2019-2020 Third Year Rotation Information and Affiliates Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COMLEX-USA for Residency Program Directors
COMLEX-USA FOR RESIDENCY PROGRAM DIRECTORS COMLEX-USA Evidence–based assessment designed specifically for osteopathic medical students and residents that measures competencies required for the provision of safe and effective osteopathic medical care to patients. It is recommended but not required that COMLEX-USA Level 3 be taken after a minimum of six months in residency. The attestation process for COMLEX-USA Level 3 helps to fulfill the NBOME mission to DO candidates are not required to pass the United States protect the public, and adds value and entrustability to state licensing Medical Licensing Examination (USMLE®) to be eligible to boards and patients. Additionally, attestation provides COMLEX-USA apply to ACGME-accredited residency programs. The score reports to residency program directors and faculty. ACGME does not specify which licensing board exam(s) (i.e., COMLEX-USA, USMLE) applicants must take to be eligible COMPETENCY AND EVIDENCE-BASED DESIGN for appointment in ACGME-accredited residency programs. In 2019, COMLEX-USA completed a transition to a contemporary, two Frequently Asked Questions: Single Accreditation System decision-point, competency-based exam blueprint and evidence- Accreditation Council for Graduate Medical Education, 20191 based design informed by extensive research on osteopathic physician practice, expert consensus and stakeholder surveys.3 The enhanced COMLEX-USA blueprint4 assesses measurable outcomes PATHWAY TO LICENSURE of seven Fundamental Osteopathic Medical Competency Domains5 COMLEX-USA, the Comprehensive Osteopathic Medical Licensing and focuses on high-frequency, high-impact health issues and clinical Examination of the United States, is the exam series used by all presentations that affect patients. medical licensing authorities to make licensing decisions for osteopathic physicians. -

PPC-Infographic.Pdf
Celebrating our 15th anniversary, Partnership for Patient Care (PPC) is the region’s premier patient safety and quality program driving health equity and high quality outcomes. 115th5th Anniversary 2006 – 2021 WHAT IS PARTNERSHIP FOR PATIENT CARE? Partnership for Patient Care (PPC) is a collaboration between Independence Blue Cross, Health Care Improvement Foundation and the region’s leading healthcare organizations and stakeholders to accelerate the adoption of evidence-based clinical best practices. PPC’s improvement efforts have enabled the region to foster partnerships among organizations that share a common desire for providing the safest and highest quality care to patients. PPC serves as an umbrella, under which several programs have been established during the past 15 years to support ongoing regional improvement. PPC PROGRAMS Health Equity Data Strategy (HEDS) NEW New in 2021, HEDS is a regional collaborative aimed at decreasing disparities in health outcomes with a focus on establishing recommendations for the implementation of a health equity data strategy. This program will support organizations in the accurate and reliable collection of REaL (ethnicity, and language) data, utilization of the data to evaluate health outcomes, identification of disparities across populations and health conditions; and implementation of targeted quality improvement strategies that promote health equity. Safety Forum 100% A forum of front-line patient safety leaders from hospitals across Southeastern PA that of participants rated promotes interactive discussions about safety hazards and vulnerabilities and a peer- the program as very good or excellent to-peer exchange of patient safety approaches, processes, and best practices. Pennsylvania Urologic Regional Collaborative (PURC) 142 PURC is a quality improvement initiative that brings urology practices together in a physician- participating physicians led, data-sharing and improvement collaborative aimed at advancing the quality of diagnosis 17,000+ and care for men with prostate cancer. -
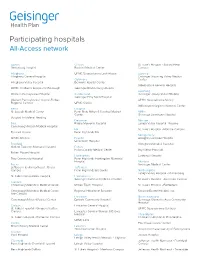
Participating Hospitals All-Access Network
Participating hospitals All-Access network Adams Clinton St. Luke’s Hospital - Sacred Heart Gettysburg Hospital Bucktail Medical Center Campus Allegheny UPMC Susquehanna Lock Haven Luzerne Allegheny General Hospital Geisinger Wyoming Valley Medical Columbia Center Allegheny Valley Hospital Berwick Hospital Center Wilkes-Barre General Hospital UPMC Children’s Hospital of Pittsburgh Geisinger Bloomsburg Hospital Lycoming Western Pennsylvania Hospital Cumberland Geisinger Jersey Shore Hospital Geisinger Holy Spirit Hospital Western Pennsylvania Hospital-Forbes UPMC Susquehanna Muncy Regional Campus UPMC Carlisle Williamsport Regional Medical Center Berks Dauphin St. Joseph Medical Center Penn State Milton S Hershey Medical Mifflin Center Geisinger Lewistown Hospital Surgical Institute of Reading Delaware Monroe Blair Riddle Memorial Hospital Lehigh Valley Hospital - Pocono Conemaugh Nason Medical Hospital Elk St. Luke’s Hospital - Monroe Campus Tyrone Hospital Penn Highlands Elk Montgomery UPMC Altoona Fayette Abington Lansdale Hospital Uniontown Hospital Bradford Abington Memorial Hospital Guthrie