PAN3–PSMA2 Fusion Resulting from a Novel T(7;13)(P14;Q12) Chromosome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effect of Temperature Adaptation on the Ubiquitin–Proteasome Pathway in Notothenioid Fishes Anne E
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 369-378 doi:10.1242/jeb.145946 RESEARCH ARTICLE The effect of temperature adaptation on the ubiquitin–proteasome pathway in notothenioid fishes Anne E. Todgham1,*, Timothy A. Crombie2 and Gretchen E. Hofmann3 ABSTRACT proliferation to compensate for the effects of low temperature on ’ There is an accumulating body of evidence suggesting that the sub- aerobic metabolism (Johnston, 1989; O Brien et al., 2003; zero Antarctic marine environment places physiological constraints Guderley, 2004). Recently, there has been an accumulating body – on protein homeostasis. Levels of ubiquitin (Ub)-conjugated proteins, of literature to suggest that protein homeostasis the maintenance of – 20S proteasome activity and mRNA expression of many proteins a functional protein pool has been highly impacted by evolution involved in both the Ub tagging of damaged proteins as well as the under these cold and stable conditions. different complexes of the 26S proteasome were measured to Maintaining protein homeostasis is a fundamental physiological examine whether there is thermal compensation of the Ub– process, reflecting a dynamic balance in synthetic and degradation proteasome pathway in Antarctic fishes to better understand the processes. There are numerous lines of evidence to suggest efficiency of the protein degradation machinery in polar species. Both temperature compensation of protein synthesis in Antarctic Antarctic (Trematomus bernacchii, Pagothenia borchgrevinki)and invertebrates (Whiteley et al., 1996; Marsh et al., 2001; Robertson non-Antarctic (Notothenia angustata, Bovichtus variegatus) et al., 2001; Fraser et al., 2002) and fish (Storch et al., 2005). In notothenioids were included in this study to investigate the zoarcid fishes, it has been demonstrated that Antarctic eelpouts mechanisms of cold adaptation of this pathway in polar species. -

Hematopoietic Differentiation
Hematopoietic Differentiation A number of lineages of mature cells are derived by a series of steps from a common stem cell precursor. Myeloid cells including neutrophils and monocytes are important for early defense against infection and because of the occurrence of myeloid leukemias. Myeloid differentiation and activation offers a favorable system for experimental investigation. Some Models of Gene Expression in Myeloid Cells 1. Compare resting neutrophils with neutrophils exposed for two hours to either. – A. Non-pathogenic E. coli. – B. Yersinia pestis D27 (plague bacillus). – C. Non-pathogenic Yersinia D28. 2. Induced differentiation of MPRO promyelocytic cells. NeutrophilsNeutrophils Major frontline defense cells against invading pathogens. – Constitute 70% of the total blood leukocytes. – Terminally differentiated professional phagocytic cells with an antibacterial arsenal. – Use both oxygen dependent and oxygen independent killing mechanisms. Play a central role in 2000X mag inflammation. Distribution of IL-8 transcripts on neutrophils (in situ hybridization) A combination of two Cy3 (red)- A labeled oligonucleotides complementary to IL-8 transcripts were used for in situ hybridization with neutrophils incubated in the absence (A) or presence (B) of ten E. coli K12 organisms per neutrophil. BB Methods of Analysis 1. mRNA analysis. – A. 3’ end restriction fragment gel display. – B. Affymetrix 60k or 42k oligonucleotide arrays. 2. Protein analysis. 2D gel electrophoresis using a variety of ph ranges for isoelectric focusing. MALDI-TOF identification of proteins. Representative Segments of Display Gels of cDNA Fragments: (Left) Neutrophils and Monocytes Exposed to E. coli for 2 H; (Right) Neutrophils Exposed to Various Bacteria for 2 H Ec: E. coli K12; Yp (KIM5): Y. -

