Peripheral T-Cell Lymphoma Facts No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Lymphoma and Multiple Myeloma Center
The Lymphoma and Multiple Myeloma Center What Sets Us Apart We provide multidisciplinary • Experienced, nationally and internationally recognized physicians dedicated exclusively to treating patients with lymphoid treatment for optimal survival or plasma cell malignancies and quality of life for patients • Cellular therapies such as Chimeric Antigen T-Cell (CAR T) therapy for relapsed/refractory disease with all types and stages of • Specialized diagnostic laboratories—flow cytometry, cytogenetics, and molecular diagnostic facilities—focusing on the latest testing lymphoma, chronic lymphocytic that identifies patients with high-risk lymphoid malignancies or plasma cell dyscrasias, which require more aggresive treatment leukemia, multiple myeloma and • Novel targeted therapies or intensified regimens based on the other plasma cell disorders. cancer’s genetic and molecular profile • Transplant & Cellular Therapy program ranked among the top 10% nationally in patient outcomes for allogeneic transplant • Clinical trials that offer tomorrow’s treatments today www.roswellpark.org/partners-in-practice Partners In Practice medical information for physicians by physicians We want to give every patient their very best chance for cure, and that means choosing Roswell Park Pathology—Taking the best and Diagnosis to a New Level “ optimal front-line Lymphoma and myeloma are a diverse and heterogeneous group of treatment.” malignancies. Lymphoid malignancy classification currently includes nearly 60 different variants, each with distinct pathophysiology, clinical behavior, response to treatment and prognosis. Our diagnostic approach in hematopathology includes the comprehensive examination of lymph node, bone marrow, blood and other extranodal and extramedullary tissue samples, and integrates clinical and diagnostic information, using a complex array of diagnostics from the following support laboratories: • Bone marrow laboratory — Francisco J. -

Low-Grade Non-Hodgkin Lymphoma Book
Low-grade non-Hodgkin lymphoma Low-grade non-Hodgkin lymphoma Follicular lymphoma Mantle cell lymphoma Marginal zone lymphomas Lymphoplasmacytic lymphoma Waldenström’s macroglobulinaemia This book has been researched and written for you by Lymphoma Action, the only UK charity dedicated to people affected by lymphoma. We could not continue to support you, your clinical team and the wider lymphoma community, without the generous donations of our incredible supporters. As an organisation we do not receive any government or NHS funding and so every penny received is truly valued. To make a donation towards our work, please visit lymphoma-action.org.uk/Donate 2 Your lymphoma type and stage Your treatment Key contact Name: Role: Contact details: Job title/role Name and contact details GP Consultant haematologist/ oncologist Clinical nurse specialist or key worker Treatment centre 3 About this book Low-grade (or indolent) non-Hodgkin lymphoma is a type of blood cancer that develops from white blood cells called lymphocytes. It is a broad term that includes lots of different types of lymphoma. This book explains what low-grade non-Hodgkin lymphoma is and how it is diagnosed and treated. It includes tips on coping with treatment and dealing with day-to-day life. The book is split into chapters. You can dip in and out of it and read the sections that are relevant to you at any given time. Important and summary points are written in the chapter colour. Lists practical tips and chapter summaries. Gives space for questions and notes. Lists other resources you might find useful, some of which are online. -

Vorinostat—An Overview Aditya Kumar Bubna
E-IJD RESIDENTS' PAGE Vorinostat—An Overview Aditya Kumar Bubna Abstract From the Consultant Vorinostat is a new drug used in the management of cutaneous T cell lymphoma when the Dermatologist, Kedar Hospital, disease persists, gets worse or comes back during or after treatment with other medicines. It is Chennai, Tamil Nadu, India an efficacious and well tolerated drug and has been considered a novel drug in the treatment of this condition. Currently apart from cutaneous T cell lymphoma the role of Vorinostat for Address for correspondence: other types of cancers is being investigated both as mono-therapy and combination therapy. Dr. Aditya Kumar Bubna, Kedar Hospital, Mugalivakkam Key Words: Cutaneous T cell lymphoma, histone deacytelase inhibitor, Vorinostat Main Road, Porur, Chennai - 600 125, Tamil Nadu, India. E-mail: [email protected] What was known? • Vorinostat is a histone deacetylase inhibitor. • It is an FDA approved drug for the treatment of cutaneous T cell lymphoma. Introduction of Vorinostat is approximately 9. Vorinostat is slightly Vorinostat is a histone deacetylase (HDAC) inhibitor, soluble in water, alcohol, isopropanol and acetone and is structurally belonging to the hydroxymate group. Other completely soluble in dimethyl sulfoxide. drugs in this group include Givinostat, Abexinostat, Mechanism of action Panobinostat, Belinostat and Trichostatin A. These Vorinostat is a broad inhibitor of HDAC activity and inhibits are an emergency class of drugs with potential anti- class I and class II HDAC enzymes.[2,3] However, Vorinostat neoplastic activity. These drugs were developed with the does not inhibit HDACs belonging to class III. Based on realization that apart from genetic mutation, alteration crystallographic studies, it has been seen that Vorinostat of HDAC enzymes affected the phenotypic and genotypic binds to the zinc atom of the catalytic site of the HDAC expression in cells, which in turn lead to disturbed enzyme with the phenyl ring of Vorinostat projecting out of homeostasis and neoplastic growth. -

Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy
cancers Review Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy Miriam Marangon 1, Carlo Visco 2 , Anna Maria Barbui 3, Annalisa Chiappella 4, Alberto Fabbri 5, Simone Ferrero 6,7 , Sara Galimberti 8 , Stefano Luminari 9,10 , Gerardo Musuraca 11, Alessandro Re 12 , Vittorio Ruggero Zilioli 13 and Marco Ladetto 14,15,* 1 Department of Hematology, Azienda Sanitaria Universitaria Giuliano Isontina, 34129 Trieste, Italy; [email protected] 2 Section of Hematology, Department of Medicine, University of Verona, 37134 Verona, Italy; [email protected] 3 Hematology Unit, ASST Papa Giovanni XXIII, 24127 Bergamo, Italy; [email protected] 4 Division of Hematology, Fondazione IRCCS, Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] 5 Hematology Division, Department of Oncology, Azienda Ospedaliero-Universitaria Senese, 53100 Siena, Italy; [email protected] 6 Hematology Division, Department of Molecular Biotechnologies and Health Sciences, Università di Torino, 10126 Torino, Italy; [email protected] 7 Hematology 1, AOU Città della Salute e della Scienza di Torino, 10126 Torino, Italy 8 Hematology Unit, Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy; [email protected] 9 Hematology Unit, Azienda Unità Sanitaria Locale IRCCS di Reggio Emilia, 42123 Modena, Italy; [email protected] 10 Surgical, Medical and Dental Department of Morphological Sciences Related -
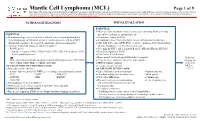
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

Divergent Clonal Evolution of a Common Precursor to Mantle Cell Lymphoma and Classic Hodgkin Lymphoma
Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Divergent clonal evolution of a common precursor to mantle cell lymphoma and classic Hodgkin lymphoma Hammad Tashkandi1, Kseniya Petrova-Drus1, Connie Lee Batlevi2, Maria Arcila1, Mikhail Roshal1, Filiz Sen1, Jinjuan Yao1, Jeeyeon Baik1, Ashley Bilger2, Jessica Singh2, Stephanie de Frank2, Anita Kumar2, Ruth Aryeequaye1, Yanming Zhang1, Ahmet Dogan1, Wenbin Xiao1,* 1Department of Pathology, 2Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY *Correspondence: Wenbin Xiao, MD, PhD Department of Pathology Memorial Sloan Kettering Cancer Center 1275 York Avenue New York, NY 10065 [email protected] Running title: Clonally related mantle cell lymphoma and classic Hodgkin lymphoma Words: 1771 Figures: 2 Tables: 1 Reference: 14 Supplemental materials: Figure S1-S2, Table S1-S4 Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract: Clonal heterogeneity and evolution of mantle cell lymphoma (MCL) remain unclear despite the progress in our understanding of its biology. Here we report a 71 years old male patient with an aggressive MCL and depict the clonal evolution from initial diagnosis of typical MCL to relapsed blastoid MCL. During the course of disease, the patient was diagnosed with Classic Hodgkin lymphoma (CHL), and received CHL therapeutic regimen. Molecular analysis by next generation sequencing of both MCL and CHL demonstrated clonally related CHL with characteristic immunophenotype and PDL1/2 gains. Moreover, our data illustrate the clonal heterogeneity and acquisition of additional genetic aberrations including a rare fusion of SEC22B-NOTCH2 in the process of clonal evolution. -

