Surgical Technique and Its Application in Neurenteric Cysts of the Cervicomedullary Junction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -

A Case Report of an Enlarged Suboccipital Nerve with Cutaneous Branch
Open Access Case Report DOI: 10.7759/cureus.2933 A Case Report of an Enlarged Suboccipital Nerve with Cutaneous Branch Sasha Lake 1 , Joe Iwanaga 2 , Rod J. Oskouian 3 , Marios Loukas 4 , R. Shane Tubbs 5 1. Anatomical Studies, St. George's, St. George, GRD 2. Medical Education and Simulation, Seattle Science Foundation, Seattle, USA 3. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 4. Anatomical Sciences, St. George's University, St. George's, GRD 5. Neurosurgery, Seattle Science Foundation, Seattle, USA Corresponding author: Joe Iwanaga, [email protected] Abstract Variations of the suboccipital nerve are infrequently reported. This nerve derived from the C1 spinal nerve is usually a small branch that primarily innervates the short suboccipital muscles. During the routine dissection of the occipital region in an adult cadaver, a vastly enlarged left-sided suboccipital nerve was identified. The nerve innervated the short suboccipital muscles and overlying semispinalis capitis in normal fashion. However, it continued cranially to end in the overlying skin of the occiput. Although not normally thought to have a cutaneous branch, recalcitrant occipital neuralgia might be due to such a variant branch. Future studies are necessary to further elucidate this proposed pathomechanism. Categories: Neurology, Pathology Keywords: suboccipital nerve, c1 nerve, occiput cutaneous innervation, sensory suboccipital nerve Introduction The suboccipital nerve is the dorsal ramus of C1. This nerve is found between the skull and atlas and within the suboccipital triangle. Here, it is positioned between the posterior arch of the atlas and vertebral artery bordering the nerve inferiorly and superiorly, respectively [1]. The suboccipital nerve innervates the rectus capitis posterior major and minor, obliquus capitis superior, obliquus capitis inferior, and semispinalis capitis. -

Abdominal Wall and Cavity
Abdominal Wall and Cavity Dr. ALSHIKH YOUSSEF Haiyan BOUNDARIES Bony Landmarks around Abdomen Iliac crest • Anterior superior iliac • spine (ASIS) Pubic crest • Inguinal ligament • Costal margin • Xiphoid process • Body Cavities Abdominopelvic Cavity Abdominal Cavity – Pelvic Cavity – P242-fig.4.21 Abdominal wall Muscle Aponeurosis DIVISIONS Abdominal Quadrants Applied Anatomy Abdomen is divided into 9 regions via four • planes: Two horizontal [sub-costal (10th) and trans – tubercules plane] (L5). Two vertical (midclavicular planes). – They help in localization of abdominal signs • and symptoms Abdomen Boundaries 9 regions hypochondrium epigastric region subcostal plane flank umbilical region transtubercular plane groin pubic region midclavicular line P243-fig.4.23 Abdominal wall Anterolateral abdominal wall Posterior abdominal wall Anterolateral abdominal wall Layers ( from superficial to deep) Skin • Superficial fascia • Anterolateral muscles • Transverse fascia • Extraperitoneal fascia • Parietal peritoneum • Superficial fascia Camper’s fascia • Scarpa's fascia • Anterolateral abdominal wall Superficial fascia : -division below umbilicus = Fatty layer (Camper’s fascia) continuous • with the superficial fascia over the rest of the ) Thigh –thorax (body. = Membranous layer (Scarpa’s fascia) • passes over the inguinal ligament to fuse the deep fascia of the thigh (fascia lata) approximately one fingerbreadth below the inguinal ligament. In the midline, it is not attached to the pubis but instead from a tubular sheath for the penis (clitoris). In the perineum, it is attaches on each side to the margins of the pubic arch and is know as Colles’ fascia. deep fascia : thin layer covering abdominal • musceles . Arteries 5 intercostal arteries • subcostal arteries • 4 lumbar arteries • Superior epigastric artery— • internal thoracic artery Inferior epigastric artery - • external iliac artery Deep iliac circumflex artery- • external iliac artery SUPERFICIAL ARTERIES Lateral • Posterior intercostal a. -

