The Deubiquitylase USP10 Regulates Integrin Β1 and Β5 and Fibrotic Wound Healing Stephanie R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gene Section Short Communication
Atlas of Genetics and Cytogenetics in Oncology and Haematology INIST -CNRS OPEN ACCESS JOURNAL Gene Section Short Communication USP32 (ubiquitin specific peptidase 32) Aysegul Sapmaz, Ayse Elif Erson-Bensan Netherlands Cancer Institute-Antoni van Leeuwenhoek hospital (NKI-AVL), Amsterdam, Netherlands (AS), Department of Biological Sciences, Middle East Technical University, Ankara, Turkey (AS, AEEB) Published in Atlas Database: July 2013 Online updated version : http://AtlasGeneticsOncology.org/Genes/USP32ID52046ch17q23.html DOI: 10.4267/2042/52076 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 2.0 France Licence. © 2014 Atlas of Genetics and Cytogenetics in Oncology and Haematology Abstract: Short communication on USP32, with data on DNA/RNA, on the protein encoded and where the gene is implicated . - CA4 (17q23): carbonic anhydrase IV Identity - FAM106DP (Chr. 17): family with sequence Other names: NY-REN-60, USP10 similarity 106 memberD pseudogene HGNC (Hugo): USP32 - SCARNA20 (17q23.2): small cajal body specific RNA 20 Location: 17q23.1 - RPL32P32 (17q23.2): ribosomal protein L32 Local order: Based on Mapviewer (Master Map: Gene pseudogene 32 on sequence, gene flanking USP32 oriented from - LOC100418753 (Chr.17): septin 7 pseudogene centromere on 17q23.3 are: - USP32 (17q23.3): ubiquitin specific protease 32 - TBC1D3P1-DHX40P1 (17q23): TBC1D3P1- - LOC100506882 (Chr.17): uncharacterized DHX40P1 read through transcribed pseudogene LOC100506882 - MIR4737: MicroRNA 4737 - C17orf64 (17q23.2): chromosome 17 open reading - HEATR6 (17q23.1): Heat repeat containing 6 frame 64 - LOC100422693 (Chr.17): UDP-N-acetyl-alpha-D- - RPL12P38 (17q23.2): ribosomal protein L12 galactosamine :polypeptide N- pseudogene 38 acetylgalactosamyltransferase 1 (GalNAc-T1) - HMGN2P42 (Chr.17) high mobility group pseudogene nucleosomal binding domain 2 pseudogen 42 - LOC6456338 (17q23.1): WDNM1-like pseudogene - APPBP2 (17q23.2): amyloid beta precursor protein - LOC653653(17q23.1): adaptor-related protein (cytoplasmic tail binding protein 2. -

Anti-USP10 Antibody (ARG59869)
Product datasheet [email protected] ARG59869 Package: 100 μl anti-USP10 antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes USP10 Tested Reactivity Hu, Ms Tested Application ICC/IF, IHC-P Host Rabbit Clonality Polyclonal Isotype IgG Target Name USP10 Antigen Species Human Immunogen Recombinant fusion protein corresponding to aa. 499-798 of Human USP10 (NP_005144.2). Conjugation Un-conjugated Alternate Names Deubiquitinating enzyme 10; Ubiquitin thioesterase 10; UBPO; Ubiquitin-specific-processing protease 10; Ubiquitin carboxyl-terminal hydrolase 10; EC 3.4.19.12 Application Instructions Application table Application Dilution ICC/IF 1:50 - 1:200 IHC-P 1:50 - 1:200 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 87 kDa Properties Form Liquid Purification Affinity purified. Buffer PBS (pH 7.3), 0.02% Sodium azide and 50% Glycerol. Preservative 0.02% Sodium azide Stabilizer 50% Glycerol Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. www.arigobio.com 1/2 Bioinformation Gene Symbol USP10 Gene Full Name ubiquitin specific peptidase 10 Background Ubiquitin is a highly conserved protein that is covalently linked to other proteins to regulate their function and degradation. This gene encodes a member of the ubiquitin-specific protease family of cysteine proteases. -

