talks – July to August 1985 29 C. The Indo-Lanka Accord – July 1987 30 D. Peace Talks – May 1989 to June 1990 32 E. Peace Talks – October 1994 to April 1995 33 F. Norwegian-Facilitated Peace Process – February 2002 to January 2008 35 G. LTTE Behaviour during 2002–2006 37 PART TWO V. RESUMPTION OF HOSTILITIES 43 VI. THE WANNI OPERATION 52 VII. -

TRI TRI Displacement Idpsitu
IDP Site Locations DISTRICT: Trincomalee As at 20 May 2009 80°50'0"E 80°55'0"E 81°0'0"E 81°5'0"E 81°10'0"E 81°15'0"E 81°20'0"E 81°25'0"E Displaced since 1983 Displaced after 2006 Tsunami IDPs Vanni IDPs Ds Division In camps In camps With host families Returnees In Camps In camps Families Families Individuals Families Individuals Families Individuals Families Families Individuals 9°0'0"N Mullaitivu Echchilampattai - - - - - 3,063 11,958 - - - Kinniya - - - 38 127 - - - - - Kuchchaveli 3 - - 26 95 - - - 2,130 7,167 Muttur - 647 2,070 - - 2,507 8,028 126 - - Seruvila - - - - - 136 512 - - Sinhala Mahavidyalaya Emergency shelter sites Thampalakamam - - - 17 43 - - - - - t[ Town & Gravets - - - 393 1,434 - - - - - ! Padavisripura .[ Pulmoddai 8°55'0"N Sahanagama Emergency shelter sites ! Thiriyai ! Eramadu Kaddukulam ! 8°50'0"N Kuchaveli ! Kuchaveli Gomarankadawela Kivulekada Kumpurupiddi East ! ! ! Adampanai 8°45'0"N Pangurugaswewa Kumpurupiddi ! ! ! Madawachchi Pettewa ! ! Valaiyoothu Tirappanai ! ! Kumpurupiddi South t[ Jaganathan Place IDP site Gopalapuram ! Nilaveli Gomarankadawala ! ! Veloor Mediyawa Nilaveli ! 8°40'0"N ! Morawewa ! ! Kambakkoddai Pankulam Periyakulam ! Mankanai ! ! ! Sempadu Sampaltivu ! ! !Uppuveli Kanniyai Town & Gravets 8°35'0"N !China Bay ! Indian Ocean Vayiriuttu ! TrincomaleeTown Kapalturai Anuradhapura ! Palampaddaru Foul Point Thampalakamam ! Kiliveddy Transit Sites ! Puthukudiyirippu Inset Map ! Kinniyai ! Muttur 8°30'0"N Pokkuruni ! ! Alankerny Sampoor Ilakkantai ! Kovil Kudiyiruppu ! Thampalakamam ! ! ! Sunkankuli -

Lions Clubs International Club Membership Register
LIONS CLUBS INTERNATIONAL CLUB MEMBERSHIP REGISTER SUMMARY THE CLUBS AND MEMBERSHIP FIGURES REFLECT CHANGES AS OF FEBRUARY 2010 MEMBERSHI P CHANGES CLUB CLUB LAST MMR FCL YR TOTAL IDENT CLUB NAME DIST NBR STATUS RPT DATE OB NEW RENST TRANS DROPS NETCG MEMBERS 5024 025598 KANDY 306 C1 4 02-2010 56 0 0 0 -3 -3 53 5024 025599 S JAYAWARDENA P-KOTTE 306 C1 4 02-2010 39 3 1 0 -1 3 42 5024 034558 BATTARAMULLA 306 C1 4 02-2010 26 1 0 0 -2 -1 25 5024 037093 MATALE 306 C1 4 02-2010 33 0 0 0 0 0 33 5024 037269 SRI JAYAWARDENAPURA NEW TOWN 306 C1 4 02-2010 10 2 0 0 -3 -1 9 5024 038505 KOLONNAWA 306 C1 4 02-2010 24 0 0 0 0 0 24 5024 041219 KANDY SENKADAGALA 306 C1 4 02-2010 46 6 0 0 -7 -1 45 5024 042006 COLOMBO WEKANDA 306 C1 4 02-2010 21 0 0 0 0 0 21 5024 042593 COLOMBO FORT 306 C1 4 02-2010 46 1 0 0 0 1 47 5024 043921 TALANGAMA MALABE 306 C1 4 02-2010 28 0 1 0 -2 -1 27 5024 045813 MULLERIYAWA NEW TOWN 306 C1 4 02-2010 12 0 0 0 0 0 12 5024 045935 AVISSAWELLA 306 C1 4 02-2010 33 0 0 0 -4 -4 29 5024 048833 WICKRAMASINGHEPURA 306 C1 4 02-2010 42 1 0 0 -2 -1 41 5024 051362 COLOMBO TORRINGTON 306 C1 4 02-2010 20 0 0 0 0 0 20 5024 051390 PELAWATTA 306 C1 4 02-2010 28 5 0 0 0 5 33 5024 053236 TRINCOMALEE TOWN 306 C1 4 02-2010 43 11 4 0 -10 5 48 5024 053710 HINGURAKGODA & MEDIRIGIRIYA LC 306 C1 4 02-2010 34 0 0 1 -3 -2 32 5024 053940 DAMBULLA 306 C1 7 12-2009 26 0 0 0 0 0 26 5024 054120 MAWANELLA 306 C1 4 02-2010 38 2 0 0 -1 1 39 5024 054480 SRI JAYAWARDENAPURA METRO 306 C1 7 02-2010 19 0 0 0 0 0 19 5024 054989 COLOMBO MAITLAND 306 C1 4 02-2010 33 4 0 0 -