Towanda Memorial Hospital Fulton Fulton County Medical Center Bryn Mawr Hospital Robert Packer Hospital Huntingdon Lankenau Hospital Troy Community Hospital Penn Highlands Huntingdon Memorial Hospital Montour Bucks Geisinger Medical Center Jefferson Health Northeast - Bucks Jefferson Campus Penn Highlands Brookville Northampton Lehigh Valley Hospital - Muhlenberg St. Luke's Quakertown Hospital Lackawanna Geisinger Community Medical Center St. Luke’s Hospital - Anderson Campus Cambria Conemaugh Memorial Medical Center Moses Taylor Hospital St. Luke’s Hospital - Bethlehem Conemaugh Memorial Medical Center - Regional Hospital of Scranton Steward Easton Hospital, Inc. Lee Campus Lancaster Northumberland Conemaugh Miners Medical Center Ephrata Community Hospital Geisinger Shamokin Area Community Hospital Carbon Lancaster General Hospital St. Luke’s Hospital - Gnaden Huetten UPMC Susquehanna Sunbury Campus Lancaster General Women & Babies Hospital Philadelphia St. -

Employee Handbook
Employee Handbook You and Jefferson Thomas Jefferson University & Hospitals Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System Dear Colleague, Welcome to Thomas Jefferson University and Hospitals! In accepting your new position, you have joined a team committed to redefining healthcare. With a robust history and community roots dating back to 1824, Jefferson is a nationally influential and widely respected academic medical center. We deliver high quality, personalized and compassionate care, and you are now a vital part of our tradition of excellence. By selecting Jefferson, you will enjoy competitive pay, a broad selection of employee benefits from which to choose, opportunity for educational and developmental growth, and a challenging and interactive work environment. Congratulations and my best wishes as you assume your new responsibilities at Jefferson. Sincerely, Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System About This Handbook This employee handbook has been designed to provide you with general information about various policies, benefits, services and facilities of Jefferson which may be of interest to you in the course of your employment. Please understand that it only highlights these topics. More specific information may be obtained from your supervisor, the hospital intranet, where any specific policies cited here may be found or the Department of Human Resources at Suite 2150 Gibbon Building or Methodist Administration Suite. You are strongly encouraged to become acquainted with all Jefferson policies and procedures to make your employment as satisfying and productive as possible. The policies, procedures and benefits described in this handbook are not all-inclusive and may be amended or rescinded from time to time at the discretion of Jefferson, with or without notice. -
Restructuring the MLH/Jefferson Partnership
Main Line Health Physician Restructuring the MLH/Jefferson partnership Surviving Sepsis: The future of Hepatology: SUMMER 2014 ED success moves health care at From Hep C to Inside: to inpatient Exton Square Mall transplant care Main Line Health Physician Medical staff education initiative BY ANGUS GILLIS, MD The Main Line Health medical staff structure is an integrated model that encompasses private practice MESSAGES | 2 physicians who are on staff, hospital-employed physicians, and physicians/physician groups who are under contract for provision of services to the Hospital System. Medical staff functions have traditionally included initial credentialing, reappointment, and approval of privileges for new procedures. Tools used to fulfill these tasks include focused and ongoing professional practice evaluation (FPPE and OPPE). The staff is responsible for peer review, including case study and quality concerns. By-law and policy issues such as investigations, interventions, confidentiality, and physician rights are also areas in which the medical staff is involved. The staff has administrative functions related to patient safety, infection control, pharmacy and therapeutics, medical records, and behavioral issues like disruptive behavior and practitioner health. This is only a partial list of the responsibilities of the medical staff. Ultimate responsibility for approval and implementation of any recommendations by the staff’s Medical Executive Committee lies with the Board of Main Line Health. In addition to the above functions, the medical staff also takes an active role in continuing medical education. Your medical staff dues have always funded clinical educational efforts, such as Grand Rounds, at our various locations. A new additional effort is the Medical Executive Committee’s budgeting of dedicated monies for physician education, which will enable members to carry out these medical staff responsibilities. -
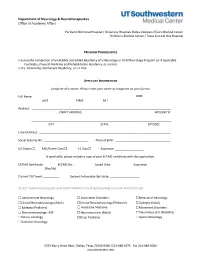
Neurology Fellowship Application
