C:\SCANSOUTH\ATSDR\Wpd\Methyl Parathion.Wpd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ACEPHATE (Addendum)
3 ACEPHATE (addendum) First draft prepared by Professor P.K. Gupta 1 and Dr Angelo Moretto 2 1 Rajinder Nagar, Bareilly, UP, India; 2 Dipartimento Medicina Ambientale e Sanità Pubblica, Università di Padova, Padova, Italy Explanation..........................................................................................................3 Evaluation for acceptable daily intake.................................................................4 Biochemical aspects ......................................................................................4 Oral absorption, distribution, excretion and metabolism .......................4 Toxicological studies.....................................................................................5 Acute toxicity.........................................................................................5 Short-term studies of toxicity.................................................................6 Special studies........................................................................................7 Studies on inhibition of cholinesterase activity in vitro ..................7 Short-term study of neurotoxicity ...................................................7 Developmental neurotoxicity..........................................................9 Observations in humans ..............................................................................10 Comments..........................................................................................................12 Toxicological evaluation ...................................................................................13 -
Additive Interactions of Some Reduced-Risk Biocides and Two
www.nature.com/scientificreports OPEN Additive interactions of some reduced‑risk biocides and two entomopathogenic nematodes suggest implications for integrated control of Spodoptera litura (Lepidoptera: Noctuidae) Rashad Rasool Khan 1,2*, Muhammad Arshad 1*, Asad Aslam 3 & Muhammad Arshad 4 Higher volumes of conventional and novel chemical insecticides are applied by farmers to control resistant strains of armyworm (Spodoperta litura) in Pakistan without knowing their risks to the environment and to public health. Ten reduced‑risk insecticides were tested for their compatibility with two entomopathogenic nematodes (EPNs); Heterorhabditis indica and Steinernema carpocapsae rd against S. litura. The insecticide emamectin benzoate was highly toxic (LC50 = 2.97 mg/l) against 3 instar S. litura larvae when applied alone whereas, novaluron and methoxyfenozide were the least toxic (LC50 = 29.56 mg/l and 21.06 mg/l), respectively. All the insecticides proved harmless against the two EPNs even 96 h after treatment. Indoxacarb, fubendiamide and spinetoram produced the greatest mortalities (72–76%) of S. litura larvae after 72 h when applied in mixtures with H. indica. Lowest mortalities (44.00 ± 3.74% and 48.00 ± 2.89) were observed for mixtures of H. indica with methoxyfenozide and chlorfenapyr, respectively. The positive control treatments with both EPNs (S. carpocapsae and H. indica) produced > 50% mortality 96 h after treatment. For insecticide mixtures with S. carpocapsae, only indoxacarb produced 90% mortality of larvae, whereas, indoxacarb, fubendiamide, emamectin benzoate, and spinetoram produced 90–92% mortality of larvae when applied in mixtures with H. indica. Additive interactions (Chi‑square < 3.84) of EPN mixtures with reduced volumes of reduced‑risk insecticides suggest opportunities to develop more environmentally favorable pest management programs for S. -
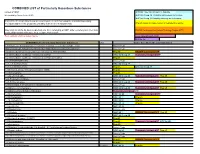
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -

Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries
Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries. Peter Jentsch Extension Associate Department of Entomology Cornell University's Hudson Valley Lab 3357 Rt. 9W; PO box 727 Highland, NY 12528 email: [email protected] Phone 845-691-7151 Mobile: 845-417-7465 http://www.nysaes.cornell.edu/ent/faculty/jentsch/ 2 Historical Perspectives on Fruit Production: Fruit Tree Pest Management, Regulation and New Chemistries. by Peter Jentsch I. Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 Synthetic Pesticide Development and Use II. Influences Changing the Pest Management Profile in Apple Production Chemical Residues in Early Insect Management Historical Chemical Regulation Recent Regulation Developments Changing Pest Management Food Quality Protection Act of 1996 The Science Behind The Methodology Pesticide Revisions – Requirements For New Registrations III. Resistance of Insect Pests to Insecticides Resistance Pest Management Strategies IV. Reduced Risk Chemistries: New Modes of Action and the Insecticide Treadmill Fermentation Microbial Products Bt’s, Abamectins, Spinosads Juvenile Hormone Analogs Formamidines, Juvenile Hormone Analogs And Mimics Insect Growth Regulators Azadirachtin, Thiadiazine Neonicotinyls Major Reduced Risk Materials: Carboxamides, Carboxylic Acid Esters, Granulosis Viruses, Diphenyloxazolines, Insecticidal Soaps, Benzoyl Urea Growth Regulators, Tetronic Acids, Oxadiazenes , Particle Films, Phenoxypyrazoles, Pyridazinones, Spinosads, Tetrazines , Organotins, Quinolines. 3 I Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 The apple has a rather ominous origin. Its inception is framed in the biblical text regarding the genesis of mankind. The backdrop appears to be the turbulent setting of what many scholars believe to be present day Iraq. -

Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues
Mississippi State University Scholars Junction Theses and Dissertations Theses and Dissertations 8-10-2018 Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues Edward Caldwell Meek Follow this and additional works at: https://scholarsjunction.msstate.edu/td Recommended Citation Meek, Edward Caldwell, "Determination of Age-Related Differences in Activation and Detoxication of Organophosphates in Rat and Human Tissues" (2018). Theses and Dissertations. 1339. https://scholarsjunction.msstate.edu/td/1339 This Dissertation - Open Access is brought to you for free and open access by the Theses and Dissertations at Scholars Junction. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Scholars Junction. For more information, please contact [email protected]. Template A v3.0 (beta): Created by J. Nail 06/2015 Determination of age-related differences in activation and detoxication of organophosphates in rat and human tissues By TITLE PAGE Edward Caldwell Meek A Dissertation Submitted to the Faculty of Mississippi State University in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Environmental Toxicology in the College of Veterinary Medicine Mississippi State, Mississippi August 2018 Copyright by COPYRIGHT PAGE Edward Caldwell Meek 2018 Determination of age-related differences in activation and detoxication of organophosphates in rat and human tissues By APPROVAL PAGE Edward Caldwell Meek -

The Spruce Budworm, Choristoneura Fumiferana
02-01370 Spruce Budworm Bro 10/10/02 11:09 AM Page 1 MORE INFORMATION The he spruce budworm, Choristoneura fumiferana For more information on Spruce Budworms call: The Tree Line Spruce (Clemens), is the most destructive and widely (204) 945-7866. Or write: Budworm distributed forest defoliator in North America. Manitoba Conservation Forestry Branch In Manitoba T Forest Health and Ecology The destructive phase of this pest is the larval or caterpillar 200 Saulteaux Crescent Winnipeg, Manitoba R3J 3W3 stage. Massive budworm outbreaks occur periodically, Web site: www.gov.mb.ca/natres/forestry/ destroying hundreds of thousands of hectares of valuable fir and spruce. Aerial view of budworm damage In eastern Canada the budworm’s preferred food is balsam fir, Photos courtesy of Canadian Forest Service, Great Lakes Forest Research Centre, white spruce and red spruce. In Manitoba, the budworm Sault Ste. Marie, Ontario and Northern Forest Research Centre, Edmonton, Alberta. feeds primarily on white spruce and balsam fir, and, less frequently, on black spruce. 02-01370 Spruce Budworm Bro 10/10/02 11:09 AM Page 2 DESCRIPTION OF LIFE STAGES LIFE CYCLE DAMAGE CONTROL The adult moth has a wingspread of The female moth lays In light and moderate infestations Various insecticides are used 21 to 30 mm. It is grey-brown in its eggs in July on the damage is restricted to a partial against the spruce budworm to colour with silvery white patches on underside of needles. loss of new foliage, particularly in protect valuable spruce and fir the forewings. Normally, the eggs the upper crown trees. -

INDEX to PESTICIDE TYPES and FAMILIES and PART 180 TOLERANCE INFORMATION of PESTICIDE CHEMICALS in FOOD and FEED COMMODITIES
US Environmental Protection Agency Office of Pesticide Programs INDEX to PESTICIDE TYPES and FAMILIES and PART 180 TOLERANCE INFORMATION of PESTICIDE CHEMICALS in FOOD and FEED COMMODITIES Note: Pesticide tolerance information is updated in the Code of Federal Regulations on a weekly basis. EPA plans to update these indexes biannually. These indexes are current as of the date indicated in the pdf file. For the latest information on pesticide tolerances, please check the electronic Code of Federal Regulations (eCFR) at http://www.access.gpo.gov/nara/cfr/waisidx_07/40cfrv23_07.html 1 40 CFR Type Family Common name CAS Number PC code 180.163 Acaricide bridged diphenyl Dicofol (1,1-Bis(chlorophenyl)-2,2,2-trichloroethanol) 115-32-2 10501 180.198 Acaricide phosphonate Trichlorfon 52-68-6 57901 180.259 Acaricide sulfite ester Propargite 2312-35-8 97601 180.446 Acaricide tetrazine Clofentezine 74115-24-5 125501 180.448 Acaricide thiazolidine Hexythiazox 78587-05-0 128849 180.517 Acaricide phenylpyrazole Fipronil 120068-37-3 129121 180.566 Acaricide pyrazole Fenpyroximate 134098-61-6 129131 180.572 Acaricide carbazate Bifenazate 149877-41-8 586 180.593 Acaricide unclassified Etoxazole 153233-91-1 107091 180.599 Acaricide unclassified Acequinocyl 57960-19-7 6329 180.341 Acaricide, fungicide dinitrophenol Dinocap (2, 4-Dinitro-6-octylphenyl crotonate and 2,6-dinitro-4- 39300-45-3 36001 octylphenyl crotonate} 180.111 Acaricide, insecticide organophosphorus Malathion 121-75-5 57701 180.182 Acaricide, insecticide cyclodiene Endosulfan 115-29-7 79401 -

