Chapter 21 – Miscellaneous Bacterial Agents of Disease*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Official Nh Dhhs Health Alert
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Phagocytosis of Borrelia Burgdorferi, the Lyme Disease Spirochete, Potentiates Innate Immune Activation and Induces Apoptosis in Human Monocytes Adriana R
University of Connecticut OpenCommons@UConn UCHC Articles - Research University of Connecticut Health Center Research 1-2008 Phagocytosis of Borrelia burgdorferi, the Lyme Disease Spirochete, Potentiates Innate Immune Activation and Induces Apoptosis in Human Monocytes Adriana R. Cruz University of Connecticut School of Medicine and Dentistry Meagan W. Moore University of Connecticut School of Medicine and Dentistry Carson J. La Vake University of Connecticut School of Medicine and Dentistry Christian H. Eggers University of Connecticut School of Medicine and Dentistry Juan C. Salazar University of Connecticut School of Medicine and Dentistry See next page for additional authors Follow this and additional works at: https://opencommons.uconn.edu/uchcres_articles Part of the Medicine and Health Sciences Commons Recommended Citation Cruz, Adriana R.; Moore, Meagan W.; La Vake, Carson J.; Eggers, Christian H.; Salazar, Juan C.; and Radolf, Justin D., "Phagocytosis of Borrelia burgdorferi, the Lyme Disease Spirochete, Potentiates Innate Immune Activation and Induces Apoptosis in Human Monocytes" (2008). UCHC Articles - Research. 182. https://opencommons.uconn.edu/uchcres_articles/182 Authors Adriana R. Cruz, Meagan W. Moore, Carson J. La Vake, Christian H. Eggers, Juan C. Salazar, and Justin D. Radolf This article is available at OpenCommons@UConn: https://opencommons.uconn.edu/uchcres_articles/182 INFECTION AND IMMUNITY, Jan. 2008, p. 56–70 Vol. 76, No. 1 0019-9567/08/$08.00ϩ0 doi:10.1128/IAI.01039-07 Copyright © 2008, American Society for Microbiology. All Rights Reserved. Phagocytosis of Borrelia burgdorferi, the Lyme Disease Spirochete, Potentiates Innate Immune Activation and Induces Apoptosis in Human Monocytesᰔ Adriana R. Cruz,1†‡ Meagan W. Moore,1† Carson J. -

Fournier's Gangrene Caused by Listeria Monocytogenes As
CASE REPORT Fournier’s gangrene caused by Listeria monocytogenes as the primary organism Sayaka Asahata MD1, Yuji Hirai MD PhD1, Yusuke Ainoda MD PhD1, Takahiro Fujita MD1, Yumiko Okada DVM PhD2, Ken Kikuchi MD PhD1 S Asahata, Y Hirai, Y Ainoda, T Fujita, Y Okada, K Kikuchi. Une gangrène de Fournier causée par le Listeria Fournier’s gangrene caused by Listeria monocytogenes as the monocytogenes comme organisme primaire primary organism. Can J Infect Dis Med Microbiol 2015;26(1):44-46. Un homme de 70 ans ayant des antécédents de cancer de la langue s’est présenté avec une gangrène de Fournier causée par un Listeria A 70-year-old man with a history of tongue cancer presented with monocytogenes de sérotype 4b. Le débridement chirurgical a révélé un Fournier’s gangrene caused by Listeria monocytogenes serotype 4b. adénocarcinome rectal non diagnostiqué. Le patient n’avait pas Surgical debridement revealed undiagnosed rectal adenocarcinoma. d’antécédents alimentaires ou de voyage apparents, mais a déclaré The patient did not have an apparent dietary or travel history but consommer des sashimis (poisson cru) tous les jours. reported daily consumption of sashimi (raw fish). L’âge avancé et l’immunodéficience causée par l’adénocarcinome rec- Old age and immunodeficiency due to rectal adenocarcinoma may tal ont peut-être favorisé l’invasion directe du L monocytogenes par la have supported the direct invasion of L monocytogenes from the tumeur. Il s’agit du premier cas déclaré de gangrène de Fournier tumour. The present article describes the first reported case of attribuable au L monocytogenes. Les auteurs proposent d’inclure la con- Fournier’s gangrene caused by L monocytogenes. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Borrelia Burgdorferi and Treponema Pallidum: a Comparison of Functional Genomics, Environmental Adaptations, and Pathogenic Mechanisms