Department of Neurology & Neurotherapeutics Office of Academic Affairs Parkland Memorial Hospital / University Hospitals Dallas Veterans Affairs Medical Center Children's Medical Center / Texas Scottish Rite Hospital PROGRAM PREREQUISITES • Successful completion of an ACGME accredited Residency of a Neurology or Child Neurology Program (or if applicable Psychiatry, Physical Medicine and Rehabilitation Residency, or similar). • U.S. Citizenship, Permanent Residency, or J-1 Visa APPLICANT INFORMATION Complete all sections. Please enter your name as it appears on your license. Full Name: DOB: LAST FIRST M.I. Address: STREET ADDRESS APT/UNIT # ______________________________________________________________________________________ CITY STATE ZIP CODE Email Address: _________________________________________________________________________________ Social Security No.: ___________________________ Place of Birth: __________________________________ US Citizen ☐ EAD/Green Card ☐ J-1 Visa ☐ Expiration __________________ If applicable, please include a copy of your ECFMG certificate with this application. ECFMG Certificate: ________ ECFMG No.: ____________ Issued Date: _____________ Expiration ______________ (Yes/No) Current PGY level: __________ Desired Fellowship start date: __________________ SELECT WHICH NEUROLOGY & NEUROTHERAPEUTICS FELLOWSHIP(S) YOU ARE APPLYING FOR: ☐ Autoimmune Neurology ☐ Autonomic Disorders ☐Behavioral Neurology ☐Clinical Neurophysiology (Adult) ☐Clinical Neurophysiology (Pediatric) ☐ Epilepsy (Adult) ☐ Epilepsy (Pediatric) -

Designated Acute Care Hospital Stroke Centers 180424
Acute Stroke -ready; Comprehensive stroke COUNTY FACILITY NAME CITY ZIP Center or Primary Stroke Center? MONTGOMERY Abington Memorial Hospital Comprehensive stroke Center Abington 19001 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 CUMBERLAND Carlisle Regional Medical Center Primary Stroke Center Carlisle 17015 FRANKLIN Chambersburg Hospital Primary Stroke Center Chambersburg 17201 CHESTER Chester County Hospital – Chester County Primary Stroke Center West Chester 19380 CAMBRIA Conemaugh Memorial Medical Center Primary Stroke Center Johnstown 15905 BLAIR Conemaugh Nason Medical Center Acute Stroke -ready Roaring Spring 16673 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 MONTGOMERY Einstein Medical Center Montgomery Primary Stroke Center East Norriton 19403 LANCASTER Ephrata Community Hospital Primary Stroke Center Ephrata 17522 WESTMORELAND Excela Health Frick Hospital Primary Stroke Center Westmoreland 15666 WESTMORELAND Excela Health Latrobe Hospital Primary Stroke Center Latrobe 15650 WESTMORELAND Excela Health Westmoreland Hospital Primary Stroke Center Greensburg 15601 LACKAWANNA Geisinger Community Medical Center – Scranton - Lackawanna County Primary Stroke Center Scranton 18510 MONTOUR Geisinger Medical Center – Montour County Primary Stroke Center Danville 17822 LUZERNE Geisinger Wyoming Valley Medical Center, Wilkes-Barre – Luzerne County Primary Stroke Center Wilkes Barre 18711 ADAMS Gettysburg Hospital Primary Stroke Center Gettysburg 17325 CARBON Gnadden Huetten Memorial -

Boston Children's Hospital / Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health
Boston Children’s Hospital/Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health Speaker Alan Woolf, MD, MPH, FAACT, FAAP, FACMT Director, Pediatric Environmental Health Center, Boston Children’s Hospital Director, Region 1 New England PEHSU Director, Fellowship Training Program Professor, Harvard Medical School School Physician Acknowledgments & Disclosures This material was supported by the American Academy of Pediatrics (AAP) and funded (in part) by the cooperative agreement FAIN: 5 NU61TS000237-05 from the Agency for Toxic Substances and Disease Registry (ATSDR). Funding for this seminar was made possible (in part) by the cooperative agreement award number 1U61TS000237- 05 from the Agency for Toxic Substances and Disease Registry (ATSDR). The views expressed in written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services. •The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government •Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications. •In the past 12 months, we have had no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed -

HMO Proactive Tiered Network Hospital List
Save with Keystone HMO Proactive, our most popular plans Keystone HMO Proactive health plans are our most popular for good reason: You get access to high-quality care and save money. Not only do you pay less for your monthly premiums, but you can save even more by choosing doctors and hospitals in Tier 1 – Preferred. Save with Tier 1 – Preferred Tier 1 – Preferred includes more than 50 percent of the network. Keystone HMO Proactive offers the same essential health benefits as our other health plans, including doctor visits, Tier 1 – Preferred hospital stays, prescription drug coverage, blood tests, and X-rays. The difference is its tiered provider network, which gives you the option to pay less for care by choosing Tier 1 –Preferred providers. Here are the most important things to know about Keystone HMO Proactive: • You can visit any doctor or hospital in the Independence Blue Cross network once you have a referral. Tier 2 – Enhanced Tier 3 – Standard • You will select a PCP to coordinate your care and refer you to specialists. • Some services cost the same no matter what provider you Save even more choose — like preventive care, emergency room visits, and Keystone HMO Silver Proactive Select and Keystone HMO Silver urgent care. Proactive Value: These lower-premium options are only available • When you use doctors and hospitals in Tier 1 – Preferred, when you purchase directly from Independence Blue Cross. you pay the lowest out-of-pocket costs. Keystone HMO Silver Proactive Value includes a deductible for • The choice is always yours. You can choose Tier 1 providers Tiers 1 – 3 for some services. -