Sleeping Beauty Transposon Mutagenesis Identifies Genes That
Sleeping Beauty transposon mutagenesis identifies PNAS PLUS genes that cooperate with mutant Smad4 in gastric cancer development Haruna Takedaa,b, Alistair G. Rustc,d, Jerrold M. Warda, Christopher Chin Kuan Yewa, Nancy A. Jenkinsa,e, and Neal G. Copelanda,e,1 aDivision of Genomics and Genetics, Institute of Molecular and Cell Biology, Agency for Science, Technology and Research, Singapore 138673; bDepartment of Pathology, School of Medicine, Kanazawa Medical University, Ishikawa 920-0293, Japan; cExperimental Cancer Genetics, Wellcome Trust Sanger Institute, Cambridge CB10 1HH, United Kingdom; dTumour Profiling Unit, The Institute of Cancer Research, Chester Beatty Laboratories, London SW3 6JB, United Kingdom; and eCancer Research Program, Houston Methodist Research Institute, Houston, TX 77030 Contributed by Neal G. Copeland, February 27, 2016 (sent for review October 15, 2015; reviewed by Yoshiaki Ito and David A. Largaespada) Mutations in SMAD4 predispose to the development of gastroin- animal models that mimic human GC, researchers have infected testinal cancer, which is the third leading cause of cancer-related mice with H. pylori and then, treated them with carcinogens. They deaths. To identify genes driving gastric cancer (GC) development, have also used genetic engineering to develop a variety of trans- we performed a Sleeping Beauty (SB) transposon mutagenesis genic and KO mouse models of GC (10). Smad4 KO mice are one + − screen in the stomach of Smad4 / mutant mice. This screen iden- GC model that has been of particular interest to us (11, 12). tified 59 candidate GC trunk drivers and a much larger number of Heterozygous Smad4 KO mice develop polyps in the pyloric re- candidate GC progression genes. -

The Tumor Suppressor Notch Inhibits Head and Neck Squamous Cell
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 12-2015 THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN) Shhyam Moorthy Shhyam Moorthy Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Biochemistry, Biophysics, and Structural Biology Commons, Cancer Biology Commons, Cell Biology Commons, and the Medicine and Health Sciences Commons Recommended Citation Moorthy, Shhyam and Moorthy, Shhyam, "THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN)" (2015). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 638. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/638 This Dissertation (PhD) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN) by Shhyam Moorthy, B.S. -

USP10 Promotes Proliferation of Hepatocellular Carcinoma By
Published OnlineFirst March 26, 2020; DOI: 10.1158/0008-5472.CAN-19-2388 CANCER RESEARCH | MOLECULAR CELL BIOLOGY USP10 Promotes Proliferation of Hepatocellular Carcinoma by Deubiquitinating and Stabilizing YAP/TAZ Hong Zhu1, Fangjie Yan1, Tao Yuan1, Meijia Qian1, Tianyi Zhou1, Xiaoyang Dai2,JiCao1, Meidan Ying1, Xiaowu Dong1, Qiaojun He1, and Bo Yang1 ABSTRACT ◥ Yes-associated protein (YAP) and its paralog, transcriptional tocellular carcinoma in vitro and in vivo. Expression levels coactivator with PDZ-binding motif (TAZ), play pivotal roles of USP10 positively correlated with the abundance of YAP/TAZ in promoting the progression of hepatocellular carcinoma. How- in hepatocellular carcinoma patient samples as well as in N- ever, the regulatory mechanism underpinning aberrant activation nitrosodiethylamine (DEN)-induced liver cancer mice models. of YAP/TAZ in hepatocellular carcinoma remains unclear. In Collectively, this study establishes the causal link between USP10 this study, we globally profiled the contribution of deubiquiti- andhyperactivatedYAP/TAZinhepatocellular carcinoma cells nating enzymes (DUB) to both transcriptional activity and and provides a rationale for potential therapeutic interventions in protein abundance of YAP/TAZ in hepatocellular carcinoma the treatment of patients with hepatocellular carcinoma harbor- models and identified ubiquitin-specificpeptidase10(USP10) ing a high level of YAP/TAZ. as a potent YAP/TAZ-activating DUB. Mechanistically, USP10 directly interacted with and stabilized YAP/TAZ by reverting Significance: These findings identify USP10 as a DUB of YAP/ their proteolytic ubiquitination. Depletion of USP10 enhanced TAZ and its role in hepatocellular carcinoma progression, which polyubiquitination of YAP/TAZ, promoted their proteasomal may serve as a potential therapeutic target for hepatocellular degradation, and ultimately arrested the proliferation of hepa- carcinoma treatment. -