Bilateral Variation of the Suboccipital Region Musculature
S Journal of O p s e s n Acce Anatomy and Physiological Studies CASE REPORT Bilateral Variation of the Suboccipital Region Musculature AR Dickerson*, CL Fisher PhD Center for Anatomical Sciences, University of North Texas Health Science Center, Fort Worth, Texas, USA Abstract Dissection of the posterior cervical and suboccipital regions of an embalmed 81-year-old male cadaver revealed bilateral variations in the muscular anatomy, including two accessory muscles lying deep to the semispinalis capitis on each side, as well as a bilateral doubling of the rectus capitis posterior major muscle. These two sets of anatomical variations have little to no previous documentation in the literature. The accessory muscle bands were observed to have unique relationships with the greater occipital nerve on each side. This case report describes the findings in detail and examines their precedent in the literature. The suboccipital region has been implicated in the etiology of cervicogenic pain, headaches, and occipital neuralgia. Variations in the muscular anatomy have the potential to create structural interactions with vascular and neurologic structures in the area. Anatomic variations like those reported here should be considered in the diagnosis and treatment of pain and other conditions of the suboccipital region. Keywords: Anatomic Variation, Suboccipital, Accessory Muscle, Greater Occipital Nerve, Rectus capitis posterior major muscle Background leading us to believe that we had encountered accessory muscles that had been previously unreported. The muscles This case report describes variation of the musculature in the were delicate and located in a region often removed to expose suboccipital region observed during dissection of an embalmed the suboccipital region just beneath, so we postulate that the 81-year-old male cadaver. -

Appleton & Lange Review of Anatomy
0523-00 FM 07/15/02 15:30 Page i Sixth edition APPLETON & LANGE REVIEW OF ANATOMY Royce Lee Montgomery, PhD Professor Department of Cell and Developmental Biology School of Medicine University of North Carolina Chapel Hill, North Carolina Kurt Ogden Gilliland, PhD Department of Cell and Developmental Biology School of Medicine University of North Carolina Chapel Hill, North Carolina Appleton & Lange Reviews/McGraw-Hill Medical Publishing Division New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto 0523-00 FM 07/15/02 15:30 Page ii Appleton & Lange Review of Anatomy, Sixth Edition Copyright © 2003 by The McGraw-Hill Companies, Inc. All rights reserved. Printed in the United States of America. Except as permitted under the United States Copyright Act of 1976, no part of this publication may be reproduced or distributed in any form or by any means, or stored in a data base or retrieval system, without the prior written permission of the publisher. Previous editions copyright © 1995, 1989, by Appleton & Lange; copyright © 1982, 1978, 1974, by Arco Publishing, Inc. 1 2 3 4 5 6 7 8 9 0 VNH VNH 0 9 8 7 6 5 4 3 2 ISBN: 0-07-137727-1 Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the stan- dards accepted at the time of publication. -

The Suboccipital Cavernous Sinus
The suboccipital cavernous sinus Kenan I. Arnautovic, M.D., Ossama Al-Mefty, M.D., T. Glenn Pait, M.D., Ali F. Krisht, M.D., and Muhammad M. Husain, M.D. Departments of Neurosurgery and Pathology, University of Arkansas for Medical Sciences, and Laboratory Service, Veterans Administration Medical Center, Little Rock, Arkansas The authors studied the microsurgical anatomy of the suboccipital region, concentrating on the third segment (V3) of the vertebral artery (VA), which extends from the transverse foramen of the axis to the dural penetration of the VA, paying particular attention to its loops, branches, supporting fibrous rings, adjacent nerves, and surrounding venous structures. Ten cadaver heads (20 sides) were fixed in formalin, their blood vessels were perfused with colored silicone rubber, and they were dissected under magnification. The authors subdivided the V3 into two parts, the horizontal (V3h) and the vertical (V3v), and studied the anatomical structures topographically, from the superficial to the deep tissues. In two additional specimens, serial histological sections were acquired through the V3 and its encircling elements to elucidate their cross-sectional anatomy. Measurements of surgically and clinically important features were obtained with the aid of an operating microscope. This study reveals an astonishing anatomical resemblance between the suboccipital complex and the cavernous sinus, as follows: venous cushioning; anatomical properties of the V3 and those of the petrouscavernous internal carotid artery (ICA), namely their loops, branches, supporting fibrous rings, and periarterial autonomic neural plexus; adjacent nerves; and skull base locations. Likewise, a review of the literature showed a related embryological development and functional and pathological features, as well as similar transitional patterns in the arterial walls of the V3 and the petrous-cavernous ICA. -

