How Would You Manage This Prolapse?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Different Influences of Endometriosis and Pelvic Inflammatory Disease On
International Journal of Environmental Research and Public Health Article Different Influences of Endometriosis and Pelvic Inflammatory Disease on the Occurrence of Ovarian Cancer Jing-Yang Huang 1,2,†, Shun-Fa Yang 1,2 , Pei-Ju Wu 1,3,†, Chun-Hao Wang 4,†, Chih-Hsin Tang 5,6,7 and Po-Hui Wang 1,2,3,8,* 1 Institute of Medicine, Chung Shan Medical University, Taichung 402, Taiwan; [email protected] (J.-Y.H.); [email protected] (S.-F.Y.); [email protected] (P.-J.W.) 2 Department of Medical Research, Chung Shan Medical University Hospital, Taichung 402, Taiwan 3 Department of Obstetrics and Gynecology, Chung Shan Medical University Hospital, Taichung 402, Taiwan 4 Department of Medicine, National Taiwan University, Taipei 106, Taiwan; [email protected] 5 School of Medicine, China Medical University, Taichung 404, Taiwan; [email protected] 6 Chinese Medicine Research Center, China Medical University, Taichung 404, Taiwan 7 Department of Medical Laboratory Science and Biotechnology, College of Medical and Health Science, Asia University, Taichung 413, Taiwan 8 School of Medicine, Chung Shan Medical University, Taichung 402, Taiwan * Correspondence: [email protected] † Equal contributions as first authors. Abstract: To compare the rate and risk of ovarian cancer in patients with endometriosis or pelvic inflammatory disease (PID). A nationwide population cohort research compared the risk of ovarian cancer in 135,236 age-matched comparison females, 114,726 PID patients, and 20,510 endometriosis patients out of 982,495 females between 1 January 2002 and 31 December 2014 and ended on the date Citation: Huang, J.-Y.; Yang, S.-F.; of confirmation of ovarian cancer, death, or 31 December 2014. -
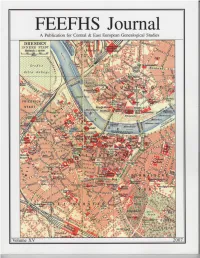
FEEFHS Journal Volume 15, 2007
FEEFHS Journal Volume 15, 2007 FEEFHS Journal Who, What and Why is FEEFHS? The Federation of East European Family History Societies Guest Editor: Kahlile B. Mehr. [email protected] (FEEFHS) was founded in June 1992 by a small dedicated group of Managing Editor: Thomas K. Edlund American and Canadian genealogists with diverse ethnic, religious, and national backgrounds. By the end of that year, eleven societies FEEFHS Executive Council had accepted its concept as founding members. Each year since then FEEFHS has grown in size. FEEFHS now represents nearly two 2006-2007 FEEFHS officers: hundred organizations as members from twenty-four states, five Ca- President: Dave Obee, 4687 Falaise Drive, Victoria, BC V8Y 1B4 nadian provinces, and fourteen countries. It continues to grow. Canada. [email protected] About half of these are genealogy societies, others are multi- 1st Vice-president: Brian J. Lenius. [email protected] purpose societies, surname associations, book or periodical publish- 2nd Vice-president: Lisa A. Alzo ers, archives, libraries, family history centers, online services, insti- 3rd Vice-president: Werner Zoglauer tutions, e-mail genealogy list-servers, heraldry societies, and other Secretary: Kahlile Mehr, 412 South 400 West, Centerville, UT. ethnic, religious, and national groups. FEEFHS includes organiza- [email protected] tions representing all East or Central European groups that have ex- Treasurer: Don Semon. [email protected] isting genealogy societies in North America and a growing group of worldwide organizations and individual members, from novices to Other members of the FEEFHS Executive Council: professionals. Founding Past President: Charles M. Hall, 4874 S. 1710 East, Salt Lake City, UT 84117-5928 Goals and Purposes: Immediate Past President: Irmgard Hein Ellingson, P.O. -

