International Journal of Current Research and Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Poxviruses: Smallpox Vaccine, Its Complications and Chemotherapy
Virus Adaptation and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article R E V IEW Poxviruses: smallpox vaccine, its complications and chemotherapy Mimi Remichkova Abstract: The threat of bioterrorism in the recent years has once again posed to mankind the unresolved problems of contagious diseases, well forgotten in the past. Smallpox (variola) is Department of Pathogenic Bacteria, The Stephan Angeloff Institute among the most dangerous and highly contagious viral infections affecting humans. The last of Microbiology, Bulgarian Academy natural case in Somalia marked the end of a successful World Health Organization campaign of Sciences, Sofia, Bulgaria for smallpox eradication by vaccination on worldwide scale. Smallpox virus still exists today in some laboratories, specially designated for that purpose. The contemporary response in the treatment of the post-vaccine complications, which would occur upon enforcing new programs for mass-scale smallpox immunization, includes application of effective chemotherapeutics and their combinations. The goals are to provide the highest possible level of protection and safety of For personal use only. the population in case of eventual terrorist attack. This review describes the characteristic features of the poxviruses, smallpox vaccination, its adverse reactions, and poxvirus chemotherapy. Keywords: poxvirus, smallpox vaccine, post vaccine complications, inhibitors Characteristics of poxviruses Smallpox (variola) infection is caused by the smallpox virus. This virus belongs to the genus of Orthopoxvirus included in the Poxviridae family. Poxviruses are one of the largest and most complexly structured viruses, known so far. The genome of poxviruses consists of a linear two-chained DNA and its replication takes place in the cytoplasm of the infected cell. -

Old Woman Creek National Estuarine Research Reserve Management Plan 2011-2016
Old Woman Creek National Estuarine Research Reserve Management Plan 2011-2016 April 1981 Revised, May 1982 2nd revision, April 1983 3rd revision, December 1999 4th revision, May 2011 Prepared for U.S. Department of Commerce Ohio Department of Natural Resources National Oceanic and Atmospheric Administration Division of Wildlife Office of Ocean and Coastal Resource Management 2045 Morse Road, Bldg. G Estuarine Reserves Division Columbus, Ohio 1305 East West Highway 43229-6693 Silver Spring, MD 20910 This management plan has been developed in accordance with NOAA regulations, including all provisions for public involvement. It is consistent with the congressional intent of Section 315 of the Coastal Zone Management Act of 1972, as amended, and the provisions of the Ohio Coastal Management Program. OWC NERR Management Plan, 2011 - 2016 Acknowledgements This management plan was prepared by the staff and Advisory Council of the Old Woman Creek National Estuarine Research Reserve (OWC NERR), in collaboration with the Ohio Department of Natural Resources-Division of Wildlife. Participants in the planning process included: Manager, Frank Lopez; Research Coordinator, Dr. David Klarer; Coastal Training Program Coordinator, Heather Elmer; Education Coordinator, Ann Keefe; Education Specialist Phoebe Van Zoest; and Office Assistant, Gloria Pasterak. Other Reserve staff including Dick Boyer and Marje Bernhardt contributed their expertise to numerous planning meetings. The Reserve is grateful for the input and recommendations provided by members of the Old Woman Creek NERR Advisory Council. The Reserve is appreciative of the review, guidance, and council of Division of Wildlife Executive Administrator Dave Scott and the mapping expertise of Keith Lott and the late Steve Barry. -

