Recognizing When a Child's Injury Or Illness Is Caused by Abuse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Section 9 Patient Care Record Documentation Guidelines
SECTION 9 PATIENT CARE RECORD DOCUMENTATION GUIDELINES Quick Reference Introduction to Patient Care Record Documentation 9-2 When to complete a Patient Care Record 9-3 Why use a patient Record 9-3 How to complete a Patient Record 9-3 Approaches to Documentation: System by System 9-4 Body Region 9-5 Gathering information using CHART format (System by System) 9-5 Gathering information using CHART format (Body Region) 9-6 Narrative using CHART format 9-7 Gathering information using SOAP format (System by System) 9-8 9-8 Gathering information using SOAP format (Body Region) 9-9 Narrative using SOAP format Illness and Injury Reference for Competency Sign offs 4.3 and 6.1 9-10 Introduction Patient Care Record Documentation Medavie HealthEd recognizes the need for students to provide detailed and accurate Patient Care Record Documentation. It is important for the student, school staff and preceptors to recognize the value of documenting patient care, in that it serves as a safety mechanism for the patient, as well as the practitioner. To that end, students, school staff and preceptors must develop the student‟s ability to document all aspects of the patient care they provide. Documentation provides a written record between practitioners of the assessment and treatment they have provided. This establishes greater patient safety and the smooth transition of patient care from one provider to another. In regard to the student and practitioner, accurate and detailed information on the Patient Care Record will serve as the primary record in any litigation that may be brought forward by a patient or their family. -
Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -

Nasolabial and Forehead Flap Reconstruction of Contiguous Alar
Journal of Plastic, Reconstructive & Aesthetic Surgery (2017) 70, 330e335 Nasolabial and forehead flap reconstruction of contiguous alareupper lip defects Jonathan A. Zelken a,b, Sashank K. Reddy c, Chun-Shin Chang a, Shiow-Shuh Chuang a, Cheng-Jen Chang a, Hung-Chang Chen a, Yen-Chang Hsiao a,* a Department of Plastic and Reconstructive Surgery, Chang Gung Memorial Hospital, College of Medicine, Chang Gung University, Taipei, Taiwan b Department of Plastic and Reconstructive Surgery, Breastlink Medical Group, Laguna Hills, CA, USA c Department of Plastic and Reconstructive Surgery, Johns Hopkins Hospital, Baltimore, MD, USA Received 4 May 2016; accepted 31 October 2016 KEYWORDS Summary Background: Defects of the nasal ala and upper lip aesthetic subunits can be Nasal reconstruction; challenging to reconstruct when they occur in isolation. When defects incorporate both Nasolabial flap; the subunits, the challenge is compounded as subunit boundaries also require reconstruc- Rhinoplasty; tion, and local soft tissue reservoirs alone may provide inadequate coverage. In such cases, Forehead flap we used nasolabial flaps for upper lip reconstructionandaforeheadflapforalarrecon- struction. Methods: Three men and three women aged 21e79 years (average, 55 years) were treated for defects of the nasal ala and upper lip that resulted from cancer (n Z 4) and trauma (n Z 2). Unaffected contralateral subunits dictated the flap design. The upper lip subunit was excised and replaced with a nasolabial flap. The flap, depending on the contralateral reference, determined accurate alar base position. A forehead flap resurfaced or replaced the nasal ala. Autologous cartilage was used in every case to fortify the forehead flap reconstruction. Results: Patients were followed for 25.6 months (range, 1e4 years). -
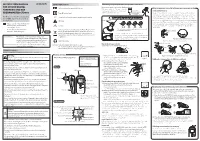
Instruction Manual for Citizen Digital Forehead And
INSTRUCTION MANUAL Symbol Explanations Measuring body temperature (temperature detection) Remove the probe cap and check the probe tip. FOR CITIZEN DIGITAL Refer to instruction manual before use. How to measure correctly in the ear measurement mode * When using it for the first time, open the FOREHEAD AND EAR battery cap and remove the insulation Open the Temperature basics battery cap to THERMOMETER CTD710 Type BF applied part sheet under the battery cap. remove the All objects radiate heat. This device consists of a probe with a built-in insulation sheet. infrared sensor that measures body temperature by detecting the heat Thank you very much for purchasing IP22 Classification for water ingress and particulate matter. radiated by the eardrum and surrounding tissue. Figure 4 shows the the CITIZEN digital forehead and ear Keeping the probe window clean tortuous anatomy of a normal ear canal. As shown in Figure 5, hold the thermometer. Warning Probe window ear and gently pull it back at an angle or pull it straight back to straighten out the ear canal. The shape of the ear canal differs from individual, check • Please read all of the information in before measurement. Accurate temperature measurements make it this instruction manual before Caution essential to straighten the ear canal so that the probe tip directly faces operating the device. the eardrum. • Be sure to have this instruction Indicates this device is subject to the Waste Electrical and Dirt in the probe window will impact the accuracy of temperature detection. External auditory manual to hand during use. 1902LA Electronic Equipment Directive in the European Union. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -

