MARYLAND STATE POLICE COVID-19 Exposure Determination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

State Police · ([, , -Faa.' * ¥S@ N
If you have issues viewing or accessing this file contact us at NCJRS.gov. , , \~\ .... , i > or <::::,•. " Maryland state Police · ([, , -fAA.' * ¥S@ n • '- . " , , • .. '. , , '., M • Q triOJl3 • , , " , ~""'"., " · ,', (0703 CJ • 107039 U.S. Department of JUstice National Institute of Justice This document has been reproduced exactly as received from the person or organization originating it. Points of view or opinions stated in this document are those of the authors and do not necessarily represent the official position or policies of the National Institute of • Justice. Permission to reproduce this copyrighted material has been granted by ~1aryland State Police • to the National Criminal Justice Reference Service (NCJRS). FUrther reproduction outside of the NCJRS system requires permis sion of the copyright owner. • ANNU~L REPORT • • • GEORGE B· BROSAN SUPERINTENDENT • PREPARED By: PLANNING AND RESEARCH UIVISION MARYLAND STATE POLICE • • STATE OF MARYLAND DEPARTMENT OF PUBLIC SAFETY AND CORRECTIONAL SERVICES BISHOP L. ROBINSON MARYLAND STATE POLICE SECmTARY PIKESVILLE, MARYLAND 21208-3899 PUBL IC SAFETY AND WIL.LlAM DONALD SCHAEFER CORRECTIONAL SERVICES • - GOVERNOR AREA CODE 301 486-3101 TTY FOR DEAF AREA CODE 301 488-0677 John J. O'Neill MELVIN A. STEINBERG Acting Superintendent LT. GOVEnNOR MARYLAND STATE POLICE June 26 I 1987 • The Honorable WillIam Donald Schaefer Governor of the State of Maryland State House Annapolis, Maryland 21404 • Dear Governor Schaefer: The Maryland State PolIce Is pleased to submit to you the 1986 Annual Report which reflects the services this Agency rendered to the citizens of Maryland during the year. • The Anti-Driving While IntoxIcated (OWl) efforts continue to be effec tive. In 1986, the percentage of alcohol related accidents was at an all time low of 47.5 percent. -

State Highway Patrols-Their Functions and Financing
State Highway Patrols-Their Functions and Financing EDWARD A. GLADSTONE and THOMAS W. COOPER, U.S. Bureau of Public Roads, Office of Planning •CONCERN FOR the safety of the motoring public, and the importance of the state police organizations in enforcing traffic and safety laws, was voiced by the governors of most of the 47 states in which the legislatures met in regular session in 1965. In state after state the governor's message emphasized highway safety and pointed to the need for additional highway patrol troops to curb highway accidents and fatalities. In at least 30 states requests were made for an increase in patrol strength, either by the governor, by legislative committees, or by safety agencies. Collectively, specific requests were made in 21 states for nearly 3, 800 troopers to be added to the patrol strength within the next onP. to four years. A summary of the requests (as of mid-1965) is given in Table 1. If approved, these requests would increase patrol strength by an average of 23 percent. TAB LE 1 REQUESTS FOR ADDITIONAL PATROL TROOPERS, SUBMITTED TO 1965 STATE LEGISLATURES BY GOVERNORS, LEGISLATIVE COMMITTEES, OR OTHERS Number Number St,it,,, (uhPr" stl\te~) State (where stated) Arkansas - New York 112 California 195 North Carolina 200 (4 years) Florida 212 Ohio 4-00 (2 years) Georgia 8o (2 years) Oklahoma 100 (2 years) Illinois 8oo ( 4 years) Pennsylvanla 300 Indiena 150 South Carolina - Iowa 100 (2 years) South Dakota - KMSt\8 50 Tennessee 100 Maryland 4o Texas - Michigan 200 Utah 20 Minnesota 368 (by 1973) Vermont 42 (2 years) Missouri 250 Washington - Nebraska 50 West Virginia - Nevada - Wisconsin - New Mexico 10 Wyoming - Source: Daily legislative bulletins published by the National. -