Obituary Index 3Dec2020.Xlsx
Last First Other Middle Maiden ObitSource City State Date Section Page # Column # Notes Naber Adelheid Carrollton Gazette Carrolton IL 9/26/1928 1 3 Naber Anna M. Carrollton Gazette Patriot Carrolton IL 9/23/1960 1 2 Naber Bernard Carrollton Gazette Carrolton IL 11/17/1910 1 6 Naber John B. Carrollton Gazette Carrolton IL 6/13/1941 1 1 Nace Joseph Lewis Carthage Republican Carthage IL 3/8/1899 5 2 Nachtigall Elsie Meler Chicago Daily News Chicago IL 3/27/1909 15 1 Nachtigall Henry C. Chicago Daily News Chicago IL 11/30/1909 18 4 Nachtigall William C. Chicago Daily News Chicago IL 10/5/1925 38 3 Nacke Mary Schleper Effingham Democrat Effingham IL 8/6/1874 3 4 Nacofsky Lillian Fletcher Chicago Daily News Chicago IL 2/22/1922 29 1 Naden Clifford Kendall County Journal Yorkville IL 11/8/1990 Countywide 2 2 Naden Earl O. Waukegan News Sun Waukegan IL 11/2/1984 7A 4 Naden Elizabeth Broadbent Kendall County Journal Yorkville IL 1/17/1900 8 4 Naden Isaac Kendall County Journal Yorkville IL 2/28/1900 4 1 Naden James Darby Kendall County Journal Yorkville IL 12/25/1935 4 5 Naden Jane Green Kendall County Journal Yorkville IL 4/10/1912 9 3 Naden John M. Kendall County Journal Yorkville IL 9/13/1944 5 4 Naden Martha Kendall County Journal Yorkville IL 12/6/1866 3 1 Naden Obadiah Kendall County Journal Yorkville IL 11/8/1911 1 1 Naden Samuel Kendall County Journal Yorkville IL 6/17/1942 7 1 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/15/1878 4 3 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/8/1878 1 4 Naden Thomas Kendall County -

PDF EPUB} La Pallacanestro Di Vittorio Tracuzzi by Gaetano Gebbia La Pallacanestro Di Vittorio Tracuzzi by Gaetano Gebbia
Read Ebook {PDF EPUB} La pallacanestro di Vittorio Tracuzzi by Gaetano Gebbia La pallacanestro di Vittorio Tracuzzi by Gaetano Gebbia. Reading is a golden bridge us to know the contents of the world without us how to get there. one we have to read is PDF La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale Download because we will be presented with the contents of the content that we do not know. So that we will be adding new things education. if you do not have time to look for La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Online then you can visit our website so you do not need to go to the bookstore to mencar La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Kindle . So you can save money and your time for other activities. Read and Download Ebook Full Book La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF PDF. Full Book La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Online PDF. Full Book PDF La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale Download By . aine. PDF File: Full . Download La pallacanestro di Vittorio Tracuzzi. L'interprete geniale di un basket attuale PDF Rach. EPUB MOBI AZW3 Kindle PDF Ebook Download. Gina Royal is the definition of average shy Midwestern . Editorial Reviews. Review. In this rapid-fire thriller. Caine spins a powerful story of maternal . .com: PDF La pallacanestro di Vittorio Tracuzzi. -

Understanding Endometriosis - Information Pack
Understanding Endometriosis - Information Pack What is endometriosis? Endometriosis (pronounced en- doh – mee – tree – oh – sis) is the name given to the condition where cells like the ones in the lining of the womb (uterus) are found elsewhere in the body. Every month a woman’s body goes through hormonal changes. Hormones are naturally released which cause the lining of the womb to increase in preparation for a fertilized egg. If pregnancy does not occur, this lining will break down and bleed – this is then released from the body as a period. Endometriosis cells react in the same way – except that they are located outside the womb. During the monthly cycle hormones stimulate the endometriosis, causing it to grow, then break down and bleed. This internal bleeding, unlike a period, has no way of leaving the body. This leads to inflammation, pain, and the formation of scar tissue (adhesions). Endometriosis is not an infection. Endometrial tissue can also be found in the ovary, Endometriosis is not contagious. where it can form cysts, called ‘chocolate cysts’ Endometriosis is not cancer. because of their appearance. Endometriosis is most commonly found inside the pelvis, around the ovaries, the fallopian tubes, on the outside of the womb or the ligaments (which hold the womb in place), or the area between your rectum and your womb, called the Pouch of Douglas. It can also be found on the bowel, the bladder, the intestines, the vagina and the rectum. You can also have endometrial tissue that grows in the muscle layer of the wall of the womb (this is another condition called adenomyosis). -