Eastern Province Biodiversity Profile and Conservation Action Plan
EASTERN PROVINCE BIODIVERSITY PROFILE AND CONSERVATION ACTION PLAN ,---~ ~- . f P-r~tP~tc\\ • ,_-- ··" : 9Hfct!O:"" 'l · . \ I -:: ~te, ·,t\.!~.' . ·· : -.;; ,,,;~(' \ J..,I ,.,. ~ , ,.. , ., Ht~,\~ _•! .. r 1t •.• \ Arc,-. <it::~:,~·--~:·.·:•·. .,~---·' i ( "oi· ... , --:-- ·- · ··-·· . ··· ···•• I . , . ., · - • , . .. ,., • ••·• • • • ' ' \ \ \ "\·•'-'"• •... ..... ' " ....,... t · · - · ~· ~ . ...... ~ .. .... .. i .'.\.\'•·,-··· :-·· ....... ........ ' Thangamuthu Jay~singam--· · ··· ···············-········ ; ~ • .... ... .r- l ~ ~~,· .. ~; ..~/ ~:,·1:u~ • •. __ .. ·-~ -..., ;\ai !I \ · . ~- l , ,i ,;,,~11·- • \ Vt '\!_;':!"!J ~ i • .• • ' l i"\.-~ lL -~:r,;.c-~(.;--- t • ~ • A Publication of Biodiversity Secretariat Ministry of Environment and Natural Resources Sri Lanka November 2008 ~~.. The Ministry of Environment and Natural Resources acknowledges the ADB/GEF, \.mM,L Government of the Netherlands funded Protected Area Management and Wildlife "'¥_. Conservation Project (Component "C") for providing financial assistance. Copyright: © Ministty of Environment and Natural Resources, Colombo, Sri Lanka Publisher: Biodiversity Secretariat Ministiy of Environment and Natural Resources, Sri Lanka Citation: Jayasingham, T. (2008) : Eastern Province Biodiversity Profile and Conservation Action Plan. The Biodiversity Secretariat, Ministry of Environment and Natural Resources, Sri Lanka. ISBN: 978-955-9120-92-6 First Print: December, 2008 Coordinated by: Lathika Hapuarachchi Saranga Jayasundara Printed by: Karunaratne & Sons (Pvt) Ltd. -
EB PMAS Class 2 2011 2.Pdf
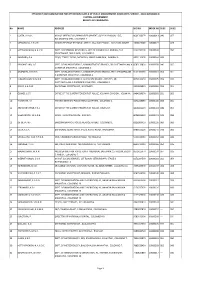
EFFICIENCY BAR EXAMINATION FOR OFFICERS IN CLASS II OF PUBLIC MANAGEMENT ASSISTANT'S SERVICE - 2011(II)2013(2014) CENTRAL GOVERNMENT RESULTS OF CANDIDATES No NAME ADDRESS NIC NO INDEX NO SUB1 SUB2 1 COSTA, K.A.G.C. M/Y OF DEFENCE & URBAN DEVELOPMENT, SUPPLY DIVISION, 15/5, 860170337V 10000013 040 057 BALADAKSHA MW, COLOMBO 3. 2 MEDAGODA, G.R.U.K. INLAND REVENUE REGIONAL OFFICE, 334, GALLE ROAD, KALUTARA SOUTH. 745802338V 10000027 --- 024 3 HETTIARACHCHI, H.A.S.W. DEPT. OF EXTERNAL RESOURCES, M/Y OF FINANCE & PLANNING, THE 823273010V 10000030 --- 050 SECRETARIAT, 3RD FLOOR, COLOMBO 1. 4 BANDARA, P.A. 230/4, TEMPLE ROAD, BATAPOLA, MADELGAMUWA, GAMPAHA. 682113260V 10000044 ABS --- 5 PRASANTHIKA, L.G. DEPT. OF INLAND REVENUE, ADMINISTRATIVE BRANCH, SRI CHITTAMPALAM A 858513383V 10000058 040 055 GARDINER MAWATHA, COLOMBO 2. 6 ATAPATTU, D.M.D.S. DEPT. OF INLAND REVENUE, ADMINISTRATION BRANCH, SRI CHITTAMPALAM 816130069V 10000061 054 051 A GARDINER MAWATHA, COLOMBO 2. 7 KUMARIHAMI, W.M.S.N. DEPT. OF INLAND REVENUE, ACCOUNTS BRANCH, POB 515, SRI 867010025V 10000075 059 070 CHITTAMPALAM A GARDINER MAWATHA, COLOMBO 2. 8 JENAT, A.A.D.M. DIVISIONAL SECRETARIAT, NEGOMBO. 685060892V 10000089 034 051 9 GOMES, J.S.T. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA DIVISION, KELANIYA. 846453857V 10000092 031 052 10 HARSHANI, A.I. FINANCE BRANCH, POLICE HEAD QUARTERS, COLOMBO 1. 827122858V 10000104 064 061 11 ABHAYARATHNE, Y.P.J. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA. 841800117V 10000118 049 057 12 WEERAKOON, W.A.D.B. 140/B, THANAYAM PLACE, INGIRIYA. 802893329V 10000121 049 068 13 DE SILVA, W.I.