Wilkins V. Maryland State Police
Wilkins v. Maryland State Police "^ irHH •••HBW H m !••••• «• •• IIP • •• •• PP-MD-002-007 UNITED STATES DISTRICT COURT FOR THE DISTRICT OF MARYLAND ROBERT L. WILKINS, ) individually and on behalf of ) all other persons similarly ) situated, ) 1620 Fuller Street, N.W. ) Apartment #505 ) Washington, D.C., 20009, ) ) NORMAN SCOTT EL-AMIN, ) individually and on behalf of ) all other persons similarly ) situated, ) 15271 Waterwheel Terrace ) Woodbridge, Virginia 22191, ) ) NU'MAN W. EL-AMIN, ) individually and on behalf of ) all other persons similarly ) situated, ) 5761 Harwich Court ) Apartment #222 ) Alexandria, Virginia 22311, ) ) and > ) AQUILA ABDULLAH, ) individually and on behalf of ) all other persons similarly ) situated, . ) 5761 Harwich Court ) Apartment #222 ) Alexandria, Virginia 22311, ) ) Plaintiffs, ) ) CÌVÌI NO. fÅiSQ ¿?3 ) ) MARYLAND STATE POLICE, ) SERVE: ) Colonel Larry W. Tolliver ) Superintendent, ) Maryland State Police ) 1201 Reisterstown Road ) Pikesville, Maryland 21208, ) ) TFC. BRYAN W. HUGHES, ¯ ) Badge #1817, ) individually and in his official ) capacity, ) Barrack "C" Cumberland ) 1125 National Highway ) Cumberland, Maryland, 21502, ) ) TFC. EDWARD V. SYRACUSE, ) Badge #3152, ) . · individually and in his official ) capacity, ) Aviation Division ) Cumberland Section ) Rt. 1, Box 100 ) Wiley Ford, West Virginia 26767, ) ) DEPUTY SHERIFF RONALD BROWN, ) individually and in his official ) capacity, ) 708 Furnace Street ) Cumberland, Maryland 21502, ) ) JOHN W. STOTLER, ) in his official capacity as ) President -

Iacp New Members
44 Canal Center Plaza, Suite 200 | Alexandria, VA 22314, USA | 703.836.6767 or 1.800.THEIACP | www.theIACP.org IACP NEW MEMBERS New member applications are published pursuant to the provisions of the IACP Constitution. If any active member in good standing objects to an applicant, written notice of the objection must be submitted to the Executive Director within 60 days of publication. The full membership listing can be found in the online member directory under the Participate tab of the IACP website. Associate members are indicated with an asterisk (*). All other listings are active members. Published February 1, 2021. Canada British Columbia Vancouver Spearn, Bill, Superintendent, Vancouver Police Department Ontario North Bay McFarlane, Scott, Inspector, North Bay Police Service Saskatchewan Saskatoon *Barber, Shelby, Immigration Enforcement Officer, Canada Border Services Agency Czech Republic Brno *Wright, Adam, Area Sales Manager, Phonexia SRO France Malakoff Gaspard, Rudy, Colonel, Gendarmerie Nationale Ghana Accra *Asante, Christabel, Lance corporal, Ghana Police Service *Gyamfi, Opoku, Corporal, Ghana Police Service *Kyei, Bright, Lance Corporal, Ghana Police Service *Mensah, Moses, Corporal, Ghana Police Service *Ofosu, Seth, Corporal, Ghana Police Service Moldova Chisinau *Pantea, Serghei, Criminal Prosecution Officer, Ministry of Internal Affairs Netherlands The Hague *Viedma, Julia, Head of the Operational & Analysis Centre, EUROPOL Nigeria Abuja - FCT *Nwachukwu, Chinyere, Deputy Superintendent of Customs, Nigeria Customs -