PERSPECTIVE SERIES Bacterial polymorphisms Martin J. Blaser and James M. Musser, Series Editors Borrelia burgdorferi and Treponema pallidum: a comparison of functional genomics, environmental adaptations, and pathogenic mechanisms Stephen F. Porcella and Tom G. Schwan Laboratory of Human Bacterial Pathogenesis, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, NIH, Hamilton, Montana, USA Address correspondence to: Tom G. Schwan, Rocky Mountain Laboratories, 903 South 4th Street, Hamilton, Montana 59840, USA. Phone: (406) 363-9250; Fax: (406) 363-9445; E-mail: [email protected]. Spirochetes are a diverse group of bacteria found in (6–8). Here, we compare the biology and genomes of soil, deep in marine sediments, commensal in the gut these two spirochetal pathogens with reference to their of termites and other arthropods, or obligate parasites different host associations and modes of transmission. of vertebrates. Two pathogenic spirochetes that are the focus of this perspective are Borrelia burgdorferi sensu Genomic structure lato, a causative agent of Lyme disease, and Treponema A striking difference between B. burgdorferi and T. pal- pallidum subspecies pallidum, the agent of venereal lidum is their total genomic structure. Although both syphilis. Although these organisms are bound togeth- pathogens have small genomes, compared with many er by ancient ancestry and similar morphology (Figure well known bacteria such as Escherichia coli and Mycobac- 1), as well as by the protean nature of the infections terium tuberculosis, the genomic structure of B. burgdorferi they cause, many differences exist in their life cycles, environmental adaptations, and impact on human health and behavior. The specific mechanisms con- tributing to multisystem disease and persistent, long- term infections caused by both organisms in spite of significant immune responses are not yet understood. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Cutaneous Melioidosis Dermatology Section
DOI: 10.7860/JCDR/2016/18823.8463 Case Report Cutaneous Melioidosis Dermatology Section BASAVAPRABHU ACHAPPA1, DEEPAK MADI2, K. VIDYALAKSHMI3 ABSTRACT Melioidosis is an emerging infection in India. It usually presents as pneumonia. Melioidosis presenting as cutaneous lesions is uncommon. We present a case of cutaneous melioidosis from Southern India. Cutaneous melioidosis can present as an ulcer, pustule or as crusted erythematous lesions. A 22-year-old gentleman known case of diabetes mellitus was admitted in our hospital with an ulcer over the left thigh. Discharge from the ulcer grew Burkholderia pseudomallei. He was successfully treated with ceftazidime. Melioidosis must be considered in the differential diagnosis of nodular or ulcerative cutaneous lesion in a diabetic patient. Keywords: B. pseudomallei, Diabetes Mellitus, Skin ulcer CASE REPORT melioidosis is a rare entity. Cutaneous melioidosis may be primary A 22-year-old gentleman was admitted in our hospital with (presenting symptom is skin infection) or secondary (melioidosis complaints of an ulcer over the left thigh of seven days duration. at other sites in the body with incidental skin involvement) [3]. History of fever was present for four days. He also complained of There is limited published data from India documenting cutaneous pain in the thigh. The patient initially noticed a nodule on the left melioidosis. thigh which eventually progressed to form a discharging ulcer. He B. pseudomallei reside in soil and water [4]. Inoculation, inhalation was a known case of diabetes mellitus (type 1) on insulin. Clinical or ingestion of infected food or water are the modes of transmission examination revealed a 5cm× 5cm ulcer on the left thigh with [5]. -
Necrotizing Fasciitis
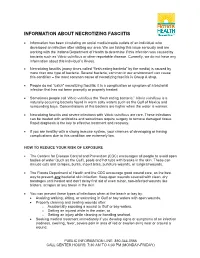
