Discrepancies in Reporting the CAG Repeat Lengths for Huntington&Apos
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
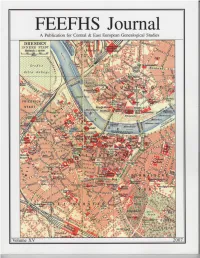
FEEFHS Journal Volume 15, 2007
FEEFHS Journal Volume 15, 2007 FEEFHS Journal Who, What and Why is FEEFHS? The Federation of East European Family History Societies Guest Editor: Kahlile B. Mehr. [email protected] (FEEFHS) was founded in June 1992 by a small dedicated group of Managing Editor: Thomas K. Edlund American and Canadian genealogists with diverse ethnic, religious, and national backgrounds. By the end of that year, eleven societies FEEFHS Executive Council had accepted its concept as founding members. Each year since then FEEFHS has grown in size. FEEFHS now represents nearly two 2006-2007 FEEFHS officers: hundred organizations as members from twenty-four states, five Ca- President: Dave Obee, 4687 Falaise Drive, Victoria, BC V8Y 1B4 nadian provinces, and fourteen countries. It continues to grow. Canada. [email protected] About half of these are genealogy societies, others are multi- 1st Vice-president: Brian J. Lenius. [email protected] purpose societies, surname associations, book or periodical publish- 2nd Vice-president: Lisa A. Alzo ers, archives, libraries, family history centers, online services, insti- 3rd Vice-president: Werner Zoglauer tutions, e-mail genealogy list-servers, heraldry societies, and other Secretary: Kahlile Mehr, 412 South 400 West, Centerville, UT. ethnic, religious, and national groups. FEEFHS includes organiza- [email protected] tions representing all East or Central European groups that have ex- Treasurer: Don Semon. [email protected] isting genealogy societies in North America and a growing group of worldwide organizations and individual members, from novices to Other members of the FEEFHS Executive Council: professionals. Founding Past President: Charles M. Hall, 4874 S. 1710 East, Salt Lake City, UT 84117-5928 Goals and Purposes: Immediate Past President: Irmgard Hein Ellingson, P.O. -

Obituary Index 3Dec2020.Xlsx
Last First Other Middle Maiden ObitSource City State Date Section Page # Column # Notes Naber Adelheid Carrollton Gazette Carrolton IL 9/26/1928 1 3 Naber Anna M. Carrollton Gazette Patriot Carrolton IL 9/23/1960 1 2 Naber Bernard Carrollton Gazette Carrolton IL 11/17/1910 1 6 Naber John B. Carrollton Gazette Carrolton IL 6/13/1941 1 1 Nace Joseph Lewis Carthage Republican Carthage IL 3/8/1899 5 2 Nachtigall Elsie Meler Chicago Daily News Chicago IL 3/27/1909 15 1 Nachtigall Henry C. Chicago Daily News Chicago IL 11/30/1909 18 4 Nachtigall William C. Chicago Daily News Chicago IL 10/5/1925 38 3 Nacke Mary Schleper Effingham Democrat Effingham IL 8/6/1874 3 4 Nacofsky Lillian Fletcher Chicago Daily News Chicago IL 2/22/1922 29 1 Naden Clifford Kendall County Journal Yorkville IL 11/8/1990 Countywide 2 2 Naden Earl O. Waukegan News Sun Waukegan IL 11/2/1984 7A 4 Naden Elizabeth Broadbent Kendall County Journal Yorkville IL 1/17/1900 8 4 Naden Isaac Kendall County Journal Yorkville IL 2/28/1900 4 1 Naden James Darby Kendall County Journal Yorkville IL 12/25/1935 4 5 Naden Jane Green Kendall County Journal Yorkville IL 4/10/1912 9 3 Naden John M. Kendall County Journal Yorkville IL 9/13/1944 5 4 Naden Martha Kendall County Journal Yorkville IL 12/6/1866 3 1 Naden Obadiah Kendall County Journal Yorkville IL 11/8/1911 1 1 Naden Samuel Kendall County Journal Yorkville IL 6/17/1942 7 1 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/15/1878 4 3 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/8/1878 1 4 Naden Thomas Kendall County -