Blister Beetles in Alfalfa Circular 536 Revised by Jane Breen Pierce1
Blister Beetles in Alfalfa Circular 536 Revised by Jane Breen Pierce1 Cooperative Extension Service • College of Agricultural, Consumer and Environmental Sciences This publication provides information on the veterinary Table 1. Estimated Number of Beetles for a Lethal and agronomic importance, distinguishing features, (1 mg/kg) Dose of Cantharidin biology, distribution, and control of blister beetles. Beetle Horse Weight (lb) Recommendations for the purchase and use of alfalfa Cantharidin hay by horse owners and other livestock owners are Content (mg) 275 550 1,000 also provided. 1 125 250 455 2 63 125 244 3 41 83 161 VETERINARY SIGNIFICANCE OF BLISTER BEETLES 4 31 63 122 The common name for blister beetles comes from the 5 25 50 97 irritating reaction the beetle’s body fluids cause on ani- Adapted from Campinera et al. (1985) mal skin or delicate membranes. These fluids contain cantharidin, a potent blistering agent that is present in varying amounts in most blister beetle species. Fluids are blistering of the mouth, esophagus, stomach, and blad- released when the beetle is crushed or handled roughly. der. Death can occur 24 hours after a heavy dose. Cantharidin is a stable chemical and a long-term health Laboratory studies have been conducted to determine threat to nearly all livestock (particularly horses) that are the amount of cantharidin contained in various species fed contaminated hay. Storing infested hay does not sig- of blister beetles. Reports on beetles in several genera nificantly reduce the amount of cantharidin in the hay. indicate cantharidin content varying from 1 to 11.3% Research reports indicate cantharidin toxosis can be of their dry weight. -

BLISTER BEETLES in ALFALFA L.Ee Townsend, Extension Entomologist
U N I V E R S I T Y O F K E N T U C K Y COLLEGE OF AGRICULTURE DEPARTMENT OF ENTOMOLOGY ENTFACT-102 BLISTER BEETLES IN ALFALFA L.ee Townsend, Extension Entomologist Several of the common members of this group of Female blister beetles lay clusters of eggs in the soil in beetles contain a chemical that often causes blisters late summer. The small, active larvae that hatch from when applied to the skin; thus the name blister beetles. these eggs crawl over the soil surface entering cracks The substance can be toxic to animals that eat a in search for grasshopper egg pods which are deposited sufficient amount. An understanding of the insects and in the soil. After finding the eggmass, blister beetle their life cycles allows sound management practices to larvae become immobile and spend the rest of their minimize the chances of trapping beetles in hay. It also developmental time as legless grubs. The following gives horse and livestock owners information to summer they transform into the pupal stage and soon consider when making hay purchases. One major emerge in the adult stage. This is why blister beetle factor that increases potential for blister beetle numbers increase dramatically following high problems is crimping hay. This crushes the beetles and grasshopper populations. leaves them in the hay where they can be eaten by animals. The second factor is a large increase in Blister Beetle Toxicity grasshopper numbers. The larval stages of these blister Cantharidin is the poisonous substance in blister beetles develop on grasshopper egg pods in the soil. -

Volume 42, Number 2 June 2015
Wisconsin Entomological Society N e w s I e t t e r Volume 42, Number 2 June 2015 Monitoring and Management - A That is, until volunteer moth surveyor, Steve Sensible Pairing Bransky, came onto the scene. Steve had By Beth Goeppinger, Wisconsin Department done a few moth and butterfly surveys here ofN atural Resources and there on the property. But that changed in 2013. Armed with mercury vapor lights, Richard Bong State Recreation Area is a bait and a Wisconsin scientific collector's heavily used 4,515 acre property in the permit, along with our permission, he began Wisconsin State Park system. It is located in surveying in earnest. western Kenosha County. The area is oak woodland, savanna, wetland, sedge meadow, He chose five sites in woodland, prairie and old field and restored and remnant prairie. savanna habitats. He came out many nights Surveys of many kinds and for many species in the months moths might be flying. After are done on the property-frog and toad, finding that moth populations seemed to drift fence, phenology, plants, ephemeral cycle every 3-5 days, he came out more ponds, upland sandpiper, black tern, frequently. His enthusiasm, dedication and grassland and marsh birds, butterfly, small never-ending energy have wielded some mammal, waterfowl, muskrat and wood surprising results. Those results, in turn, ducks to name a few. Moths, except for the have guided us in our habitat management showy and easy-to-identify species, have practices. been ignored. Of the 4,500 moth species found in the state, Steve has confirmed close to 1,200 on the property, and he isn't done yet! He found one of the biggest populations of the endangered Papaipema silphii moths (Silphium borer) in the state as well as 36 species of Catocola moths (underwings), them. -