Anatomy Anatomy
ANATOMY ANATOMY NECK AREAS BONES ORGANS MUSCLES NERVES VESSELS OTHER •Anterior •Cervical •Pharynx •Suboccipital •Phrenic •Arterial •Fascial Triangle Spine •Larynx •Suprahyoids Nerve Supply Layers •Posterior •Hyoid Bone •Oesophagus •Infrahyoids •Cervical •Venous Triangle •Thyroid •Scalenes Plexus Drainage Gland •Lymphatics •Parathyroid Glands Neck NECK MUSCLES • SUBOCCIPITAL • SUPRAHYOIDS • INFRAHYOIDS • SCALENES SUBOCCIPITAL GROUP Contents 1 Rectus Capitis Posterior Major MUSCLES OF 2 Rectus Capitis Posterior Minor 3 Obliquus Capitis Inferior THE NECK 4 Obliquus Capitis Superior 5 Suboccipital Triangle • The suboccipital muscles are a group of four muscles situated underneath the occipital bone. All the muscles in this group are innervated by the suboccipital nerve. • They are located within the suboccipital compartment of the neck; deep to the Suboccipital sternocleidomastoid, trapezius, splenius and semispinalis muscles. They collectively act to extend and Group of rotate the head. Muscle • In this article, we shall look at the anatomy of the suboccipital muscles – their attachments, actions and innervation. Rectus Capitis Posterior Major • The rectus capitis posterior major is the larger of the rectus capitis muscles. It is located laterally to the rectus capitis posterior minor. Suboccipital • Attachments: Originates from the spinous process of the C2 vertebrae (axis), and inserts into the lateral part of Group of the inferior nuchal line of the occipital bone. Muscle • Actions: Extension and rotation of the head. • Innervation: Suboccipital nerve (posterior ramus of C1). Rectus Capitis Posterior Major Rectus Capitis Posterior Minor • The rectus capitis posterior minor is the most medial of the suboccipital muscles. There is a connective tissue bridge between this muscle and the dura mater (outer membrane of the meninges) – which may play a role in cervicogenic headaches. -
Cervical Anatomy Overview: Building the Cervical Spine • Atlas •Axis • Ligaments • Muscles •Fascia • the Vert • and How to Apply to Common Cases Atlas
MastoidC4-5C3C4 body facet process joint Cervical anatomy Overview: building the cervical spine • Atlas •axis • ligaments • muscles •fascia • the vert • And how to apply to common cases Atlas • Ring of bone • Lateral mass on each side • Transverse process • Superior projects medially and inferior articular facet projects medially to C2 superior artic facet • 3 cm canal Axis 1 Spinous Process 2. Lamina 3. Transverse Process 4. Pedicle 5. Superior Articular Surface 6. Odontoid Process (Dens) 7. Body 9. Inferior Articular Surface Atlanto-Occipital Joint • Allows flexion and extension and slight side to side motion • almost NO rotation • Stability dependent on ligaments: ALL, attaches to tubercle on axis, then small contin to skull apical ligament tectorial membrane (broad ligamentous sheet) (continuation of PLL) cruciate ligament --formed by rostral and caudal longitudinal bands Alar ligaments arise from dens, connect to medial occipital condyle limit rotation of AO joint dorsal atlanto-occipital membrane (continuation of Ligamentum flavum), --remember overlays vert, C1 C1 and C2 nerves pass dorsally to occipitocervical and C1/2 joint capsules, NOT ventral to facets UNLIKE other cervical vertebrae Draw C1, 2 ligaments (coronal view) A- apical B- alar C-cruciform D-tectoral Draw C1, 2 ligaments (sagittal view) A- apical B- anterior alantooccipital C-cruciform D-tectorial membrane (PLL) Movements allowed in the craniocervical region Range of Joint Motion motion (degrees) Occiput–C1 Combined flexion/extension 25 Lateral bending (unilateral) 5 Axial rotation (unilateral) 5 C1–C2 Combined flexion/extension 20 Lateral bending (unilateral) 5 Axial rotation (unilateral) 40 VOLUME 60 | NUMBER 1 | JANUARY 2007 SUPPLEMENT Surface anatomy of neck Neck triangles • Anterior triangle – 4 triangles: 1. -