Differential Diagnosis of Endometriosis by Ultrasound
diagnostics Review Differential Diagnosis of Endometriosis by Ultrasound: A Rising Challenge Marco Scioscia 1 , Bruna A. Virgilio 1, Antonio Simone Laganà 2,* , Tommaso Bernardini 1, Nicola Fattizzi 1, Manuela Neri 3,4 and Stefano Guerriero 3,4 1 Department of Obstetrics and Gynecology, Policlinico Hospital, 35031 Abano Terme, PD, Italy; [email protected] (M.S.); [email protected] (B.A.V.); [email protected] (T.B.); [email protected] (N.F.) 2 Department of Obstetrics and Gynecology, “Filippo Del Ponte” Hospital, University of Insubria, 21100 Varese, VA, Italy 3 Obstetrics and Gynecology, University of Cagliari, 09124 Cagliari, CA, Italy; [email protected] (M.N.); [email protected] (S.G.) 4 Department of Obstetrics and Gynecology, Azienda Ospedaliero Universitaria, Policlinico Universitario Duilio Casula, 09045 Monserrato, CA, Italy * Correspondence: [email protected] Received: 6 October 2020; Accepted: 15 October 2020; Published: 20 October 2020 Abstract: Ultrasound is an effective tool to detect and characterize endometriosis lesions. Variances in endometriosis lesions’ appearance and distorted anatomy secondary to adhesions and fibrosis present as major difficulties during the complete sonographic evaluation of pelvic endometriosis. Currently, differential diagnosis of endometriosis to distinguish it from other diseases represents the hardest challenge and affects subsequent treatment. Several gynecological and non-gynecological conditions can mimic deep-infiltrating endometriosis. For example, abdominopelvic endometriosis may present as atypical lesions by ultrasound. Here, we present an overview of benign and malignant diseases that may resemble endometriosis of the internal genitalia, bowels, bladder, ureter, peritoneum, retroperitoneum, as well as less common locations. An accurate diagnosis of endometriosis has significant clinical impact and is important for appropriate treatment. -

HAVING REGARD to the Regulation of the Politecnico Di Bari Concerning Ph.D
Rector’s Decree n. 662 THE RECTOR GIVEN THE Statute of Politecnico di Bari issued with Rectoral Decree n. 175/2019; HAVING REGARD TO the Regulation of the Politecnico di Bari concerning Ph.D. programs, issued with Rector’s Decree n. 286 dated July 1, 2013; HAVING REGARD TO the Italian Ministerial-Director Decree dated 13/09/2019, n. 1747, Call MIUR PON RI FSE-FESR “Research and Innovation 2014-2020” Action I.1 “Industry oriented Innovative Ph. D. programs for the Academic year 2019-2020, which aims at promoting and strengthening doctoral studies consistently with the needs of the national industrial system and with the Italian strategy for smart specialization 2014-2020 supported by the European Committee by means of additional doctoral scholarships and their actuation protocol; HAVING REGARD TO the Dean Decree n. 68/2019 about the appointment of the selection Committee for the admission to Ph.D. in ELECTRICAL AND INFORMATION ENGINEERING - XXXV cycle; HAVING REGARD TO the Dean Decree n. 24/2019 about the appointment of the selection Committee for the admission to Ph.D. in DESIGN FOR HERITAGE: KNOWLEDGE AND LANDSCAPE - XXXV cycle; HAVING REGARD TO the Dean Decree n. 67/2019 about the appointment of the selection Committee for the admission to Ph.D. in MECHANICAL ENGINEERING AND MANAGEMENT - XXXV cycle; HAVING REGARD TO the Dean Decree n. 51/2019 about the appointment of the selection Committee for the admission to Ph.D. in RISK AND ENVIRONMENTAL, TERRITORIAL AND BUILDING DEVELOPMENT - XXXV cycle; HAVING REGARD TO minutes of the selection Committees about results of the evaluation for admission the above-mentioned Ph.D. -