Identification of New Cantharidin Derivatives As
IDENTIFICATION OF NEW CANTHARIDIN DERIVATIVES AS NOVEL POTENTIAL INHIBITORS OF PROTEIN PHOSPHATASES 2 AND 5 (PP2A, PP5) Olga Balabon, Dariia Samofalova Life Chemicals Europe GmbH, Leonhardsweg 2, 82008 Unterhaching, Germany. e-mail: [email protected] Cantharidin, a natural compound occurring in medicinal insect blister beetle (Mylabris phalerata Pallas), The docking results showed that three amino acid and its water-soluble demethylated synthetic analog norcantharidin (better known as endothall), residues, Arg275, Asn303, His304, and Arg275, His304, historically used in the purification of phosphorylated proteins, were identified as inhibitors of Arg400 (PP5 and PP2A, respectively) were the most serine-threonine protein phosphatases (PP). Cantharidin (CID 5944, hydrolyzing into cathartic acid important for the ligand binding. In total, nine residues were demonstrated to be involved in the binding - CID 2544) is a potent selective inhibitor of PP2A and PP5 [PMID: 1334551], while of the inhibitors. The completeness of the amino norcantharidin (CID 93004) is a medium-strength inhibitor of PP2A only acid sequence and the profile of the site interaction [PMID:12003183, 23809227]. These compounds have extensively been studied as promising leads in were determined by pairwise and profile alignment with the development of more effective therapeutics for the treatment of cancer, the original sequence (with ClustalX). The binding site neurodegenerative disorders, and type 1 diabetes mellitus. As no highly PP5 selective inhibitors for -
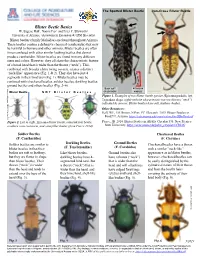
Blister Beetle Basics W
The Spotted Blister Beetle Iron-Cross Blister Beetle Blister Beetle Basics W. Eugene Hall1, Naomi Pier1 and Peter C. Ellsworth2 University of Arizona, 1Assistants in Extension & 2IPM Specialist Blister beetles (family Meloidae) are found throughout Arizona. These beetles contain a defensive chemical (cantharidin) that may be harmful to humans and other animals. Blister beetles are often times confused with other similar looking beetles that do not produce cantharidin. Blister beetles are found in many different sizes and colors. However, they all share the characteristic feature of a broad head that is wider than the thorax (“neck”). This, combined with broader elytra (wing covers), creates a distinct “neck-like” appearance (Fig. 1 & 2). They also have just 4 1 segments in their hind tarsi (Fig. 1). Blister beetles may be 2 confused with checkered beetles, soldier beetles, darkling beetles, 3 4 Figureground 8G. Adult beetles blister beetle, and Zonitis others atripennis beetles. (Fig.Figure 8H 2. –Adult6). blister beetle, Zonitis sayi. (Whitney (WhitneySandya Cranshaw, Colorado State University, Bugwood.org) Cranshaw, Colorado State University, Bugwood.org) BODY SOFT 4 TARSI IN Blister Beetle NOT Blister Beetles OR LEATHERY HINDLEG Athigiman Figure 1. Examples of two blister beetle species (Epicauta pardalis, left; Tegrodera aloga, right) with the characteristic narrow thorax (“neck”) , NMSU, Circular 536 Circular , NMSU, indicated by arrows. Blister beetles have soft, leathery bodies. Other Resources: Hall, WE, LM Brown, N Pier, PC Ellsworth. 2019. Blister Beetles in Food? U. Arizona. https://cals.arizona.edu/crops/cotton/files/BBinFood.pdf Figure 2. Left to right, Epicauta blister beetle, tamarisk leaf beetle, Pierce, JB. -