Immersive Surgical Anatomy of the Craniocervical Junction
Open Access Technical Report DOI: 10.7759/cureus.10364 Immersive Surgical Anatomy of the Craniocervical Junction Vera Vigo 1 , Ankit Hirpara 1 , Mohamed Yassin 1 , Minghao Wang 2 , Dean Chou 3 , Pasquale De Bonis 4 , Adib Abla 1 , Roberto Rodriguez Rubio 1 1. Neurological Surgery, University of California San Francisco, San Francisco, USA 2. Neurological Surgery, First Affiliated Hospital of China Medical University, Shenyang, CHN 3. Neurological Surgery, University of Caifornia San Francisco, San Francisco, USA 4. Neurological Surgery, Ferrara University Hospital, Ferrara, ITA Corresponding author: Roberto Rodriguez Rubio, [email protected] Abstract With the advent and increased usage of posterior, lateral, and anterior surgical approaches to the craniocervical junction (CCJ), it is essential to have a sound understanding of the osseous, ligamentous, and neurovascular layers of this region as well as their three-dimensional (3D) orientations and functional kinematics. Advances in 3D technology can be leveraged to develop a more nuanced and comprehensive understanding of the CCJ, classically depicted via dissections and sketches. As such, this study aims to illustrate - with the use of 3D technologies - the major anatomical landmarks of the CCJ in an innovative and informative way. Photogrammetry, structured light scanning, and 3D reconstruction of medical images were used to generate these high-resolution volumetric models. A clear knowledge of the critical anatomical structures and morphometrics of the CCJ is crucial for the diagnosis, classification, and treatment of pathologies in this transitional region. Categories: Neurosurgery, Orthopedics, Anatomy Keywords: craniocervical junction, atlas, axis, occipital bone, biomechanics, cruciform ligament, volumetric model, neuroanatomy, surgical lines Introduction The craniocervical junction (CCJ) is a complex transitional region between the base of the skull and the upper cervical spine [1]. -
Dry Lab-Weyrich
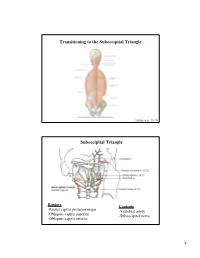
Transitioning to the Suboccipital Triangle Syllabus p. 14-15 Suboccipital Triangle Borders Contents -Rectus capitis posterior major -Vertebral artery -Obliquus capitis superior -Suboccipital nerve -Obliquus capitis inferior 1 Innervation of the Suboccipital Region Suboccipital (C1) – innervates suboccipital muscles Greater occipital (C2) – supplies posterior scalp C3 – supplies small area of lower scalp Blood Supply to the Suboccipital Region Occipital artery 2 A 29 year old man suffers from a stroke. A dissecting vertebral artery contributed to his stroke. This may in part be due to the course of the vertebral artery as it approaches the suboccipital triangle, which is bordered by the following muscles: 100% A. Obliquus capitis superior, Obliquus capitis inferior, rectus capitis minor B. Obliquus capitis superior, rectus capitis minor, rectus capitis major C. Obliquus capitis superior, Obliquus capitis inferior, rectus capitis major D. Obliquus capitis superior, semispinalis cervicus, rectus capitis major 0% 0% 0% 0% E. Obliquus capitis inferior, rectus capitis minor, rectus capitis major A. Obliquus B. capitis Obliquus s... Obliquus capitis s... capitis Obliquus supe... capitis Obliquus supe... capitis inferio.. Osteology • Back -Gray’s pp. 26-47 -Gray’s dissector, pp. 3-9 3 Osteologic Landmarks (Back) Scapula (posterior) 4 The Vertebral Column Normal Curvatures of the Vertebral Column 5 Abnormal Curvatures of the Vertebral Column A 42 year old male goes running for one hour and subsequently complains of lower back pain and disoriented equilibrium. After a superficial examination of the back, you conclude that the runner is suffering from one of the following: 100% A. Lordosis B. Scoliosis C. Right side winged scapula D. -