Isolation and Characterization of Lymphocyte-Like Cells from a Lamprey
Isolation and characterization of lymphocyte-like cells from a lamprey Werner E. Mayer*, Tatiana Uinuk-ool*, Herbert Tichy*, Lanier A. Gartland†, Jan Klein*, and Max D. Cooper†‡ *Max-Planck-Institut fu¨r Biologie, Abteilung Immungenetik, Corrensstrasse 42, D-72076 Tu¨bingen, Germany; and †Howard Hughes Medical Institute, University of Alabama, 378 Wallace Tumor Institute, Birmingham, AL 35294 Contributed by Max D. Cooper, August 30, 2002 Lymphocyte-like cells in the intestine of the sea lamprey, Petro- existence of the adaptive immune system in jawless fishes, myzon marinus, were isolated by flow cytometry under light- the identity of these cells has remained in doubt. The aim of the scatter conditions used for the purification of mouse intestinal present study was to exploit contemporary methods of cell lymphocytes. The purified lamprey cells were morphologically separation to isolate the agnathan lymphocyte-like cells to indistinguishable from mammalian lymphocytes. A cDNA library characterize them morphologically and by the genes they was prepared from the lamprey lymphocyte-like cells, and more express. than 8,000 randomly selected clones were sequenced. Homology searches comparing these ESTs with sequences deposited in the Materials and Methods databases led to the identification of numerous genes homologous Source and Preparation of Cell Suspension. Ammocoete larvae to those predominantly or characteristically expressed in mamma- (8–13 cm long) of the sea lamprey, Petromyzon marinus (from lian lymphocytes, which included genes controlling lymphopoiesis, Lake Huron, MI) were dissected along the ventral side to extract intracellular signaling, proliferation, migration, and involvement the intestine and the associated typhlosole (spiral valve). Cells of lymphocytes in innate immune responses. -

Role of Phytochemicals in Colon Cancer Prevention: a Nutrigenomics Approach
Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan J van Erk Promotor: Prof. Dr. P.J. van Bladeren Hoogleraar in de Toxicokinetiek en Biotransformatie Wageningen Universiteit Co-promotoren: Dr. Ir. J.M.M.J.G. Aarts Universitair Docent, Sectie Toxicologie Wageningen Universiteit Dr. Ir. B. van Ommen Senior Research Fellow Nutritional Systems Biology TNO Voeding, Zeist Promotiecommissie: Prof. Dr. P. Dolara University of Florence, Italy Prof. Dr. J.A.M. Leunissen Wageningen Universiteit Prof. Dr. J.C. Mathers University of Newcastle, United Kingdom Prof. Dr. M. Müller Wageningen Universiteit Dit onderzoek is uitgevoerd binnen de onderzoekschool VLAG Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan Jolanda van Erk Proefschrift ter verkrijging van graad van doctor op gezag van de rector magnificus van Wageningen Universiteit, Prof.Dr.Ir. L. Speelman, in het openbaar te verdedigen op vrijdag 1 oktober 2004 des namiddags te vier uur in de Aula Title Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Author Marjan Jolanda van Erk Thesis Wageningen University, Wageningen, the Netherlands (2004) with abstract, with references, with summary in Dutch ISBN 90-8504-085-X ABSTRACT Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Specific food compounds, especially from fruits and vegetables, may protect against development of colon cancer. In this thesis effects and mechanisms of various phytochemicals in relation to colon cancer prevention were studied through application of large-scale gene expression profiling. Expression measurement of thousands of genes can yield a more complete and in-depth insight into the mode of action of the compounds. -
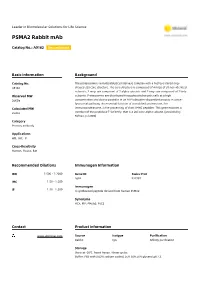
PSMA2 Rabbit Mab
Leader in Biomolecular Solutions for Life Science PSMA2 Rabbit mAb Catalog No.: A9182 Recombinant Basic Information Background Catalog No. The proteasome is a multicatalytic proteinase complex with a highly ordered ring- A9182 shaped 20S core structure. The core structure is composed of 4 rings of 28 non-identical subunits; 2 rings are composed of 7 alpha subunits and 2 rings are composed of 7 beta Observed MW subunits. Proteasomes are distributed throughout eukaryotic cells at a high 26KDa concentration and cleave peptides in an ATP/ubiquitin-dependent process in a non- lysosomal pathway. An essential function of a modified proteasome, the Calculated MW immunoproteasome, is the processing of class I MHC peptides. This gene encodes a 25kDa member of the peptidase T1A family, that is a 20S core alpha subunit. [provided by RefSeq, Jul 2008] Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 5683 P25787 IHC 1:50 - 1:200 Immunogen 1:50 - 1:200 IF A synthesized peptide derived from human PSMA2 Synonyms HC3; MU; PMSA2; PSC2 Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,0.05% BSA,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using PSMA2 Rabbit mAb (A9182) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. -