USP10 Rabbit Pab
Leader in Biomolecular Solutions for Life Science USP10 Rabbit pAb Catalog No.: A13387 Basic Information Background Catalog No. Ubiquitin is a highly conserved protein that is covalently linked to other proteins to A13387 regulate their function and degradation. This gene encodes a member of the ubiquitin- specific protease family of cysteine proteases. The enzyme specifically cleaves ubiquitin Observed MW from ubiquitin-conjugated protein substrates. The protein is found in the nucleus and cytoplasm. It functions as a co-factor of the DNA-bound androgen receptor complex, Calculated MW and is inhibited by a protein in the Ras-GTPase pathway. The human genome contains 87kDa/92kDa several pseudogenes similar to this gene. Several transcript variants, some protein- coding and others not protein-coding, have been found for this gene. Category Primary antibody Applications WB,IHC,IF Cross-Reactivity Human, Mouse Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 9100 Q14694 IHC 1:50 - 1:100 Immunogen 1:50 - 1:100 IF Recombinant fusion protein containing a sequence corresponding to amino acids 499-798 of human USP10 (NP_005144.2). Synonyms UBPO;USP10 Contact Product Information 400-999-6126 Source Isotype Purification Rabbit IgG Affinity purification [email protected] www.abclonal.com.cn Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Immunohistochemistry of paraffin- Immunofluorescence analysis of A549 cells embedded mouse brain using USP10 using USP10 antibody (A13387). Blue: DAPI Antibody (A13387) at dilution of 1:100 (40x for nuclear staining. lens). Antibody | Protein | ELISA Kits | Enzyme | NGS | Service For research use only. -

Variation in Protein Coding Genes Identifies Information Flow
bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 1 1 2 3 4 5 Variation in protein coding genes identifies information flow as a contributor to 6 animal complexity 7 8 Jack Dean, Daniela Lopes Cardoso and Colin Sharpe* 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Institute of Biological and Biomedical Sciences 25 School of Biological Science 26 University of Portsmouth, 27 Portsmouth, UK 28 PO16 7YH 29 30 * Author for correspondence 31 [email protected] 32 33 Orcid numbers: 34 DLC: 0000-0003-2683-1745 35 CS: 0000-0002-5022-0840 36 37 38 39 40 41 42 43 44 45 46 47 48 49 Abstract bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 2 1 Across the metazoans there is a trend towards greater organismal complexity. How 2 complexity is generated, however, is uncertain. Since C.elegans and humans have 3 approximately the same number of genes, the explanation will depend on how genes are 4 used, rather than their absolute number. -
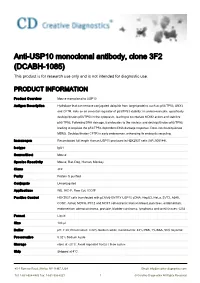
Anti-USP10 Monoclonal Antibody, Clone 3F2 (DCABH-1085) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-USP10 monoclonal antibody, clone 3F2 (DCABH-1085) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse monoclonal to USP10 Antigen Description Hydrolase that can remove conjugated ubiquitin from target proteins such as p53/TP53, SNX3 and CFTR. Acts as an essential regulator of p53/TP53 stability: in unstressed cells, specifically deubiquitinates p53/TP53 in the cytoplasm, leading to counteract MDM2 action and stabilize p53/TP53. Following DNA damage, translocates to the nucleus and deubiquitinates p53/TP53, leading to regulate the p53/TP53-dependent DNA damage response. Does not deubiquitinate MDM2. Deubiquitinates CFTR in early endosomes, enhancing its endocytic recycling. Immunogen Recombinant full length Human USP10 produced in HEK293T cells (NP_005144). Isotype IgG1 Source/Host Mouse Species Reactivity Mouse, Rat, Dog, Human, Monkey Clone 3F2 Purity Protein G purified Conjugate Unconjugated Applications WB, IHC-P, Flow Cyt, ICC/IF Positive Control HEK293T cells transfected with pCMV6-ENTRY USP10 cDNA; HepG2, HeLa, SVT2, A549, COS7, Jurkat, MDCK, PC12 and MCF7 cell extracts; Human breast, pancreas, endometrium, endometrium adenocarcinoma, prostate, bladder carcinoma, lymphoma and tonsil tissues; COS Format Liquid Size 100 μl Buffer pH: 7.30; Preservative: 0.02% Sodium azide; Constituents: 48% PBS, 1% BSA, 50% Glycerol Preservative 0.02% Sodium Azide Storage store at -20°C. Avoid repeated freeze / thaw cycles. Ship Shipped at 4°C. 45-1 Ramsey Road, Shirley, NY 11967, -