Evaluation of the Greater Occipital Nerve Location Regarding Its Relation to Intermastoid and External Occipital Protuberance to Mastoid Process Lines T
Folia Morphol. Vol. 80, No. 3, pp. 533–541 DOI: 10.5603/FM.a2020.0099 O R I G I N A L A R T I C L E Copyright © 2021 Via Medica ISSN 0015–5659 eISSN 1644–3284 journals.viamedica.pl Evaluation of the greater occipital nerve location regarding its relation to intermastoid and external occipital protuberance to mastoid process lines T. Huanmanop1, I. Issara2, S. Agthong1, V. Chentanez1 1Department of Anatomy, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand 2Medical Science Programme, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand [Received: 22 June 2020; Accepted: 7 August 2020; Early publication date: 22 August 2020] Background: Localisation of the greater occipital nerve (GON) is essential for the achievement of several procedures performed in the occipital region especially the treatment of occipital neuralgia. This study proposed to investigate the location of GON subcutaneous (Sc) and semispinalis capitis (SSC) piercing points related to the intermastoid and external occipital protuberance (EOP) to mastoid process (MP) lines. Materials and methods: The Sc piercing point, relation to SSC and obliquus capitis inferior (OCI) muscles of 100 GONs from 50 cadaveric heads (23 males, 27 females) were dissected. Distances from EOP to MP (EM line) on both sides and between MPs (MM line) were measured. Perpendicular lines from Sc and SSC piercing points to EM and MM lines were created and measured. Distances from EOP to the perpendicular lines of SSC piercing point and from MP to the perpendicular lines of Sc piercing point were measured and calculated into percentage of EM and MM length, respectively. -

Landmarks for the Identification of the Cutaneous Nerves of the Occiput
Clinical Anatomy 20:235–238 (2007) ORIGINAL COMMUNICATION Landmarks for the Identification of the Cutaneous Nerves of the Occiput and Nuchal Regions R. SHANE TUBBS,* E. GEORGE SALTER, JOHN C. WELLONS III, JEFFREY P. BLOUNT, AND W. JERRY OAKES Pediatric Neurosurgery, Children’s Hospital, Birmingham, Alabama Although surgical procedures are often performed over the posterior head and neck, surgical landmarks for avoiding the cutaneous nerves in this region are surprisingly lacking in the literature. Twelve adult cadaveric specimens under- went dissection of the cutaneous nerves overlying the posterior head and neck, and mensuration was made between these structures and easily identifi- able surrounding bony landmarks. All specimens were found to have a third occipital nerve (TON), lesser occipital nerve (LON), and greater occipital nerve (GON), and we found that the TON was, on average, 3 mm lateral to the external occipital protuberance (EOP). Small branches were found to cross the midline and communicate with the contralateral TON inferior to the EOP in the majority of sides. The mean diameter of the main TON trunk was 1.3 mm. This trunk became subcutaneous at a mean of 6 cm inferior to the EOP. The GON was found to lie at a mean distance of 4 cm lateral to the EOP. On all but three sides, a small medial branch was found that ran medially from the GON to the TON *1 cm superior to a horizontal line drawn through the EOP. The GON was found to pierce the semispinalis capitis muscle on average 2 cm superior to the intermastoid line. The mean diameter of the GON was 3.5 mm.