Review of Police Disciplinary Procedures in Maryland and Other States Review of Police Disciplinary Procedures in Maryland and Other States
Review of Police Disciplinary Procedures in Maryland and Other States Review of Police Disciplinary Procedures in Maryland and Other States Project X-47 Prepared by Jeanne E. Bilanin Institute for Governmental Service University of Maryland Center for Applied Policy Studies 4511 Knox Road, Suite 205 College Park, Maryland 20742 June 1999 Contents Acknowledgments ..............................................................ii Executive Summary ............................................................ iii Introduction ...................................................................1 Current Law in Maryland ...................................................1 1997 Proposal to Change Current Maryland Law .................................5 Study Methodology .......................................................5 Comparison of State Statutes ......................................................8 Officers Covered by Statutory Provisions .......................................8 Requirements Concerning Internal Investigations .................................10 Requirements Concerning Disciplinary Procedures ...............................15 Hearing Requirements ....................................................15 Hearing Board Composition ................................................18 Selection of Hearing Board Members .........................................21 Effect of Decision ........................................................22 Appeals ...............................................................25 Maryland Compared -
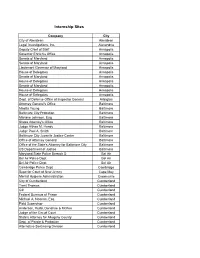
Internship Sites
Internship Sites Company City City of Aberdeen Aberdeen Legal Investigations, Inc. Alexandria Deputy Chief of Staff Annapolis Governor Ehrlich's Office Annapolis Senate of Maryland Annapolis Senate of Maryland Annapolis Lieutenant Governor of Maryland Annapolis House of Delegates Annapolis Senate of Maryland Annapolis House of Delegates Annapolis Senate of Maryland Annapolis House of Delegates Annapolis House of Delegates Annapolis Dept. of Defense Office of Inspector General Arlington Attorney General's Office Baltimore Maetta Young Baltimore Baltimore City Probation Baltimore Marlane Johnson, Esq. Baltimore States Attorney's Office Baltimore Judge Althea M. Handy Baltimore Judge Paul A. Smith Baltimore Baltimore City Juvenile Justice Center Baltimore Office of Attorney General Baltimore Office of the State's Attorney for Baltimore City Baltimore US Department of Justice Baltimore Maryland State Police Barrack D Bel Air Bel Air Police Dept. Bel Air Bel Air Police Dept. Bel Air Cambridge Police Dept Cambridge Superior Court of New Jersey Cape May Mental Hygiene Administration Crownsville City of Cumberland Cumberland Trent Thomas Cumberland C3I Cumberland Federal Bureaus of Prison Cumberland Michael A. Noonan, Esq. Cumberland Field Supervisor Cumberland Anderson, Rudd, Donahue & McKee Cumberland Judge of the Circuit Court Cumberland State's Attorney for Allegany County Cumberland Dept. of Parole & Probation Cumberland Alternative Sentincing Division Cumberland Allegany County Sheriff's Office Patrol Division Cumberland John Robb, Esq. -

Department of State Police Department of State Police Summary of Department of State Police Summary of Maryland State Police
Maryland State Police MISSION To ensure Maryland is a safe place to live, work and visit. VISION To serve and protect the citizens of Maryland while remaining focused on our core values of integrity, fairness and service. KEY GOALS, OBJECTIVES, AND PERFORMANCE MEASURES Goal 1. Prevent and investigate crime while supporting allied law enforcement agencies. Obj. 1.1 Use task forces, drug interdiction units, forensic and intelligence data to identify and arrest perpetrators of criminal acts. Performance Measures 2014 Act. 2015 Act. 2016 Act. 2017 Act. 2018 Act. 2019 Est. 2020 Est. Number of local drug task force investigations 1,366 1,810 1,731 1,977 1,898 1,900 1,900 Number of arrests 752 789 1,567 842 586 650 650 Number of drug interdiction investigations – Package Unit 476 366 406 362 281 300 300 Number of drug interdiction arrests 253 179 124 134 99 130 130 Amount of seized cash assets $2,853,638 $1,857,260 $8,428,716 $4,871,208 $7,311,121 $4,000,000 $3,700,000 Amount of forfeited cash assets $2,556,161 $3,508,238 $152,513 $251,969 $707,906 $450,000 $300,000 597 Amount of seized non-cash assets $1,438,065 $751,997 $521,111 $514,394 $534,704 $400,000 $400,000 Amount of forfeited non-cash assets $151,555 $117,771 $212,854 $82,380 $111,792 $120,000 $125,000 Obj. 1.2 The Vehicle Theft Prevention Council will assist jurisdictions having the highest auto theft rates by disseminating grant funding for special enforcement and prevention projects. -