Supplementary Table S1. Correlation Between the Mutant P53-Interacting Partners and PTTG3P, PTTG1 and PTTG2, Based on Data from Starbase V3.0 Database
Supplementary Table S1. Correlation between the mutant p53-interacting partners and PTTG3P, PTTG1 and PTTG2, based on data from StarBase v3.0 database. PTTG3P PTTG1 PTTG2 Gene ID Coefficient-R p-value Coefficient-R p-value Coefficient-R p-value NF-YA ENSG00000001167 −0.077 8.59e-2 −0.210 2.09e-6 −0.122 6.23e-3 NF-YB ENSG00000120837 0.176 7.12e-5 0.227 2.82e-7 0.094 3.59e-2 NF-YC ENSG00000066136 0.124 5.45e-3 0.124 5.40e-3 0.051 2.51e-1 Sp1 ENSG00000185591 −0.014 7.50e-1 −0.201 5.82e-6 −0.072 1.07e-1 Ets-1 ENSG00000134954 −0.096 3.14e-2 −0.257 4.83e-9 0.034 4.46e-1 VDR ENSG00000111424 −0.091 4.10e-2 −0.216 1.03e-6 0.014 7.48e-1 SREBP-2 ENSG00000198911 −0.064 1.53e-1 −0.147 9.27e-4 −0.073 1.01e-1 TopBP1 ENSG00000163781 0.067 1.36e-1 0.051 2.57e-1 −0.020 6.57e-1 Pin1 ENSG00000127445 0.250 1.40e-8 0.571 9.56e-45 0.187 2.52e-5 MRE11 ENSG00000020922 0.063 1.56e-1 −0.007 8.81e-1 −0.024 5.93e-1 PML ENSG00000140464 0.072 1.05e-1 0.217 9.36e-7 0.166 1.85e-4 p63 ENSG00000073282 −0.120 7.04e-3 −0.283 1.08e-10 −0.198 7.71e-6 p73 ENSG00000078900 0.104 2.03e-2 0.258 4.67e-9 0.097 3.02e-2 Supplementary Table S2. -

Cell Type-Specific Analysis of Human Interactome and Transcriptome Shahin Mohammadi Purdue University
Purdue University Purdue e-Pubs Open Access Dissertations Theses and Dissertations January 2016 Cell Type-specific Analysis of Human Interactome and Transcriptome Shahin Mohammadi Purdue University Follow this and additional works at: https://docs.lib.purdue.edu/open_access_dissertations Recommended Citation Mohammadi, Shahin, "Cell Type-specific Analysis of Human Interactome and Transcriptome" (2016). Open Access Dissertations. 1371. https://docs.lib.purdue.edu/open_access_dissertations/1371 This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. Graduate School Form 30 Updated 12/26/2015 PURDUE UNIVERSITY GRADUATE SCHOOL Thesis/Dissertation Acceptance This is to certify that the thesis/dissertation prepared By Shahin Mohammadi Entitled CELL TYPE-SPECIFIC ANALYSIS OF HUMAN INTERACTOME AND TRANSCRIPTOME For the degree of Doctor of Philosophy Is approved by the final examining committee: Ananth Grama Wojciech Szpankowski Chair David Gleich Jennifer Neville Markus Lill To the best of my knowledge and as understood by the student in the Thesis/Dissertation Agreement, Publication Delay, and Certification Disclaimer (Graduate School Form 32), this thesis/dissertation adheres to the provisions of Purdue University’s “Policy of Integrity in Research” and the use of copyright material. Approved by Major Professor(s): Ananth Grama William Gorman, Assistant to the Department Head 11/1/2016 Approved by: Head of the Departmental Graduate Program Date CELL TYPE-SPECIFIC ANALYSIS OF HUMAN INTERACTOME AND TRANSCRIPTOME A Dissertation Submitted to the Faculty of Purdue University by Shahin Mohammadi In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy December 2016 Purdue University West Lafayette, Indiana ii I dedicate this thesis to my mom, whose role in my life I can not even begin to describe. -