Women's Health
Women’s Health Kristen Jones, DO Osteopathic Faculty St. Luke’s Family Medicine Residency Bethlehem, PA ACOFP exam • Women’s Issues (4% of test – OB/GYN = 4%) between 4-6% • Common Topics • Vaginal Discharge • Pelvic Pain • Cancer risk factors • Menstrual disorders • Breast Discharge • Eang disorders • Osteoporosis • HRT • 23 yo with vaginal discharge. Sexually ac[ve. Pelvic exam reveals: • Thin gray-white discharge, pH 5, a strong fishy odor is present when KoH is added to the discharge. • A)Bacterial Vaginosis • B)Gonorrhea • C)Chlamydia • D)Candida • E)Physiologic Discharge • 23 yo with vaginal discharge. Sexually ac[ve. Pelvic exam reveals: • Thin gray-white discharge, pH 5, a strong fishy odor is present when KoH is added to the discharge. • A)Bacterial Vaginosis • B)Gonorrhea • C)Chlamydia • D)Candida • E)Physiologic Discharge Bacterial Vaginosis • pH >4.5 • +Whiff Test • +Clue cells – epithelial cells with adherent bacteria. • Caused by Gardnerella • Treat with Flagyl 500mg po q12hx7 days (safe in pregnancy) • 23 yo with vaginal discharge. Sexually ac[ve. Pelvic exam reveals: • pH <4, vulvar erythema, thick white discharge • Most likely cause is: • A)Bacterial Vaginosis • B)Trichomonas • C)Chlamydia • D)Candida • E)Physiologic Discharge • 23 yo with vaginal discharge. Sexually ac[ve. Pelvic exam reveals: • pH <4.5, vulvar erythema, thick white discharge • Most likely cause is: • A)Bacterial Vaginosis • B)Trichomonas • C)Chlamydia • D)Candida • E)Physiologic Discharge Vaginal Candidiasis • pH <4.5 • Budding yeast and hyphae on KOH • Thick white, chunky discharge • Vulvar erythema and pruri[s • Treat with PO fluconazole 150mg po x1 • Treat with PV clotrimazole or miconazole for 7 days during pregnancy • 23 yo with vaginal discharge. -

Update on Treatment of Menstrual Disorders
THE REPRODUCTIVE YEARS Update on treatment of menstrual disorders Martha Hickey and Cynthia M Farquhar DISTURBANCES OF MENSTRUAL BLEEDING are a major social and medical problem for women, their families and ABSTRACT the health services, and a common reason for women to ■ There is evidence from well designed randomised controlled consult their general practitioners or gynaecologists. In the trials that modern medical and conservative surgical United Kingdom, each year one in 20 women consult their therapies (including endometrial ablation) are effective GPs aboutThe Medical heavy Journal menstrual of Australia bleeding. ISSN:1 0025-729X 16 June treatments for heavy menstrual bleeding for many women. Heavy2003 bleeding178 12 625-629 is the most common menstrual com- ■ Submucous fibroids may be resected directly via the plaint.©The In Medicalmost cases,Journal thisof Australia has no 2003 identifiable www.mja.com.au pelvic or The reproductive years hysteroscope, reducing menstrual bleeding, although data systemic cause and is termed dysfunctional uterine bleed- are available only from case series. ing. Irregular dysfunctional uterine bleeding is generally ■ associated with anovulation. Historically, many women with Endometriosis is common, may also occur in young women heavy menstrual bleeding were advised to undergo hysterec- and may present with atypical or non-cyclical symptoms; tomy, which was the only way of ensuring a “cure”. conservative laparoscopic surgery increases fecundity and However, a range of new and effective interventions can now reduces dysmenorrhoea and dyspareunia. be offered for dysfunctional uterine bleeding and other ■ Randomised trials of the levonorgestrel intrauterine system common causes of menstrual disorder, such as fibroids and in women with menorrhagia have shown that hysterectomy endometriosis. -

Vaginitis and Cervicitis in the Clinic 2009.Pdf
in the clinic Vaginitis and Cervicitis Prevention page ITC3-2 Screening page ITC3-3 Diagnosis page ITC3-5 Treatment page ITC3-10 Practice Improvement page ITC3-14 CME Questions page ITC3-16 Section Co-Editors: The content of In the Clinic is drawn from the clinical information and Christine Laine, MD, MPH education resources of the American College of Physicians (ACP), including Sankey Williams, MD PIER (Physicians’ Information and Education Resource) and MKSAP (Medical Knowledge and Self-Assessment Program). Annals of Internal Medicine Science Writer: editors develop In the Clinic from these primary sources in collaboration with Jennifer F. Wilson the ACP’s Medical Education and Publishing Division and with the assistance of science writers and physician writers. Editorial consultants from PIER and MKSAP provide expert review of the content. Readers who are interested in these primary resources for more detail can consult http://pier.acponline.org and other resources referenced in each issue of In the Clinic. CME Objective: To gain knowledge about the management of patients with vagini- tis and cervicitis. The information contained herein should never be used as a substitute for clinical judgment. © 2009 American College of Physicians in the clinic he vagina has a squamous epithelium and is susceptible to bacterial vaginosis, trichomoniasis, and candidiasis. Vaginitis may also result Tfrom irritants, allergic reactions, or postmenopausal atrophy. The endocervix has a columnar epithelium and is susceptible to infection with Neisseria gonorrhoeae, Chlamydia trachomatis, or less commonly, herpes sim- plex virus. Vaginitis causes discomfort, but rarely has serious consequences except during pregnancy and gynecologic surgery. Cervicitis may be asymptomatic and if untreated, can lead to pelvic inflammatory disease (PID), which can damage the reproductive organs and lead to infertility, ectopic pregnancy, or chronic pelvic pain. -