PDF EPUB} La Pallacanestro Di Vittorio Tracuzzi by Gaetano Gebbia La Pallacanestro Di Vittorio Tracuzzi by Gaetano Gebbia
Read Ebook {PDF EPUB} La pallacanestro di Vittorio Tracuzzi by Gaetano Gebbia La pallacanestro di Vittorio Tracuzzi by Gaetano Gebbia. Reading is a golden bridge us to know the contents of the world without us how to get there. one we have to read is PDF La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale Download because we will be presented with the contents of the content that we do not know. So that we will be adding new things education. if you do not have time to look for La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Online then you can visit our website so you do not need to go to the bookstore to mencar La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Kindle . So you can save money and your time for other activities. Read and Download Ebook Full Book La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF PDF. Full Book La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Online PDF. Full Book PDF La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale Download By . aine. PDF File: Full . Download La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Rach. EPUB MOBI AZW3 Kindle PDF Ebook Download. Gina Royal is the definition of average shy Midwestern . Editorial Reviews. Review. In this rapid-fire thriller. Caine spins a powerful story of maternal . .com: PDF La pallacanestro di Vittorio Tracuzzi. -

HAVING REGARD to the Regulation of the Politecnico Di Bari Concerning Ph.D
Rector’s Decree n. 662 THE RECTOR GIVEN THE Statute of Politecnico di Bari issued with Rectoral Decree n. 175/2019; HAVING REGARD TO the Regulation of the Politecnico di Bari concerning Ph.D. programs, issued with Rector’s Decree n. 286 dated July 1, 2013; HAVING REGARD TO the Italian Ministerial-Director Decree dated 13/09/2019, n. 1747, Call MIUR PON RI FSE-FESR “Research and Innovation 2014-2020” Action I.1 “Industry oriented Innovative Ph. D. programs for the Academic year 2019-2020, which aims at promoting and strengthening doctoral studies consistently with the needs of the national industrial system and with the Italian strategy for smart specialization 2014-2020 supported by the European Committee by means of additional doctoral scholarships and their actuation protocol; HAVING REGARD TO the Dean Decree n. 68/2019 about the appointment of the selection Committee for the admission to Ph.D. in ELECTRICAL AND INFORMATION ENGINEERING - XXXV cycle; HAVING REGARD TO the Dean Decree n. 24/2019 about the appointment of the selection Committee for the admission to Ph.D. in DESIGN FOR HERITAGE: KNOWLEDGE AND LANDSCAPE - XXXV cycle; HAVING REGARD TO the Dean Decree n. 67/2019 about the appointment of the selection Committee for the admission to Ph.D. in MECHANICAL ENGINEERING AND MANAGEMENT - XXXV cycle; HAVING REGARD TO the Dean Decree n. 51/2019 about the appointment of the selection Committee for the admission to Ph.D. in RISK AND ENVIRONMENTAL, TERRITORIAL AND BUILDING DEVELOPMENT - XXXV cycle; HAVING REGARD TO minutes of the selection Committees about results of the evaluation for admission the above-mentioned Ph.D. -