Melanoma Cell Resistance to Vemurafenib Modifies Inter-Cellular
biomedicines Article Melanoma Cell Resistance to Vemurafenib Modifies Inter-Cellular Communication Signals Claudio Tabolacci 1,* , Martina Cordella 1, Sabrina Mariotti 2, Stefania Rossi 1 , Cinzia Senatore 1, Carla Lintas 3 , Lauretta Levati 4, Daniela D’Arcangelo 4, Antonio Facchiano 4 , Stefania D’Atri 4, Roberto Nisini 2 and Francesco Facchiano 1,* 1 Department of Oncology and Molecular Medicine, Istituto Superiore di Sanità, Viale Regina Elena 299, 00161 Rome, Italy; [email protected] (M.C.); [email protected] (S.R.); [email protected] (C.S.) 2 Department of Infectious Diseases, Istituto Superiore di Sanità, 00161 Rome, Italy; [email protected] (S.M.); [email protected] (R.N.) 3 Department of Experimental Medicine, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] 4 Laboratory of Molecular Oncology, IDI-IRCCS, 00167 Rome, Italy; [email protected] (L.L.); [email protected] (D.D.); [email protected] (A.F.); [email protected] (S.D.) * Correspondence: [email protected] (C.T.); [email protected] (F.F.) Abstract: The therapeutic success of BRAF inhibitors (BRAFi) and MEK inhibitors (MEKi) in BRAF- mutant melanoma is limited by the emergence of drug resistance, and several lines of evidence suggest that changes in the tumor microenvironment can play a pivotal role in acquired resistance. The present study focused on secretome profiling of melanoma cells sensitive or resistant to the BRAFi vemurafenib. Proteomic and cytokine/chemokine secretion analyses were performed in order to better understand the interplay between vemurafenib-resistant melanoma cells and the tumor microenvironment. We found that vemurafenib-resistant melanoma cells can influence dendritic Citation: Tabolacci, C.; Cordella, M.; cell (DC) maturation by modulating their activation and cytokine production. -

Functional Gene Clusters in Global Pathogenesis of Clear Cell Carcinoma of the Ovary Discovered by Integrated Analysis of Transcriptomes
International Journal of Environmental Research and Public Health Article Functional Gene Clusters in Global Pathogenesis of Clear Cell Carcinoma of the Ovary Discovered by Integrated Analysis of Transcriptomes Yueh-Han Hsu 1,2, Peng-Hui Wang 1,2,3,4,5 and Chia-Ming Chang 1,2,* 1 Department of Obstetrics and Gynecology, Taipei Veterans General Hospital, Taipei 112, Taiwan; [email protected] (Y.-H.H.); [email protected] (P.-H.W.) 2 School of Medicine, National Yang-Ming University, Taipei 112, Taiwan 3 Institute of Clinical Medicine, National Yang-Ming University, Taipei 112, Taiwan 4 Department of Medical Research, China Medical University Hospital, Taichung 440, Taiwan 5 Female Cancer Foundation, Taipei 104, Taiwan * Correspondence: [email protected]; Tel.: +886-2-2875-7826; Fax: +886-2-5570-2788 Received: 27 April 2020; Accepted: 31 May 2020; Published: 2 June 2020 Abstract: Clear cell carcinoma of the ovary (ovarian clear cell carcinoma (OCCC)) is one epithelial ovarian carcinoma that is known to have a poor prognosis and a tendency for being refractory to treatment due to unclear pathogenesis. Published investigations of OCCC have mainly focused only on individual genes and lack of systematic integrated research to analyze the pathogenesis of OCCC in a genome-wide perspective. Thus, we conducted an integrated analysis using transcriptome datasets from a public domain database to determine genes that may be implicated in the pathogenesis involved in OCCC carcinogenesis. We used the data obtained from the National Center for Biotechnology Information (NCBI) Gene Expression Omnibus (GEO) DataSets. We found six interactive functional gene clusters in the pathogenesis network of OCCC, including ribosomal protein, eukaryotic translation initiation factors, lactate, prostaglandin, proteasome, and insulin-like growth factor. -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................ -