Intricate Connections Between the Microbiota and Endometriosis
International Journal of Molecular Sciences Review Intricate Connections between the Microbiota and Endometriosis Irene Jiang, Paul J. Yong, Catherine Allaire and Mohamed A. Bedaiwy * Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, University of British Columbia, D415A-4500 Oak Street, Vancouver, BC V6H 3N1, Canada; [email protected] (I.J.); [email protected] (P.J.Y.); [email protected] (C.A.) * Correspondence: [email protected]; Tel.: +604-875-2000 (ext. 4310) Abstract: Imbalances in gut and reproductive tract microbiota composition, known as dysbiosis, disrupt normal immune function, leading to the elevation of proinflammatory cytokines, compro- mised immunosurveillance and altered immune cell profiles, all of which may contribute to the pathogenesis of endometriosis. Over time, this immune dysregulation can progress into a chronic state of inflammation, creating an environment conducive to increased adhesion and angiogenesis, which may drive the vicious cycle of endometriosis onset and progression. Recent studies have demonstrated both the ability of endometriosis to induce microbiota changes, and the ability of antibiotics to treat endometriosis. Endometriotic microbiotas have been consistently associated with diminished Lactobacillus dominance, as well as the elevated abundance of bacterial vaginosis-related bacteria and other opportunistic pathogens. Possible explanations for the implications of dysbiosis in endometriosis include the Bacterial Contamination Theory and immune activation, cytokine- impaired gut function, altered estrogen metabolism and signaling, and aberrant progenitor and stem-cell homeostasis. Although preliminary, antibiotic and probiotic treatments have demonstrated efficacy in treating endometriosis, and female reproductive tract (FRT) microbiota sampling has Citation: Jiang, I.; Yong, P.J.; Allaire, successfully predicted disease risk and stage. -

Año XVII. Núm. 17. Madrid 1º De Mayo De 1873
YL AMERICANA I# ¡ i i fìssisi '¡YLV: ensñlA , í^fW< iw^in IMiKGlUS DE 5¿ L'SGHlClnN. AÑO XVII.— NÛM. XVII. l'llK C lO * DF. SL'SCRTCION. aS". 5KMKf*TH£. TWMKMíllE. M.MF.STRK. Dinr.r.i"n-PR('1'IKT.M:I,|. D. ABELARDO DE CARLOS 12 7 3 5 pesetas. 18 pesetas. l(i pesetas. (.’uba y Pucrtn-Ilico.. pesos fnortes. pesos fuertes. Madrid............... AD.MIM'JIl.UiuX, CARRETAS, 12, I'KINCII'AL. Provincia?........... 4 0 id. 20 id. 11 id Filipinas...................... 15 iil. 8 id. 4 .3 0 0 2 .3 0 0 veis. Portugal.. 8 .4 0 0 veis. reís. Madrid, I." dr Mavì» de 1 8 7 3 . Eu lus demas Americas lijan el precio los Fres. Agentes. SUMARIO. iiiiiiginc-c lo ij»io .-era el nuestro, i|Uc la tiene tan rica y variada; tan Im o .—Tlr vbta ironrnil , pur i l Murrini* rte V 1 cumula di toda clase de aconteci Ue.Alcrrp. — Xuestro» pruhuilos, por I». Ku-> Ilio Martine?, «le Vrliwe — Ìtobenn Robert, miento:?. por D. Eu-ajbio Rla?e(>.—Vitijr nlrfilcd"-r tir- hi Desde laanicrior Revista, ¡ cuán Exposlclon imi vorrai ili Vionn. por un Cnbntlc-: to-, etniu graves y trascendentales ro Espiulòl.—lìitHiriifiii dii Uni un «le l.t-bii,'. p u D. II. T. Malie/, il»* Lumi'.—ìli ” ini ¡ui- lian oí niTuie en él ! ¡ Cómo lia cam tiguo mitigo 1.1. .lumi Multino/. Villcvgtvs.pov inado la faz «le las cosas! ¡Cómo se D. Munuol Juan Diluiti.— HI -nrnoilc un cuento (coiiclliilon). por Carlini Rublo.—Kii Iti han complicado y envenenado todas orlili»del mar, poe-ai, pi.r le Ju.