Año XVII. Núm. 17. Madrid 1º De Mayo De 1873
YL AMERICANA I# ¡ i i fìssisi '¡YLV: ensñlA , í^fW< iw^in IMiKGlUS DE 5¿ L'SGHlClnN. AÑO XVII.— NÛM. XVII. l'llK C lO * DF. SL'SCRTCION. aS". 5KMKf*TH£. TWMKMíllE. M.MF.STRK. Dinr.r.i"n-PR('1'IKT.M:I,|. D. ABELARDO DE CARLOS 12 7 3 5 pesetas. 18 pesetas. l(i pesetas. (.’uba y Pucrtn-Ilico.. pesos fnortes. pesos fuertes. Madrid............... AD.MIM'JIl.UiuX, CARRETAS, 12, I'KINCII'AL. Provincia?........... 4 0 id. 20 id. 11 id Filipinas...................... 15 iil. 8 id. 4 .3 0 0 2 .3 0 0 veis. Portugal.. 8 .4 0 0 veis. reís. Madrid, I." dr Mavì» de 1 8 7 3 . Eu lus demas Americas lijan el precio los Fres. Agentes. SUMARIO. iiiiiiginc-c lo ij»io .-era el nuestro, i|Uc la tiene tan rica y variada; tan Im o .—Tlr vbta ironrnil , pur i l Murrini* rte V 1 cumula di toda clase de aconteci Ue.Alcrrp. — Xuestro» pruhuilos, por I». Ku-> Ilio Martine?, «le Vrliwe — Ìtobenn Robert, miento:?. por D. Eu-ajbio Rla?e(>.—Vitijr nlrfilcd"-r tir- hi Desde laanicrior Revista, ¡ cuán Exposlclon imi vorrai ili Vionn. por un Cnbntlc-: to-, etniu graves y trascendentales ro Espiulòl.—lìitHiriifiii dii Uni un «le l.t-bii,'. p u D. II. T. Malie/, il»* Lumi'.—ìli ” ini ¡ui- lian oí niTuie en él ! ¡ Cómo lia cam tiguo mitigo 1.1. .lumi Multino/. Villcvgtvs.pov inado la faz «le las cosas! ¡Cómo se D. Munuol Juan Diluiti.— HI -nrnoilc un cuento (coiiclliilon). por Carlini Rublo.—Kii Iti han complicado y envenenado todas orlili»del mar, poe-ai, pi.r le Ju. -

Akron Beacon Journal
AKRON BEACON JOURNAL Index to Obituaries 1962 - 1979 M-N Compiled by the staff of the -anguage, Literature and History Division, Akron-Summit County Public Library NAME DRTE DBIT WP M. Alice Sister '3- 1 9-79 Maag , Byron H: 4-1 9-78 Maag, Carl 9- 1-66 Maag , Clarence 4-6-68 Maag, Ida C. 2-7-62 hag, John J. 7-24-76 Maag. Myrtle L. 7- 15-72 Maag. Oris L. 6-1 8-79 Maag, Wally 8-27-69 Maag. William H. 9-1 4-77 Maahs, Anna 16-27-68 flaahs, Louise 5-20-76 . Maahs. Pearl 7-9-78 Maahs. Robert H. 4-9-79 Maahs, William 5-20-67 Maas, Behrend 12-3-68 Maas. Calla 2-15-62 Maas. Paul 4-23-73 Maass, Elda 1-24-79 Maass, Elda C. 1-4-78 Mabe. Ada M. 11-16-64 Mabe, Lloyd P. 12-1 9-62 Mabius, Frank 6. 6- 12-73 Mabius, Marht.a 4-30-73 Mable, Ruth L. 12-2-63 flabry , Alonzo 1-22-78 Mabry. Donald D. 5-8-78 Mabry, Edwin A. 3- 13-70 Mabry, Hazel I. 6-1 -64 Mabry. Henry H. 7-24-69 Mabry , Lizzie 4-27-63 Mabry. Raymond L. 8-12-71 Mabry, Winnefred J. 8-30-76 MacAdam. Joseph E.L. 9-1 1-74 Macelone, Dorothy 12-1 2-75 Macale, Mary 6-19-71 Macale, Thomas 7-2-7 I ' Macaluso, Antonia 1-1 9-71 Macaluso, Frank 3-1 7-65 . Macaluso, Rose 6-6-66 Macaluso, Thomas J. -

Download a Certificate of Recognition Directly from Our Submission System