REVIEW Regulation of the Androgen Receptor by Post-Translational Modifications
221 REVIEW Regulation of the androgen receptor by post-translational modifications Kelly Coffey and Craig N Robson Solid Tumour Target Discovery Group, The Medical School, Newcastle Cancer Centre at the Northern Institute for Cancer Research, Newcastle University, Paul O’Gorman Building, Framlington Place, Newcastle upon Tyne, Tyne and Wear NE2 4HH, UK (Correspondence should be addressed to C N Robson; Email: [email protected]) Abstract The androgen receptor (AR) is a key molecule in prostate modifications have mostly been studied as individual events, it cancer and Kennedy’s disease. Understanding the regulatory is becoming clear that these modifications can functionally mechanisms of this steroid receptor is important in the interact with each other in a signalling pathway. In this review, development of potential therapies for these diseases. One the effects of all modifications are described with a focus on layer of AR regulation is provided by post-translational interplay between them and the functional consequences for modifications including phosphorylation, acetylation, the AR. sumoylation, ubiquitination and methylation. While these Journal of Endocrinology (2012) 215, 221–237 Introduction Many of the enzymes that are responsible for the modification of the receptor are dysregulated in disease, The androgen receptor (AR; Fig. 1) is a steroid hormone which results in aberrant AR activity. More recently, the receptor that plays a critical role in prostate cancer (PC) interplay between protein PTMs is becoming apparent. progression and development. In addition, it can also cause Where these modifications were thought to result in a simple spinal bulbar muscular dystrophy (commonly referred to as signal for the molecule to alter its activity or interaction with Kennedy’s disease). -

Allelic Loss in a Minimal Region on Chromosome 16Q24 Is Associated with Vitreous Seeding of Retinoblastoma
Research Article Allelic Loss in a Minimal Region on Chromosome 16q24 Is Associated with Vitreous Seeding of Retinoblastoma Sandrine Gratias,1 Harald Rieder,4 Reinhard Ullmann,5 Ludger Klein-Hitpass,2 Stephanie Schneider,6 Re´ka Bo¨lo¨ni,3 Martin Kappler,7 and Dietmar R. Lohmann1 1Institut fu¨r Humangenetik, 2Institut fu¨r Zellbiologie, and 3Augenklinik, Universita¨tsklinikum Essen, Essen, Germany; 4Institut fu¨r Humangenetik und Anthropologie, Universita¨tsstraße 1, Universita¨tDu¨sseldorf, Du¨sseldorf, Germany; 5Max-Planck Institute for Molecular Genetics, Berlin, Germany; 6Institut fu¨r Klinische Genetik, Universita¨tsklinikum Marburg, Marburg, Germany; and 7Berufsgenossenschaftliches Forschungsinstitut fu¨r Arbeitsmedizin, Ruhr-Universita¨tBochum, Bochum, Germany Abstract Loss of all or parts of chromosome 16 is observed in 31% of In addition to RB1 gene mutations, retinoblastomas frequently retinoblastomas (51 of 162; summarized in ref. 6). In most of these show gains of 1q and 6p and losses of 16q. To identify tumors, the whole long arm of one homologue is lost (40 of suppressor genes on 16q, we analyzed 22 short tandem repeat 51, 78%). A survey of comparative genomic hybridization (CGH) loci in 58 patients with known RB1 mutations. A subset of analyses has indicated that most partial deletions on chromosome tumors was also investigated by conventional and matrix 16q include chromosome band 16q22 (7 of 11, 64%; ref. 3). To study comparative genomic hybridization. In 40 of 58 (69%) tumors, alterations of this region in further detail, Marchong et al. (6) did LOH analysis of seven microsatellite markers located on 16q21-23.3 we found no loss of heterozygosity (LOH) at any 16q marker. -