Method 8141B
METHOD 8141B ORGANOPHOSPHORUS COMPOUNDS BY GAS CHROMATOGRAPHY 1.0 SCOPE AND APPLICATION 1.1 This method provides procedures for the gas chromatographic (GC) determination of organophosphorus (OP) compounds. The compounds listed in the table below can be determined by GC using capillary columns with a flame photometric detector (FPD) or a nitrogen-phosphorus detector (NPD). Triazine herbicides can also be determined with this method when the NPD is used. Although performance data are presented for each of the listed chemicals, it is unlikely that all of them could be determined in a single analysis. This limitation results because the chemical and chromatographic behavior of many of these chemicals can result in co-elution. The analyst must select columns, detectors, and calibration procedures for the specific analytes of interest. Any listed chemical is a potential method interference when it is not a target analyte. Analyte CAS Registry No. Organophosphorus Pesticides Asponb 3244-90-4 Azinphos-methyl 86-50-0 Azinphos-ethyla 2642-71-9 Bolstar (Sulprofos) 35400-43-2 Carbophenothiona 786-19-6 Chlorfenvinphosa 470-90-6 Chlorpyrifos 2921-88-2 Chlorpyrifos methyla 5598-13-0 Coumaphos 56-72-4 Crotoxyphosa 7700-17-6 Demeton-Oc 8065-48-3 Demeton-Sc 8065-48-3 Diazinon 333-41-5 Dichlorofenthiona 97-17-6 Dichlorvos (DDVP) 62-73-7 Dicrotophosa 141-66-2 Dimethoate 60-51-5 Dioxathiona,c 78-34-2 Disulfoton 298-04-4 EPN 2104-64-5 Ethiona 563-12-2 Ethoprop 13194-48-4 Famphura 52-85-7 8141B - 1 Revision 2 November 2000 Analyte CAS Registry No. Fenitrothiona -

Index to the NLM Classification 2011
National Library of Medicine Classification 2011 Index Disease see Tyrosinemias 1-8 5,12-diHETE see Leukotriene B4 1,2-Benzopyrones see Coumarins 5,12-HETE see Leukotriene B4 1,2-Dibromoethane see Ethylene Dibromide 5-HT see Serotonin 1,8-Dihydroxy-9-anthrone see Anthralin 5-HT Antagonists see Serotonin Antagonists 1-Oxacephalosporin see Moxalactam 5-Hydroxytryptamine see Serotonin 1-Propanol 5-Hydroxytryptamine Antagonists see Serotonin Organic chemistry QD 305.A4 Antagonists Pharmacology QV 82 6-Mercaptopurine QV 269 1-Sar-8-Ala Angiotensin II see Saralasin 7S RNA see RNA, Small Nuclear 1-Sarcosine-8-Alanine Angiotensin II see Saralasin 8-Hydroxyquinoline see Oxyquinoline 13-cis-Retinoic Acid see Isotretinoin 8-Methoxypsoralen see Methoxsalen 15th Century History see History, 15th Century 8-Quinolinol see Oxyquinoline 16th Century History see History, 16th Century 17 beta-Estradiol see Estradiol 17-Ketosteroids WK 755 A 17-Oxosteroids see 17-Ketosteroids A Fibers see Nerve Fibers, Myelinated 17th Century History see History, 17th Century Aardvarks see Xenarthra 18th Century History see History, 18th Century Abate see Temefos 19th Century History see History, 19th Century Abattoirs WA 707 2',3'-Cyclic-Nucleotide Phosphodiesterases QU 136 Abbreviations 2,4-D see 2,4-Dichlorophenoxyacetic Acid Chemistry QD 7 2,4-Dichlorophenoxyacetic Acid General P 365-365.5 Organic chemistry QD 341.A2 Library symbols (U.S.) Z 881 2',5'-Oligoadenylate Polymerase see Medical W 13 2',5'-Oligoadenylate Synthetase By specialties (Form number 13 in any NLM -