Editorial Acknowledgement to Reviewers of Forests in 2016 Forests Editorial Office Published: 11 January 2017 MDPI AG, St. Alban-Anlage 66, 4052 Basel, Switzerland; [email protected] The editors of Forests would like to express their sincere gratitude to the following reviewers for assessing manuscripts in 2016. We greatly appreciate the contribution of expert reviewers, which is crucial to the journal’s editorial process. We aim to recognize reviewer contributions through several mechanisms, of which the annual publication of reviewer names is one. Reviewers receive a voucher entitling them to a discount on their next MDPI publication and can download a certificate of recognition directly from our submission system. Additionally, reviewers can sign up to the service Publons (https://publons.com) to receive recognition. Of course, in these intiatives we are careful not to compromise reviewer confidentiality. Many reviewers see their work as a voluntary and often unseen part of their role as researchers. We are grateful to the time reviewers donate to our journals and the contribution they make. If you are interested in becoming a reviewer for Forests, see the link at the bottom of the webpage http://www.mdpi.com/reviewers. The following reviewed for Forests in 2016: Abbas, Sawaid Arias-Rodil, Manuel Bazot, Stéphane Adams, Mary Beth Armenteras-Pascual, Dolors Belbo, Helmer Agnoletti, Mauro Arnold, Sven Bell, F. Wayne Ågren, Göran I. Arp, Paul Ben-Dov, Iddo Z. Aguirre-Gutiérrez, Jesús Artlip, Timothy Bennett, Joanne M. Aitken, Sally N Aruga, Kazuhiro Berhongaray, Gonzalo Alam, Ashraful Asao, Shinichi Berland, Adam Alcasena, Fermín J. Asplund, Johan Berner, Logan Alexander, Peter Asselin, Hugo Berrill, Pascal Alía, Ricardo Atangana, Alain R. -

Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi University of Wisconsin-Milwaukee, [email protected]
University of Wisconsin Milwaukee UWM Digital Commons French, Italian and Comparative Literature Faculty French, Italian and Comparative Literature Books Department 2019 Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi University of Wisconsin-Milwaukee, [email protected] Follow this and additional works at: https://dc.uwm.edu/freita_facbooks Part of the Criminology and Criminal Justice Commons, Italian Language and Literature Commons, and the Women's Studies Commons Recommended Citation Pickering-Iazzi, Robin, "Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018" (2019). French, Italian and Comparative Literature Faculty Books. 2. https://dc.uwm.edu/freita_facbooks/2 This Book is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in French, Italian and Comparative Literature Faculty Books by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. DEAD SILENT: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi Robin Pickering-Iazzi is Professor of Italian and Comparative Literature in the Department of French, Italian, and Comparative Literature at the University of Wisconsin-Milwaukee. She is the author of The Mafia in Italian Lives and Literature: Life Sentences and Their Geographies, published in Italian as Le geografie della mafia nella vita e nella letteratura dell’Italia contemporanea, and editor of the acclaimed volumes The Italian Antimafia, New Media, and the Culture of Legality and Mafia and Outlaw Stories in Italian Life and Literature. She is currently working on a book that examines representations of feminicide in Italian literature, film, and media. -