Maj. Neill Franklin (Ret.) Baltimore City & Maryland State Police Departments White Hall, MD Executive Board Member
Maj. Neill Franklin (Ret.) Baltimore City & Maryland State Police Departments White Hall, MD Executive Board Member Major Neill Franklin (Ret.) is a 34-year law enforcement veteran of the Maryland State Police and Baltimore Police Department. After 23 years of dedicated service to the Maryland State Police, he was recruited in 2000 by the Commissioner of the Baltimore Police Department to reconstruct and command Baltimore’s Education and Training Section. During his time on the force, he held the position of commander for the Education and Training Division and the Bureau of Drug and Criminal Enforcement. He also instituted and oversaw the very first Domestic Violence Investigative Units for the Maryland State Police. While serving as a narcotics agent with the Maryland State Police, Maj. Franklin was persuaded by then-mayor Kurt Schmoke's declaration that the War on Drugs was counterproductive and created excessive violence. This, followed by the tragic murder of his close friend, Corporal Ed Toatley, while making a drug buy as an undercover agent, cemented his resolve to reform failed drug war policies. He retired from policing in 2010 to lead the Law Enforcement Action Partnership as executive director. After 10 years of leadership, Maj. Franklin retired as Executive Director of the Law Enforcement Action Partnership in 2020. He serves on many boards, including Murder Victims Families for Reconciliation, the Faith Based Community Council on Law Enforcement and Intelligence, the Place of Grace Church, Anne Arundel Community College Criminal Justice Advisory Board, and TurnAround Inc. The Law Enforcement Action Partnership is a nonprofit organization composed of police, prosecutors, judges, and other criminal justice professionals who use their expertise to advance drug policy and criminal justice solutions that improve public safety. -

UNITED STATES DISTRICT COURT DISTRICT of MARYLAND HISPANIC NATIONAL LAW ENFORCEMENT ASSOCIATION NCR P.O. Box 766 Cheltenham, MD
Case 8:18-cv-03821-CBD Document 1 Filed 12/12/18 Page 1 of 65 UNITED STATES DISTRICT COURT DISTRICT OF MARYLAND HISPANIC NATIONAL LAW ENFORCEMENT ASSOCIATION NCR P.O. Box 766 Cheltenham, MD 20623 UNITED BLACK POLICE OFFICERS ASSOCIATION P.O. Box 766 CIVIL ACTION NO.: 18-cv-03821 Cheltenham, MD 20623 MICHAEL ANIS 7600 Barlowe Rd COMPLAINT FOR DECLARATORY Landover, MD 20785 AND INJUNCTIVE RELIEF AND DAMAGES MICHAEL BROWN P.O. Box 1434 Bowie, MD 20717 DEMAND FOR JURY TRIAL THOMAS BOONE 601 Crain Hwy. Upper Marlboro, MD 20774 DANITA INGRAM 7600 Barlowe Rd Landover, MD 20785 PAUL MACK 7600 Barlowe Rd1 Landover, MD 20785 JOSEPH PEREZ 7600 Barlowe Rd Landover, MD 20785 TASHA OATIS PO Box 8532 Oakridge, MD 21075 1 This caption lists the professional addresses or post office boxes of the police officer Plaintiffs and Defendants because of the sensitivity of publicly disclosing home addresses of law enforcement professionals. US:163108711v1 Case 8:18-cv-03821-CBD Document 1 Filed 12/12/18 Page 2 of 65 CLARENCE RUCKER 401 Capitol Heights Blvd. Capitol Heights, MD 20743 CHRIS SMITH 7600 Barlowe Rd Landover, MD 20785 RICHARD TORRES 7600 Barlowe Rd Landover, MD 20785 THOMAS WALL 7600 Barlowe Rd Landover, MD 20785 and SONYA L. ZOLLICOFFER2 11108 Fort Washington, Rd. Fort Washington, MD 20744 Plaintiffs, PRINCE GEORGE’S COUNTY 14741 Governor Oden Bowie Drive Upper Marlboro, MD 20772 HENRY P. STAWINSKI, III, individually and in his official capacity as Chief of Police 7600 Barlowe Rd Landover, MD 20785 MARK A. MAGAW, individually and in his official capacity as Deputy Chief Administrative Officer for Public Safety 1301 McCormick Drive, Suite 4000 Largo, MD 20774 CHRISTOPHER MURTHA, individually and in his official capacity as Deputy Chief of Police 7600 Barlowe Rd Landover, MD 20785 2 Lt. -