INFORMATION ABOUT NECROTIZING FASCIITIS • Information has been circulating on social media/media outlets of an individual who developed an infection after visiting our area. We are taking this issue seriously and are working with the Indiana Department of Health to determine if this infection was caused by bacteria such as Vibrio vulnificus or other reportable disease. Currently, we do not have any information about this individual’s illness. • Necrotizing fasciitis (many times called “flesh eating bacteria” by the media) is caused by more than one type of bacteria. Several bacteria, common in our environment can cause this condition – the most common cause of necrotizing fasciitis is Group A strep. • People do not “catch” necrotizing fasciitis; it is a complication or symptom of a bacterial infection that has not been promptly or properly treated. • Sometimes people call Vibrio vulnificus the “flesh eating bacteria.” Vibrio vulnificus is a naturally occurring bacteria found in warm salty waters such as the Gulf of Mexico and surrounding bays. Concentrations of this bacteria are higher when the water is warmer. • Necrotizing fasciitis and severe infections with Vibrio vulnificus are rare. These infections can be treated with antibiotics and sometimes require surgery to remove damaged tissue. Rapid diagnosis is the key to effective treatment and recovery. • If you are healthy with a strong immune system, your chances of developing or having complications due to this condition are extremely low. HOW TO REDUCE YOUR RISK OF EXPOSURE • The Centers for Disease Control and Prevention (CDC) encourages all people to avoid open bodies of water (such as the Gulf), pools and hot tubs with breaks in the skin. -

CD Alert Monthly Newsletter of National Centre for Disease Control, Directorate General of Health Services, Government of India
CD Alert Monthly Newsletter of National Centre for Disease Control, Directorate General of Health Services, Government of India May - July 2009 Vol. 13 : No. 1 SCRUB TYPHUS & OTHER RICKETTSIOSES it lacks lipopolysaccharide and peptidoglycan RICKETTSIAL DISEASES and does not have an outer slime layer. It is These are the diseases caused by rickettsiae endowed with a major surface protein (56kDa) which are small, gram negative bacilli adapted and some minor surface protein (110, 80, 46, to obligate intracellular parasitism, and 43, 39, 35, 25 and 25kDa). There are transmitted by arthropod vectors. These considerable differences in virulence and organisms are primarily parasites of arthropods antigen composition among individual strains such as lice, fleas, ticks and mites, in which of O.tsutsugamushi. O.tsutsugamushi has they are found in the alimentary canal. In many serotypes (Karp, Gillian, Kato and vertebrates, including humans, they infect the Kawazaki). vascular endothelium and reticuloendothelial GLOBAL SCENARIO cells. Commonly known rickettsial disease is Scrub Typhus. Geographic distribution of the disease occurs within an area of about 13 million km2 including- The family Rickettsiaeceae currently comprises Afghanistan and Pakistan to the west; Russia of three genera – Rickettsia, Orientia and to the north; Korea and Japan to the northeast; Ehrlichia which appear to have descended Indonesia, Papua New Guinea, and northern from a common ancestor. Former members Australia to the south; and some smaller of the family, Coxiella burnetii, which causes islands in the western Pacific. It was Q fever and Rochalimaea quintana causing first observed in Japan where it was found to trench fever have been excluded because the be transmitted by mites. -

Chlamydophila Felis Prevalence Chlamydophila Felis Prevalence