Blister Beetles (Insecta: Coleoptera: Meloidae)1 Richard B
EENY166 Blister Beetles (Insecta: Coleoptera: Meloidae)1 Richard B. Selander and Thomas R. Fasulo2 Introduction blister beetles are seldom seen, except for first instar larvae (triungulins) frequenting flowers or clinging to adult The family Meloidae, the blister beetles, contains about bees. All blister beetle larvae are specialized predators. 2500 species, divided among 120 genera and four subfami- Larvae of most genera enter the nests of wild bees, where lies (Bologna and Pinto 2001). Florida has 26 species, only they consume both immature bees and the provisions a small fraction of the total number in the US, but nearly of one or more nest cells. The larvae of some Meloinae, three times that of the West Indies (Selander and Bouseman including most Epicauta spp., prey on the eggs of acridid 1960). Adult beetles are phytophagous, feeding especially grasshoppers. A few larvae evidently prey on the eggs of on plants in the families Amaranthaceae, Asteraceae, blister beetles (Selander 1981). Of the Florida species, Fabaceae, and Solanaceae. Most adults eat only floral parts, Nemognatha punctulata LeConte (misidentified as Zonitis but some, particularly those of Epicauta spp., eat leaves as vittigera (LeConte)) has been found in a nest of a Megachile well. sp. in Cuba (Scaramuzza 1938) and several members of the genus Epicauta have been associated with the eggpods of Melanoplus spp. Figure 1. Adult Epicauta floridensis Werner (left), and E. cinerea Forster (right). Credits: Lyle J. Buss, University of Florida A few adults are nocturnal, but most are diurnal or show no distinct diel cycle. Since adults are gregarious and often Figure 2. -

Wöhler Synthesis of Urea
Wöhler synthesis of urea Wöhler, 1928 – – + + NH Cl + K N C O 4 NH4 N C O O H2N NH2 Friedrich Wöhler Annalen der Physik und Chemie 1828, 88, 253–256 Significance: Wöhler was the first to make an organic substance from an inorganic substance. This was the beginning of the end of the theory of vitalism: the idea that organic and inorganic materials differed essentially by the presence of the “vital force”– present only in organic material. To his mentor Berzelius:“I can make urea without thereby needing to have kidneys, or anyhow, an animal, be it human or dog" Friedrich Wöhler, 1880-1882 Polytechnic School in Berlin Support for vitalism remained until 1845, when Kolbe synthesized acetic acid Polytechnic School at Kassel from carbon disulfide University of Göttingen Fischer synthesis of glucose PhHN N O N O NHPh Br aq. HCl Δ PhNH2NH2 HO H HO H O Br "α−acrose" H OH H OH H OH H OH CH2OH CH2OH α−acrosazone α−acrosone an “osazone” (osazone test for reducing sugars) Zn/AcOH OH OH CO2H CHO O HO H HO H OH Br2 HO H HO H Na-Hg HO H HNO3 HO H H OH H OH H OH H OH then resolve H O+ H OH via strychnine H OH H OH 3 H OH CH2OH salts CH2OH CH OH CH2OH 2 D-Mannonic acid DL-Mannose DL-Mannitol DL-Fructose quinoline • Established stereochemical relationship CO2H CHO H OH H OH between mannose and glucose Na-Hg HO H HO H (part of Fischer proof) H OH + H OH H3O • work mechanisms from acrosazone on H OH H OH Emil Fischer, 1852-1919 CH2OH CH2OH University of Munich (1875-81) D-Gluconic acid D-Glucose University of Erlangen (1881-88) University of Würzburg (1888-92) University of Berlin (1892-1919) Fischer, E. -