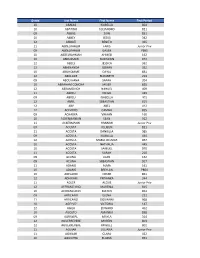
Grade Last Name First Name First Period 10 ABADIA ISABELLA 804
Grade Last Name First Name First Period 10 ABADIA ISABELLA 804 10 ABATINO ALEJANDRO 821 09 ABBAS ZAIN 851 10 ABBEY JESUS 342 12 ABBIATI BENITO 365 11 ABDELRAHEM FARIS Junior Priv 09 ABDELRAHEM GASIM P865 10 ABDELRAHMAN AHMED 162 10 ABDUSSAMI TAISHAWN 972 12 ABELS JESSICA 362 12 ABHINANDA GOWRI 352 10 ABILHOMME DAYAL 831 12 ABOLADE ELIZABETH 213 09 ABOU HANA SARAH 204 10 ABRAHAM CONCHA JAVIER 835 12 ABRAMOVICH NAHUEL 409 11 ABREU DIEGO 429 09 ABREU ISABELLA 401 12 ABRIL SEBASTIAN 815 12 ABY ABEL 412 12 ACEVEDO CAMILA 855 09 ACHARYA VIHAAN 160 10 ACKERMANIAN SEAN 912 11 ACKERMANN HANNAH Junior Priv 09 ACOSTA ALLISON 821 11 ACOSTA DANIELLA 985 09 ACOSTA ISABELLA 434 12 ACOSTA MARIA DELMAR 857 10 ACOSTA NATHALIA 445 10 ACOSTA SAMUEL 970 11 ACOSTA SARAH 210 09 ACUNA JUAN 162 09 ACUNA SEBASTIAN 917 11 ADAMS ALMA 161 10 ADAMS BREYLAN P864 10 ADELARDI OMAR 851 12 ADHIKARI PRIYANKA 344 11 ADLER ALEXIS Junior Priv 12 AFFRANCHINO MARTINA 815 10 AFFRANCHINO MATEO 853 09 AFRICANO ELENA 222 11 AFRICANO GIOVANNI 968 10 AGELVIZ VICTORIA 147 12 AGILA EDWARD 452 10 AGOSTO AMANDA 858 09 AGRAWAL MAYLA 314 12 AGUERREVERE MARTIN 803 12 AGUERREVERE MIGUEL 802 11 AGUIAR JULIANA Junior Priv 11 AGUILAR CLARA 422 10 AGUILERA ELAINA 951 Grade Last Name First Name First Period 11 AGUINAGA VELA GABRIELA 957 09 AGUIRRE CHRISTIAN 413 10 AGUIRRE DANIEL 419 12 AGUIRRE DIEGO 437 12 AGUIRRE JASON 223 11 AGUIRRE SARAVIA FRANCO 210 12 AHN JOSHUA 421 11 AIAZZI XIOMARA 445 12 AIKEN NICHOLAS 178 10 AIKMAN CORDELL 948 11 AILDASANI JULIA 340 11 AILDASANI RAPHAELA 854 09 AIRES RADA -

Nomenclature of Taxa of the Order Actinomycetales (Schizomycetes) Erwin Francis Lessel Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1961 Nomenclature of taxa of the order Actinomycetales (Schizomycetes) Erwin Francis Lessel Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Microbiology Commons Recommended Citation Lessel, Erwin Francis, "Nomenclature of taxa of the order Actinomycetales (Schizomycetes) " (1961). Retrospective Theses and Dissertations. 2440. https://lib.dr.iastate.edu/rtd/2440 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. This dissertation has been (J 1-3042 microfilmed exactly as received LESSEL, Jr., iJrxvin Francis, 1U3U- NOMENCLATURE OF TAXA OF THE ORUEIR AC TINO M YC E TA LE S (SCIIIZO M YC ETES). Iowa State University of Science and Technology Ph.D., 1001 Bacteriology University Microfilms, Inc., Ann Arbor, Mic hi g NOMENCLATURE OF TAXA OF THE ORDKR ACTINOMYCETALES (SCHIZOMYCETES) oy Erwin Francis Lessel, Jr. A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY Ma-'or Subject: Bacteriology Approved: Signature was redacted for privacy. In Charge of Major Work Signature was redacted for privacy. -

The Best of Youth (La Meglio Gioventù)