Medical Scientist Training Program
The University of Michigan MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines A Handbook for Fellows https://www.medicine.umich.edu/medschool/education/md-phd- program/current students/ August 2018 CONTENTS 1. MSTP Office 2. Communication 3. Academic Advising 4. I.D. and Computer Access 5. Course of Study 6. Biological Chemistry Requirement 7. Medical School Registration 8. Medical and Graduate School Grading Systems 9. Graduate School Registration 10. Research Rotations 11. Selecting a Doctoral Field and the Thesis Research Mentor 12. Graduate School Residency Requirements 13. Research Responsibility and Ethics Requirements 14. Research Phase: External Funding Sources 15. Advancement to Candidacy 16. Precandidate Year to Candidacy Transition: Funding and Insurance Issues 17. Research Phase to M3 Transition 18. M4 Year 19. Transition to Post Graduate Training, Residency 20. Dean’s Letters 21. Simultaneous Awarding of Dual Degrees 22. United States Medical Licensure Examination Step 1 and Step 2 (Clinical Knowledge and Clinical Skills) 23. Rackham Graduate School Policies 24. Medical School Policies and Procedures 25. The Fellowship Award and the Stipend Level 26. Monthly Stipend Check 27. Taxability of NRSA Stipends 28. NIH Funding Trainee Appointment Forms and Trainee Termination Notice Forms 29. Tuition Payment, Billing Procedures, and Registration 30. Travel Funds and Expense Forms 31. Health Care Insurance 32. Health Service 33. CV and Publication File 34. Individual Development Pan (IDP) 35. Vacations and Other Absences 36. MSTP Scientific Retreat 37. MSTP Seminars 38. Citizenship 39. MSTP Committees: Operating Committee (OC) and Program Activities Committee (PAC) A Handbook for MSTP Fellows MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines for Fellows 1. -

Primer for Applying to Internal Medicine Residency Programs A
Primer for Applying to Internal Medicine Residency Programs A) Fourth-Year Schedule: • Ideally, schedule the internal medicine sub-internship during July or August in order to procure a letter of recommendation (if needed). • Alternative clinical experiences to consider in place of the sub-internship include: o Away rotations: ▪ Away rotations are NOT required for IM. The majority of students applying to IM across the country do not partake in visiting rotations. Visiting rotations are most helpful if students demonstrate a significant interest in a particular program or location. ▪ Away rotations may increase the chance of an invitation to interview at the hosting institution, but this is NOT guaranteed. ▪ Visiting subspecialty electives are preferred over visiting sub- internships, which require strong institutional systems knowledge to optimize clinical performance. o Critical Care Clerkship o Subspecialty Rotations at Cooper • IM residency interviews often start in mid-October and extend to the end of January with the majority of interviews occurring in November and December. Therefore, plan accordingly. • Schedule a more rigorous clinical experience in the spring to enhance clinical skills prior to graduation in preparation for residency. B) Timeline: C) Curriculum Vitae & ERAS Application: • Timeline: Should include all longitudinal, meaningful experiences from the first day of college until present day. • Experience Boxes: o Research Experience: ▪ Include all meaningful research at both the undergraduate and medical school level -
SAP Crystal Reports
Results of the 2016 NRMP Program Director Survey Specialties Matching Service October 2016 www.nrmp.org Requests for permission to use these data as well as questions about the content of this publication or the National Resident Matching Program data and reports may be directed to Mei Liang, Director of Research, NRMP, at [email protected]. Questions about the NRMP should be directed to Mona M. Signer, President and CEO, NRMP, at [email protected]. Suggested Citation National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey, Specialties Matching Service. National Resident Matching Program, Washington, DC. 2016. Copyright © 2016 National Resident Matching Program. All rights reserved. Permission to use, copy and/or distribute any documentation and/or related images from this publication shall be expressly obtained from the NRMP. Table of Contents Introduction .................................................................................................................................................... 1 Response rates ................................................................................................................................................. 2 All Specialties................................................................................................................................................. 3 Charts for Individual Specialties Abdominal Transplant Surgery ....................................................................................................................