Notch Controls Arterialization by Regulating the Cell Cycle and Not Differentiation
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.07.192344; this version posted July 7, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Notch controls arterialization by regulating the cell cycle and not differentiation Wen Luo,1 Irene Garcia-Gonzalez,1 Macarena Fernandez-Chacon, 1 Veronica Casquero-Garcia, 1 Rui Benedito1,* 1Molecular Genetics of Angiogenesis Group. Centro Nacional de Investigaciones Cardiovasculares (CNIC), Melchor Fernandez Almagro, 3, Madrid, Spain *Correspondence: [email protected] Abstract Arteries are thought to be formed by the induction of a highly conserved arterial genetic program in a subset of vessels experiencing an increase in pulsatile and oxygenated blood flow. Both VEGF and Notch signalling have been shown to be essential for the initial steps of arterial specification. Here, we combined inducible genetic mosaics and transcriptomics to modulate and understand the function of these signalling pathways on cell proliferation, arterial-venous differentiation and mobilization. We observed that endothelial cells with high VEGF or Notch signalling are not genetically pre-determined and can form both arteries and veins. Importantly, cells completely lacking the Notch-Rbpj transcriptional activator complex can form arteries when the Myc- dependent metabolic and cell-cycle activity is suppressed. Thus, arterial development does not require the induction of a Notch-dependent arterial differentiation program, but rather the timely suppression of the endothelial metabolism and cell-cycle, a process preceding arterial mobilization and complete differentiation. Introduction Angiogenesis occurs through the reiterative growth and remodeling of a precursor angiogenic vascular plexus. -

Caprin-1 Binding to the Critical Stress Granule Protein G3BP1 Is Regulated by Ph
bioRxiv preprint doi: https://doi.org/10.1101/2021.02.05.429362; this version posted February 5, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Caprin-1 binding to the critical stress granule protein G3BP1 is regulated by pH 1 2, 2 3 1 Tim Schulte* , Marc D. Panas* Lucy Williams , Nancy Kedersha , Jonas Simon Fleck , Timothy J.C. Tan2, Anders Olsson4, Ainhoa Moliner Morro 2, Leo Hanke 2, Johan Nilvebrant5, Kim Anh Giang5, Per-Åke Nygren5, Paul Anderson 3, Adnane Achour# 1, Gerald M. McInerney# 2 1 Science for Life Laboratory, Department of Medicine Solna, Karolinska Institutet, and Division of Infectious Diseases, Karolinska University Hospital, Stockholm, 171 77, Sweden 2 Department of Microbiology, Tumor and Cell Biology, Karolinska Institutet, Stockholm, 171 77, Sweden 3 Division of Rheumatology, Immunity, and Inflammation, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02115, USA; Harvard Medical School Initiative for RNA Medicine, Harvard Medical School, Boston, MA 02115, USA 4 Protein Expression and Characterization, Royal Institute of Technology, Stockholm, and Science for Life Laboratory, Solna, Sweden. 5 Division of Protein Engineering, Department of Protein Science, School of Engineering Sciences in Chemistry, Biotechnology and Health, AlbaNova University Center, Royal Institute of Technology, Stockholm, and Science for Life Laboratory, Solna, Sweden. *, # These authors contributed equally. For correspondence: [email protected], [email protected] Abstract G3BP is the central hub within the protein-RNA interaction network of stress-induced bio-molecular condensates known as stress granules (SG).