Stem Cells® Original Article
® Stem Cells Original Article Properties of Pluripotent Human Embryonic Stem Cells BG01 and BG02 XIANMIN ZENG,a TAKUMI MIURA,b YONGQUAN LUO,b BHASKAR BHATTACHARYA,c BRIAN CONDIE,d JIA CHEN,a IRENE GINIS,b IAN LYONS,d JOSEF MEJIDO,c RAJ K. PURI,c MAHENDRA S. RAO,b WILLIAM J. FREEDa aCellular Neurobiology Research Branch, National Institute on Drug Abuse, Department of Health and Human Services (DHHS), Baltimore, Maryland, USA; bLaboratory of Neuroscience, National Institute of Aging, DHHS, Baltimore, Maryland, USA; cLaboratory of Molecular Tumor Biology, Division of Cellular and Gene Therapies, Center for Biologics Evaluation and Research, Food and Drug Administration, Bethesda, Maryland, USA; dBresaGen Inc., Athens, Georgia, USA Key Words. Embryonic stem cells · Differentiation · Microarray ABSTRACT Human ES (hES) cell lines have only recently been compared with pooled human RNA. Ninety-two of these generated, and differences between human and mouse genes were also highly expressed in four other hES lines ES cells have been identified. In this manuscript we (TE05, GE01, GE09, and pooled samples derived from describe the properties of two human ES cell lines, GE01, GE09, and GE07). Included in the list are genes BG01 and BG02. By immunocytochemistry and reverse involved in cell signaling and development, metabolism, transcription polymerase chain reaction, undifferenti- transcription regulation, and many hypothetical pro- ated cells expressed markers that are characteristic of teins. Two focused arrays designed to examine tran- ES cells, including SSEA-3, SSEA-4, TRA-1-60, TRA-1- scripts associated with stem cells and with the 81, and OCT-3/4. Both cell lines were readily main- transforming growth factor-β superfamily were tained in an undifferentiated state and could employed to examine differentially expressed genes. -

Advancing the Role of Gamma-Tocotrienol As Proteasomes Inhibitor: a Quantitative Proteomic Analysis of MDA-MB-231 Human Breast Cancer Cells
biomolecules Article Advancing the Role of Gamma-Tocotrienol as Proteasomes Inhibitor: A Quantitative Proteomic Analysis of MDA-MB-231 Human Breast Cancer Cells Premdass Ramdas 1,2, Ammu Kutty Radhakrishnan 3 , Asmahani Azira Abdu Sani 4 , Mangala Kumari 5, Jeya Seela Anandha Rao 6 and Puteri Shafinaz Abdul-Rahman 1,7,* 1 Department of Molecular Medicine, Faculty of Medicine, University of Malaya, 50603 Kuala Lumpur, Malaysia; [email protected] 2 Department of Medical Biotechnology, School of Health Sciences, International Medical University, 57000 Kuala Lumpur, Malaysia 3 Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Bandar Sunway, 47500 Selangor, Malaysia; [email protected] 4 Malaysian Genome Institute, National Institute of Biotechnology, 43000 Bangi, Malaysia; [email protected] 5 Division of Human Biology, International Medical University, 57000 Kuala Lumpur, Malaysia; [email protected] 6 Division of Pathology, International Medical University, 57000 Kuala Lumpur, Malaysia; [email protected] 7 University of Malaya Centre of Proteomics Research (UMCPR), University of Malaya, 50603 Kuala Lumpur, Malaysia * Correspondence: [email protected] Received: 27 November 2019; Accepted: 14 December 2019; Published: 21 December 2019 Abstract: Tocotrienol, an analogue of vitamin E has been known for its numerous health benefits and anti-cancer effects. Of the four isoforms of tocotrienols, gamma-tocotrienol (γT3) has been frequently reported for their superior anti-tumorigenic activity in both in vitro and in vivo studies, when compared to its counterparts. In this study, the effect of γT3 treatment in the cytoplasmic and nuclear fraction of MDA-MB-231 human breast cancer cells were assessed using the label-free quantitative proteomics analysis.