Maryl(Lnd Statepq[Ice
.. ii4Q. .. 9* If you have issues viewing or accessing this file contact us at NCJRS.gov. f ,~ " ~I 4 Ly I~, tl' if '(l' This microfiche was produced from documents received for inclusion in the NCJRS data base. Since NCJRS cannot exercise .Maryl(lnd StatePQ[ice .. ... control over the physical condition of the documents submitted, -'~'..:..' "- : ~ " 'II,.I '.- the individual frame quality will vary. The resolution chart on , . , <:;:) this frame may be used to evaluate the document quality. -.-.---~-------1", I oj I I, 1 ....~ .... 1 j I 1 -,..i"_. _. __ .', .. ___ .. _____ . __ .__ .____ . ____________ . _~ _____ _ \\\\\ 1.25 111111.4_ IIIII 1.6 If . " MICROCOPY RESOLUTION TEST CHART NATIONAL BUREAU OF STANOAROS-1963-A Microfilming procedures used to create this fiche comply with the standards set forth in 41CFR 101-11.504. Points of view or opinions stated in this document are those of the author(s) and do not represent the official position or policies of the U. S. Department of Justice. '0 National Institute of Justice United States Department of Justice Washington, D. C. 20531 4/25/84 _\ '... ... W4t - ., lit' I:1 )1\' I, Ii~! ') U.S. Department of Justice \ National Institute of Justice ~ This document has been reproduced exactly as received from the person or organization originating it. Points of view or opinions stated in this document are those of the authors and do not pecessarily represeot the Qlficial position or policies of the National Institute of Justice. Permission to reproduce this copyrighted material has been granted by Maryland State Police to the National Criminal Justice Reference Service (NCJRS). -

Census of State and Local Law Enforcement Agencies, 2008 Brian A
U.S. Department of Justice Office of Justice Programs Bureau of Justice Statistics July 2011, NCJ 233982 Bulletin Census of State and Local Law Enforcement Agencies, 2008 Brian A. Reaves, Ph.D., BJS Statistician n September 2008, state and local law enforcement FIGURE 1 agencies employed more than 1.1 million persons Net increase in full-time sworn personnel employed on a full-time basis, including about 765,000 by state and local law enforcement agencies, per Isworn personnel (defined as those with general arrest 4-year period, 1992–2008 powers). Agencies also employed approximately 100,000 part-time employees, including 44,000 sworn officers. These findings come from the 2008 Bureau 2004-2008 33,343 of Justice Statistics’ (BJS) Census of State and Local Law Enforcement Agencies (CSLLEA), the fifth such census to be conducted since the quadrennial series 2000-2004 23,881 began in 1992. From 2004 to 2008, state and local agencies added a net total of about 33,000 full-time sworn personnel. 1996-2000 44,487 This was about 9,500 more than agencies added from 2000 to 2004 (figure 1), reversing a trend of declining growth observed in prior 4-year comparisons based 1992-1996 on the CSLLEA. Local police departments added the 55,513 most officers, about 14,000. Sheriffs’ offices and spe- cial jurisdiction agencies added about 8,000 officers Net increase each. From 2004 to 2008, the number of full-time sworn personnel per 100,000 U.S. residents increased from 250 to 251. HIGHLIGHTS State and local law enforcement agencies employed From 2004 to 2008, state and local law enforcement about 1,133,000 persons on a full-time basis in 2008, agencies added about 9,500 more full-time sworn including 765,000 sworn personnel. -

School Safety Enforcement Program Awards
School Safety Enforcement Program Awards Jurisdiction Agency Award Allegany County Allegany County Sheriff's Office $5,000.00 Allegany County Maryland State Police – Cumberland Barrack $9,000.00 Allegany County Cumberland Police Department $24,880.00 Allegany County Frostburg City Police Department $2,000.00 Anne Arundel County Anne Arundel County Police Department $16,000.00 Headquarters Anne Arundel County Annapolis City Police Department $11,400.00 Baltimore County Baltimore County Police Department $35,000.00 Calvert County Calvert County Sheriff's Office $8,000.00 Calvert County Maryland State Police – Prince Frederick Barrack $12,000.00 Caroline County Caroline County Sheriff's Office $3,000.00 Carroll County Westminster Police Department $5,000.00 Carroll County Sykesville Police Department $1,500.00 Carroll County Hampstead Police Department $10,000.00 Carroll County Carroll County Sheriff's Office $12,100.00 Carroll County Maryland State Police – Westminster Barrack $12,000.00 Cecil County Cecil County Sheriff's Office Law Enforcement $3,000.00 Facility Cecil County Maryland State Police – North East Barrack $13,500.00 Charles County Maryland State Police – La Plata Barrack $7,000.00 Charles County Charles County Sheriff's Office $16,000.00 Dorchester County Dorchester County Sheriff's Office $26,000.00 Dorchester County Cambridge Police Department $9,500.00 Frederick County Frederick City Police Department $17,000.00 Frederick County Maryland State Police – Frederick Barrack $10,000.00 Garrett County Oakland Police Department