Use of Cantharidin for Verruca
CHA PT ER 4 USE OF CANTHARIDIN FOR VERRUCA Mickey D. Stapp, DPM HISTORY MECHANISM OF ACTION Cantharidin has been used for more than 2,000 years in Cantharidin is a vesicant produced by beetles belonging to both folk and traditional medicine. It was used in China the order of Coleoptera and the family of Meloidae. for many medicinal purposes including furuncles, ulcers, and Cantharidin used medically is collected from species of the tuberculosis, topically, and for abdominal masses, rabies, and genera Mylabris and Lytta, especially Lytta vesicatoria, as an anticancer agent, orally. In Europe, it appeared in better known as “Spanish Fly.” The male blister beetle Materia Medica, a medical monograph written in 50 to produces the substance, giving the chemical to the female 100 AD. Hippocrates prescribed cantharidin as a treatment during mating. Afterwards the female beetle will cover its for dropsy (1). eggs with the chemical as a defense against predators (6). Cantharidin has a long infamous reputation for being Cantharidin acts as a blistering agent or acantholytic. an aphrodisiac and is known as Spanish fly. This reputation The lipid layers of epidermal cell membranes absorb it. Once is based on the observation of pelvic congestion in women applied, cantharidin causes release of neutral serine proteases and priapism in men after cantharidin ingestion. It is not that cause degeneration of the desmosmal plaque, leading a true aphrodisiac, and fatal poisonings can occur (2). to detachment of tonofilaments from desmosomes (7). This Cantharidin has also been used as a homicidal agent in leads to intraepidermal blistering and nonspecific lysis of the South Africa. -

Butterflies of North America
Insects of Western North America 7. Survey of Selected Arthropod Taxa of Fort Sill, Comanche County, Oklahoma. 4. Hexapoda: Selected Coleoptera and Diptera with cumulative list of Arthropoda and additional taxa Contributions of the C.P. Gillette Museum of Arthropod Diversity Colorado State University, Fort Collins, CO 80523-1177 2 Insects of Western North America. 7. Survey of Selected Arthropod Taxa of Fort Sill, Comanche County, Oklahoma. 4. Hexapoda: Selected Coleoptera and Diptera with cumulative list of Arthropoda and additional taxa by Boris C. Kondratieff, Luke Myers, and Whitney S. Cranshaw C.P. Gillette Museum of Arthropod Diversity Department of Bioagricultural Sciences and Pest Management Colorado State University, Fort Collins, Colorado 80523 August 22, 2011 Contributions of the C.P. Gillette Museum of Arthropod Diversity. Department of Bioagricultural Sciences and Pest Management Colorado State University, Fort Collins, CO 80523-1177 3 Cover Photo Credits: Whitney S. Cranshaw. Females of the blow fly Cochliomyia macellaria (Fab.) laying eggs on an animal carcass on Fort Sill, Oklahoma. ISBN 1084-8819 This publication and others in the series may be ordered from the C.P. Gillette Museum of Arthropod Diversity, Department of Bioagricultural Sciences and Pest Management, Colorado State University, Fort Collins, Colorado, 80523-1177. Copyrighted 2011 4 Contents EXECUTIVE SUMMARY .............................................................................................................7 SUMMARY AND MANAGEMENT CONSIDERATIONS -

Blister Beetles in Food? W
5/2019 Sandya Athigiman , NMSU, Circular 536 Circular , NMSU, Blister Beetles in Food? W. Eugene Hall1, Lydia M. Brown1, Naomi Pier1 and Peter C. Ellsworth2 University of Arizona, 1Assistants in Extension, 2IPM Specialist Beetles in food? Yuck! Well, just eat around them! That might be an option for you, but not for livestock including horses. And perhaps not the safest option for blister beetle contamination, because these beetles produce a defensive, toxic compound called Figure 1. Examples of the general body shape of blister beetles. Note the cantharidin in their blood. This chemical is especially toxic to “neck-like” appearance of the thorax just behind the head and how the horses if ingested in sufficient quantity. Thankfully, the effects on rest of the body is broader (from Pierce 2014). humans and other animals are far less serious, but still more unpleasant than just eating a beetle! Alexander Wild, ©alexanderwild.com Blister beetles (family Meloidae) are widely distributed, but only A B occasionally invade crop fields. Cantharidin is usually produced by male beetles and transferred to females during mating. Contact with cantharidin on the skin or mucous membranes can cause blistering or skin irritation. When ingested, the chemical irritates the gastrointestinal and urinary tracts, potentially leading to discomfort or illness, depending on the amount consumed. While not all species of blister beetles possess the same levels of cantharidin, avoid contact with them externally and internally. Found throughout North America, 150 species of blister beetles Figure 2. The Spotted occur in the Southwest; the majority are never found in agricultural Blister Beetle, Epicauta fields.