Ear and Forehead Thermometer
Ear and Forehead Thermometer INSTRUCTION MANUAL Item No. 91807 19.PJN174-14_GA-USA_HHD-Ohrthermometer_DSO364_28.07.14 Montag, 28. Juli 2014 14:37:38 USAD TABLE OF CONTENTS No. Topic Page 1.0 Definition of symbols 5 2.0 Application and functionality 6 2.1 Intended use 6 2.2 Field of application 7 3.0 Safety instructions 7 3.1 General safety instructions 7 3.3 Environment for which the DSO 364 device is not suited 9 3.4 Usage by children and adolescents 10 3.5 Information on the application of the device 10 4.0 Questions concerning body temperature 13 4.1 What is body temperature? 13 4.2 Advantages of measuring the body tempera- ture in the ear 14 4.3 Information on measuring the body tempera- ture in the ear 15 5.0 Scope of delivery / contents 16 6.0 Designation of device parts 17 7.0 LCD display 18 8.0 Basic functions 19 8.1 Commissioning of the device 19 8.2 Warning indicator if the body temperature is 21 too high 2 19.PJN174-14_GA-USA_HHD-Ohrthermometer_DSO364_28.07.14 Montag, 28. Juli 2014 14:37:38 TABLE OF CONTENTS USA No. Topic Page 8.3 Backlighting / torch function 21 8.4 Energy saving mode 22 8.5 Setting °Celsius / °Fahrenheit 22 9.0 Display / setting time and date 23 9.1 Display of time and date 23 9.2 Setting time and date 23 10.0 Memory mode 26 11.0 Measuring the temperature in the ear 28 12.0 Measuring the temperature on the forehead 30 13.0 Object temperature measurement 32 14.0 Disposal of the device 33 15.0 Battery change and information concerning batteries 33 16.0 Cleaning and care 36 17.0 “Cleaning” warning indicator 37 18.0 Calibration 38 19.0 Malfunctions 39 20.0 Technical specification 41 21.0 Warranty 44 3 19.PJN174-14_GA-USA_HHD-Ohrthermometer_DSO364_28.07.14 Montag, 28. -
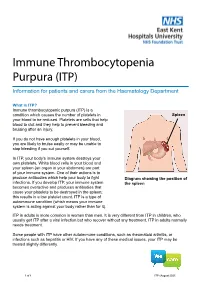
Immune Thrombocytopenia Purpura (ITP)
Immune Thrombocytopenia Purpura (ITP) Information for patients and carers from the Haematology Department What is ITP? Immune thrombocytopenic purpura (ITP) is a condition which causes the number of platelets in Spleen your blood to be reduced. Platelets are cells that help blood to clot and they help to prevent bleeding and bruising after an injury. If you do not have enough platelets in your blood, you are likely to bruise easily or may be unable to stop bleeding if you cut yourself. In ITP, your body’s immune system destroys your own platelets. White blood cells in your blood and your spleen (an organ in your abdomen) are part of your immune system. One of their actions is to produce antibodies which help your body to fight Diagram showing the position of infections. If you develop ITP, your immune system the spleen becomes overactive and produces antibodies that cause your platelets to be destroyed in the spleen; this results in a low platelet count. ITP is a type of autoimmune condition (which means your immune system is acting against your body rather than for it). ITP in adults is more common in women than men. It is very different from ITP in children, who usually get ITP after a viral infection but who recover without any treatment. ITP in adults normally needs treatment. Some people with ITP have other autoimmune conditions, such as rheumatoid arthritis, or infections such as hepatitis or HIV. If you have any of these medical issues, your ITP may be treated slightly differently. 1 of 8 ITP (August 2021) A normal platelet count is between 150 and 400 thousand million platelets per litre of blood. -

Clinical Update and Treatment of Lactation Insufficiency
Review Article Maternal Health CLINICAL UPDATE AND TREATMENT OF LACTATION INSUFFICIENCY ARSHIYA SULTANA* KHALEEQ UR RAHMAN** MANJULA S MS*** SUMMARY: Lactation is beneficial to mother’s health as well as provides specific nourishments, growth, and development to the baby. Hence, it is a nature’s precious gift for the infant; however, lactation insufficiency is one of the explanations mentioned most often by women throughout the world for the early discontinuation of breast- feeding and/or for the introduction of supplementary bottles. Globally, lactation insufficiency is a public health concern, as the use of breast milk substitutes increases the risk of morbidity and mortality among infants in developing countries, and these supplements are the most common cause of malnutrition. The incidence has been estimated to range from 23% to 63% during the first 4 months after delivery. The present article provides a literary search in English language of incidence, etiopathogensis, pathophysiology, clinical features, diagnosis, and current update on treatment of lactation insufficiency from different sources such as reference books, Medline, Pubmed, other Web sites, etc. Non-breast-fed infant are 14 times more likely to die due to diarrhea, 3 times more likely to die of respiratory infection, and twice as likely to die of other infections than an exclusively breast-fed child. Therefore, lactation insufficiency should be tackled in appropriate manner. Key words : Lactation insufficiency, lactation, galactagogue, breast-feeding INTRODUCTION Breast-feeding is advised becasue human milk is The synonyms of lactation insufficiency are as follows: species-specific nourishment for the baby, produces lactational inadequacy (1), breast milk insufficiency (2), optimum growth and development, and provides substantial lactation failure (3,4), mothers milk insufficiency (MMI) (2), protection from illness. -

SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment
Organizational Principles to Guide and Define the Child Health Care System and/or Improve the Health of all Children POLICY STATEMENT SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment TASK FORCE ON SUDDEN INFANT DEATH SYNDROME abstract KEY WORDS Despite a major decrease in the incidence of sudden infant death syn- SIDS, sudden infant death, infant mortality, sleep position, bed- sharing, tobacco, pacifier, immunization, bedding, sleep surface drome (SIDS) since the American Academy of Pediatrics (AAP) released ABBREVIATIONS its recommendation in 1992 that infants be placed for sleep in a non- SIDS—sudden infant death syndrome prone position, this decline has plateaued in recent years. Concur- SUID—sudden unexpected infant death rently, other causes of sudden unexpected infant death that occur AAP—American Academy of Pediatrics during sleep (sleep-related deaths), including suffocation, asphyxia, This document is copyrighted and is property of the American and entrapment, and ill-defined or unspecified causes of death have Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American increased in incidence, particularly since the AAP published its last Academy of Pediatrics. Any conflicts have been resolved through statement on SIDS in 2005. It has become increasingly important to a process approved by the Board of Directors. The American address these other causes of sleep-related infant death. Many of the Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of modifiable and nonmodifiable risk factors for SIDS and suffocation are this publication. -

Definitions of Child Abuse and Neglect
STATE STATUTES Current Through March 2019 WHAT’S INSIDE Defining child abuse or Definitions of Child neglect in State law Abuse and Neglect Standards for reporting Child abuse and neglect are defined by Federal Persons responsible for the child and State laws. At the State level, child abuse and neglect may be defined in both civil and criminal Exceptions statutes. This publication presents civil definitions that determine the grounds for intervention by Summaries of State laws State child protective agencies.1 At the Federal level, the Child Abuse Prevention and Treatment To find statute information for a Act (CAPTA) has defined child abuse and neglect particular State, as "any recent act or failure to act on the part go to of a parent or caregiver that results in death, https://www.childwelfare. serious physical or emotional harm, sexual abuse, gov/topics/systemwide/ or exploitation, or an act or failure to act that laws-policies/state/. presents an imminent risk of serious harm."2 1 States also may define child abuse and neglect in criminal statutes. These definitions provide the grounds for the arrest and prosecution of the offenders. 2 CAPTA Reauthorization Act of 2010 (P.L. 111-320), 42 U.S.C. § 5101, Note (§ 3). Children’s Bureau/ACYF/ACF/HHS 800.394.3366 | Email: [email protected] | https://www.childwelfare.gov Definitions of Child Abuse and Neglect https://www.childwelfare.gov CAPTA defines sexual abuse as follows: and neglect in statute.5 States recognize the different types of abuse in their definitions, including physical abuse, The employment, use, persuasion, inducement, neglect, sexual abuse, and emotional abuse. -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

Bleeds and Bruises in Children with Haemophilia
Bleeds and Bruises in CHildren WiTH HaeMOPHilia MusCle ANd/or JoiNt Bleeds Call the parent/guardian P.r.i.C.e. siGNs oF A serious HeAd Bleed P : Protection * Headache. Lower Limb: Take weight off the joint or muscle * drowsiness. Upper Limb: No carrying using affected arm * Nausea. r : rest * Vomiting. • Rest means rest! * unsteady Balance. • Try not to allow use of the joint or muscle where * irritability. possible. * Confusion. * seizures. i : ice * loss of consciousness. • Regular ice packs can help with pain & reduce swelling. • Put an ice pack over the affected area for 20 minutes. Repeat every two hours. DO NOT leave the ice pack on for more than 20 minutes siGNs oF A soFt tissue DO NOT place ice pack directly on skin (Use a tea Bleed towel/cold pack cover) * Bruising, discolouring of skin. C : Compression * Mild swelling. • Use an elasticated bandage to compress the affected area to reduce swelling. e : elevation • Elevate the affected limb to help reduce swelling. siGNs oF AN ABdoMiNAl • Keep the affected joint or muscle above the level of the Bleed heart. * Bloody, black or tar-like First Aid bowel motions. * red or brown urine. Mouth & Gum Bleeds * Pain. These can be hard to control because clots that form are * Vomiting of blood (blood washed away by saliva or knocked off by the tongue or food. Try giving the child an ice cube or ice pop to suck. may be red or black). These bleeds may need treatment by parents or the treatment centre. Nosebleeds siGNs oF BleediNG iNto tHe Tilt head forward and pinch the bridge of the nose below the bone for 10 - 20 minutes and / or put an ice-pack on JoiNts or MusCles the bridge of the nose for not more than 5 minutes.