ORIGINAL SCIENTIFIC ARTICLE / IZVORNI ZNANSTVENI ČLANAK A preliminary study of Chlamydophila felis prevalence among domestic cats in the City of Zagreb and Zagreb County in Croatia Gordana Gregurić Gračner*, Ksenija Vlahović, Alenka Dovč, Brigita Slavec, Ljiljana Bedrica, S. Žužul and D. Gračner Introduction Feline chlamydiosis is a disease in do- Rampazzo et al. (2003) investigated mestic cats caused by Chlamydophila felis the prevalence of Cp. felis and feline (Cp. felis), which is primarily a pathogen herpesvirus in cats with conjunctivitis by of the conjunctiva and nasal mucosa using a conventional polymerase chain rather than a pulmonary pathogen. It is reaction (PCR), and discovered that 14 capable of causing acute to chronic con- out of 70 (20%) cats with conjunctivitis junctivitis, with blepharospasm, chem- were positive only on Cp. felis and mixed osis and congestion, a serous to mucop- infections with herpesvirus were present urulent ocular discharge, and rhinitis in 5 of 70 (7%) cats. (Hoover et al., 1978; Sykes, 2005). C. Helps et al. (2005) took oropharyngeal 1 psittaci infection in kittens produces fe- and conjunctival swabs from 1101 cats ver, lethargy, lameness, and reduction and by using a PCR determined Cp. felis in weight gain (Terwee at al., 1998). Ac- in 10% of the 558 swab samples of cats cording to the literature, chlamydiosis with URDT and in 3% of the 558 swab in cats can be treated successfully by samples of cats without URDT. administering potentiated amoxicillin Low et al. (2007) investigated 55 cats for 30 days, which can result in a com- with conjunctivitis, 39 healthy cats and plete clinical recovery with no evidence 32 cats with a history of conjunctivitis of a recurrence for six months (Sturgess that been resolved for at least 3 months. -

WHO GUIDELINES for the Treatment of Treponema Pallidum (Syphilis)
WHO GUIDELINES FOR THE Treatment of Treponema pallidum (syphilis) WHO GUIDELINES FOR THE Treatment of Treponema pallidum (syphilis) WHO Library Cataloguing-in-Publication Data WHO guidelines for the treatment of Treponema pallidum (syphilis). Contents: Web annex D: Evidence profiles and evidence-to-decision frameworks - Web annex E: Systematic reviews for syphilis guidelines - Web annex F: Summary of conflicts of interest 1.Syphilis – drug therapy. 2.Treponema pallidum. 3.Sexually Transmitted Diseases. 4.Guideline. I.World Health Organization. ISBN 978 92 4 154980 6 (NLM classification: WC 170) © World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/ copyright_form/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Chlamydia Trachomatis Infection Is Driven by Nonprotective Immune Cells That Are Distinct from Protective Populations
Pathology after Chlamydia trachomatis infection is driven by nonprotective immune cells that are distinct from protective populations Rebeccah S. Lijeka,b,1, Jennifer D. Helblea, Andrew J. Olivea,c, Kyra W. Seigerb, and Michael N. Starnbacha,1 aDepartment of Microbiology and Immunobiology, Harvard Medical School, Boston, MA 02115; bDepartment of Biological Sciences, Mount Holyoke College, South Hadley, MA 01075; and cDepartment of Microbiology and Physiological Systems, University of Massachusetts Medical School, Worcester, MA 01605 Edited by Rafi Ahmed, Emory University, Atlanta, GA, and approved December 27, 2017 (received for review June 23, 2017) Infection with Chlamydia trachomatis drives severe mucosal immu- sequence identity, Chlamydia muridarum, the extent to which the nopathology; however, the immune responses that are required for molecular pathogenesis of C. muridarum represents that of Ct is mediating pathology vs. protection are not well understood. Here, unknown (6). Ct serovar L2 (Ct L2) is capable of infecting the we employed a mouse model to identify immune responses re- mouse upper genital tract when inoculated across the cervix into quired for C. trachomatis-induced upper genital tract pathology the uterus (7, 8) but it does not induce robust immunopathology. and to determine whether these responses are also required for This is consistent with the human disease phenotype caused by Ct L2, bacterial clearance. In mice as in humans, immunopathology was which disseminates to the lymph nodes causing lymphogranuloma characterized by extravasation of leukocytes into the upper genital venereum (LGV) and is not a major cause of mucosal immunopa- thology in the female upper genital tract (uterus and ovaries). tract that occluded luminal spaces in the uterus and ovaries.