Rai Radiotelevisione Italiana presents a film by MARCO TULLIO GIORDANA The Best of Youth (La Meglio Gioventù) written by SANDRO PETRAGLIA and STEFANO RULLI produced by ANGELO BARBAGALLO a Rai Fiction production realized by BìBì Film Tv international distribution Rai Trade Technical Cast Cast The plot Director Marco Tullio Giordana Nicola Carati Luigi Lo Cascio La Meglio Gioventù tells the story of an Italian family from the end Screenplay Sandro Petraglia Matteo Carati Alessio Boni Stefano Rulli Adriana Carati Adriana Asti of the 60s till nowadays. The lives of two brothers, Nicola and Matteo, Director of Photography Roberto Forza Giulia Monfalco Sonia Bergamasco are the heart of the story. At first they share the same dreams, the Camera Operator Vincenzo Carpineta Carlo Tommasi Fabrizio Gifuni same hopes, the same books and friendships. Meeting Giorgia, a girl 1st Assistant Director and Casting Barbara Melega Mirella Utano Maya Sansa Production Designer Franco Ceraolo Francesca Carati Valentina Carnelutti with mental disorders, will be determinant for the future of the two Costume Designer Elisabetta Montaldo Giorgia Jasmine Trinca brothers: Nicola decides to become a psychiatrist, Matteo abandons Sound Designer Fulgenzio Ceccon Angelo Carati Andrea Tidona his studies and joins the police. Boom Operator Decio Trani Giovanna Carati Lidia Vitale Angelo – the father – is a loving parent and husband. The family Film Editor Roberto Missiroli a.m.c. Sara Carati Camilla Filippi Sara Carati 8 years Greta Cavuoti experiences his exuberance with tolerant complaisance. Adriana – General Organizer Gianfranco Barbagallo Sara Carati 5 years Sara Pavoncello the mother – is a modern and irreproachable teacher, who loves her Executive Producer Alessandro Calosci Vitale Micavi Claudio Gioè pupils like her own children. -
Last Name First Name Middle Name Years of Service A
UNCLAIMED CAPITAL CREDITS - UPDATED 4/16/2020 LAST NAME FIRST NAME MIDDLE NAME YEARS OF SERVICE A BETTER IMAGE PRINTING 1992-1989 ABAR JOHN M 1992-1988 ABAYHAN RASIT R 1992-1988 ABBATE PAUL 1992-1988 ABBOTT LUTHER D 1992-1988 ABBOTT JOYCE 1990-1988 ABBOTT CHRISTOPH 1990-1988 ABBOTT DARBY LEE 1991-1989 ABDELUARIM HANI O 1992-1991 ABERNETHY DARRELL F 1992-1991 ABERNETHY ROBIN ELIZABETH 1992-1988 ABERNETHY WILLIAM RHYNE 1992-1989 ABRAHAM MARY BETH 1991-1988 ABRAMS LEW J 1990-1988 ABRAMS KATHLEEN 1989-1988 ABSHEAR J DAVID 1991-1989 ABT LYNETTE MARIE 1991-1989 ACKERMAN STEPHEN D 1991 ACOSTA MONIQUE E 1990-1988 ACREE RUDOLPH 1992-1989 ACREY PHILLIP CLINTON 1992-1988 ADAME ALFREDO A 1990-1989 ADAMS P B 1991 ADAMS RICHARD 1989-1988 ADAMS GLENN 1990-1988 ADAMS MALLIE 1991-1989 ADAMS DAVID ROBERT 1990-1989 ADAMS LARA JEANE 1991 ADAMS KIMBERLY ELAINE 1991-1989 ADAMS CHRISTOPH ALLEN 1991-1989 ADAMS PAMELA SUE 1992-1991 ADAMS COLLEEN 1992-1991 ADAMS HOWARD ANTHONY 1989-1988 ADAMS FLOYD E 1992-1988 ADAMS KELLY N 1991-1988 ADCOCK DOROTHY A 1992-1988 ADDISON ANDREW JOHN 1991-1989 ADKINS WANDA P 1992-1989 ADORNETTO LISA JO 1990-1988 AFFERICA TODD 1989-1988 AGNER JOHN MICHAEL 1990-1988 AGOSTI DIANE LEIGH 1990-1989 AHERN ELLEN L 1990-1988 AIBEL JEFFREY B 1990-1988 AIELW JOSEPH R 1992 AIKEN TIM J 1990-1989 AINSWORTH W E 1989-1988 AKERS TERESA B 1991-1988 AKINBI HENRY & 1991-1989 AKINS LEANNE L 1990-1988 ALBANO KRISTI LEE 1991 ALBERT GABRIELLE 1991-1989 ALBERT JAMES FRED 1992-1988 ALBRIGHT STEPHEN JAMES 1992-1989 ALBRIGHT SUSAN EVANS 1992 ALBRO CHRISTOPH