20110628140658587.Pdf
1210 YUE ET AL.:JOURNAL OF AOAC INTERNATIONAL VOL. 91, NO. 5, 2008 SPECIAL GUEST EDITOR SECTION High-Performance Thin-Layer Chromatographic Analysis of Selected Organophosphorous Pesticide Residues in Tea YONGDE YUE International Center for Bamboo and Rattan, 100102, Beijing, People’s Republic of China RONG ZHANG and WEI FAN Key Laboratory for Agri-Food Safety of Anhui Province, School of Resources and Environment, Anhui Agricultural University, Hefei, Anhui, 230036, People’s Republic of China FENG TANG International Center for Bamboo and Rattan, 100102, Beijing, People’s Republic of China The separation of 9 organophosphates determination procedure. In many cases, searching for a fast (monocrotophos, quinalphos, triazophos, and efficient method for enrichment and determination of parathion-methyl, isofenphos-methyl, temephos, organophosphorous residues from complex matrixes is still a parathion, phoxim-ethyl, and chlorpyrifos) by challenge for many researchers. high-performance thin-layer chromatography In many analytical situations, modern quantitative (HPTLC) with automated multiple development was high-performance thin-layer chromatography (HPTLC), studied. The HPTLC method was developed and when properly performed by well-trained analysts, has many validated for analysis of residues of phoxim-ethyl advantages over HPLC or GC. These advantages include and chlorpyrifos in tea. The sample was extracted simplicity of operation, the availability of many sensitive and with acetonitrile and cleaned up by ENVI-CARB selective reagents for detection and confirmation without solid-phase extraction. The extract was directly interference from the mobile phase, the ability to repeat applied as bands to glass-backed silica gel 60F254 detection and quantification at any time with changed HPTLC plates. -

Imidacloprid Does Not Enhance Growth and Yield of Muskmelon In
HORTSCIENCE 30(5):997–999. 1995. plant growth and yield responses of muskmel- ons to imidacloprid in the presence and ab- Imidacloprid Does Not Enhance sence of whiteflies. Growth and Yield of Muskmelon in the Materials and Methods Greenhouse studies. All plants used in the Absence of Whitefly greenhouse tests were direct-seeded ‘Topmark’ muskmelons in a 3 soil : 3 perlite : 1 peat J.C. Palumbo and C.A. Sanchez mixture in 1.5-liter pots. Each pot contained 500 g of soil mixture and was planted with four University of Arizona, Yuma Valley Agricultural Center, 6425 West 8th Street, to five seeds. Seedlings were grown during Yuma, AZ 85364 Mar. and Apr. 1994 in a glasshouse under natural light with adequate water and nutrients Additional index words. Bemisia tabaci, Bemisia argentifolii, Cucumis melo, relative growth for maximum growth. Upon emergence, seed- rate, net assimilation rate ling plants were thinned to one per pot. Pots Abstract. Imidacloprid is a new, chloronicotinyl insecticide currently being used to control were then placed in wooden-frame exclusion × × sweetpotato whitefly [Bemisia tabaci Genn, also known as silverleaf whitefly (Bemisia cages (1.7 m width 1.2 m long 0.6 m high) argentifolii Bellows and Perring)]. Large growth and yield increases of muskmelon screened with fine organdy cloth to exclude (Cucumis melo L.) following the use of imidacloprid have caused some to speculate that this whitefly adults and other insects. The cages ± compound may enhance growth and yield above that expected from insect control alone. were maintained in the glasshouse at 28 4C. Greenhouse and field studies were conducted to evaluate the growth and yield response of Whitefly adults used in these studies were melons to imidacloprid in the presence and absence of whitefly pressure. -

Review of Azinphos-Methyl Was Undertaken by the Office of Chemical Safety (OCS), Which Considered All the Toxicological Data and Information Submitted for the Review
The reconsideration of the active constituent azinphos-methyl, registrations of products containing azinphos-methyl and approvals of their associated labels PRELIMINARY REVIEW FINDINGS Volume 1: Review Summary OCTOBER 2006 Canberra Australia Azinphos-methyl review – Preliminary Review Findings © Australian Pesticides & Veterinary Medicines Authority 2006 This work is copyright. Apart from any use permitted under the Copyright Act 1968, no part may be reproduced without permission from the Australian Pesticides & Veterinary Medicines Authority. The Australian Pesticides & Veterinary Medicines Authority publishes this preliminary review findings report for the active constituent azinphos-methyl and products containing azinphos- methyl. For further information about this review or the Pesticides Review Program, contact: Manager Chemical Review Australian Pesticides & Veterinary Medicines Authority PO Box E 240 KINGSTON ACT 2604 Australia Telephone: 61 2 6272 3213 Facsimile: 61 2 6272 3218 Email: [email protected] APVMA web site: http://www.apvma.gov.au i Azinphos-methyl review – Preliminary Review Findings FOREWORD The Australian Pesticides & Veterinary Medicines Authority (APVMA) is an independent statutory authority with responsibility for the regulation of agricultural and veterinary chemicals in Australia. Its statutory powers are provided in the Agvet Codes scheduled to the Agricultural and Veterinary Chemicals Code Act 1994. The APVMA can reconsider the approval of an active constituent, the registration of a chemical product or