Peripheral T-Cell Lymphomas
Critical Reviews in Oncology/Hematology 99 (2016) 214–227 CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Contents lists available at ScienceDirect Critical Reviews in Oncology/Hematology jo urnal homepage: www.elsevier.com/locate/critrevonc Panoptic clinical review of the current and future treatment of relapsed/refractory T-cell lymphomas: Peripheral T-cell lymphomas a,∗ b c c d Pier Luigi Zinzani , Vijayveer Bonthapally , Dirk Huebner , Richard Lutes , Andy Chi , e,f Stefano Pileri a Institute of Hematology ‘L. e A. Seràgnoli’, Policlinico Sant’Orsola-Malpighi, University of Bologna, Via Massarenti 9, 40138 Bologna, Italy b 1 Global Outcomes and Epidemiology Research (GOER), Millennium Pharmaceuticals Inc., 40 Lansdowne Street, Cambridge, MA 02139, USA c 1 Oncology Clinical Research, Millennium Pharmaceuticals Inc., 35 Lansdowne Street, Cambridge, MA 02139, USA d 1 Department of Biostatistics, Millennium Pharmaceuticals Inc., 40 Lansdowne Street, Cambridge, MA 02139, USA e Department of Experimental, Diagnostic, and Specialty Medicine, Bologna University School of Medicine, Via Massarenti 8, 40138 Bologna, Italy f Unit of Hematopathology, European Institute of Oncology, Via Ripamonti 435, 20141 Milan, Italy Contents 1. Introduction . 214 2. Methodology. .215 3. Treatment of relapsed/refractory PTCL . 215 3.1. Conventional chemotherapy in relapsed/refractory PTCL. .215 3.2. Approved therapies in relapsed/refractory PTCL . 216 3.3. Investigational and off-label therapies in relapsed/refractory PTCL . 222 4. Concluding remarks . 224 Conflict of interest . 224 Funding . 224 Acknowledgments. .224 References . 224 Biography . 227 a r t i c l e i n f o a b s t r a c t Article history: Peripheral T-cell lymphomas (PTCLs) tend to be aggressive and chemorefractory, with about 70% of Received 29 June 2015 patients developing relapsed/refractory disease. -

Belinostat (Beleodaq®)
Belinostat (Beleodaq®) Belinostat (Beleodaq®) Pronounced: be-lin-oh-stat Classification: Histone Deacetylase Inhibitor About Belinostat (Beleodaq®) Belinostat is in a class of anti-cancer therapies called histone deacetylase (HDAC) inhibitors. Histone deacetylation is a biochemical process that is thought to play a role in promoting tumor growth. It does this by silencing some tumor suppressor genes, as well as other genes that are responsible for cell cycle progression, cell proliferation, programmed cell death (apoptosis), and differentiation (transformation of young cells into specialized cells). Therefore, blocking histone deacetylation may allow the body to block tumor growth and prevent progression. How to Take Belinostat Belinostat is given by intravenous (IV, into a vein) infusion. The dose and how often you receive this medication is based on your weight and will be decided by your provider. Your dose may be reduced if you are having severe side effects. Possible Side Effects of Belinostat There are a number of things you can do to manage the side effects of belinostat. Talk to your care team about these recommendations. They can help you decide what will work best for you. These are some of the most common or important side effects: Nausea and/or Vomiting Talk to your oncology care team so they can prescribe medications to help you manage nausea and vomiting. In addition, dietary changes may help. Avoid things that may worsen the symptoms, such as heavy or greasy/fatty, spicy or acidic foods (lemons, tomatoes, oranges). Try saltines, or ginger ale to lessen symptoms. Call your oncology care team if you are unable to keep fluids down for more than 12 hours or if you feel lightheaded or dizzy at any time. -

Histone Deacetylase Inhibitors
ANTICANCER RESEARCH 36 : 5019-5024 (2016) doi:10.21873/anticanres.11070 Review Histone Deacetylase Inhibitors: A Novel Therapeutic Weapon Αgainst Medullary Thyroid Cancer? CHRISTOS DAMASKOS 1,2* , SERENA VALSAMI 3* , ELEFTHERIOS SPARTALIS 2, EFSTATHIOS A. ANTONIOU 1, PERIKLIS TOMOS 4, STEFANOS KARAMAROUDIS 5, THEOFANO ZOUMPOU 5, VASILIOS PERGIALIOTIS 2, KONSTANTINOS STERGIOS 2,6 , CONSTANTINOS MICHAELIDES 7, KONSTANTINOS KONTZOGLOU 1, DESPINA PERREA 2, NIKOLAOS NIKITEAS 2 and DIMITRIOS DIMITROULIS 1 1Second Department of Propedeutic Surgery, “Laiko” General Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 2Laboratory of Experimental Surgery and Surgical Research N.S. Christeas, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 3Blood Transfusion Department, Aretaieion Hospital, Medical School, National and Kapodistrian Athens University, Athens, Greece; 4Department of Thoracic Surgery, “Attikon” General Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 5Medical School, National and Kapodistrian University of Athens, Athens, Greece; 6Colorectal Department, General Surgery, The Princess Alexandra Hospital NHS Trust, Harlow, U.K.; 71st Department of Pathology, School of Medicine, University of Athens, Athens, Greece Abstract. Background/ Aim : Medullary thyroid cancer (MTC) is and histone deacetylase (HDAC) seems to play a potential role highly malignant, metastatic and recurrent, remaining generally to gene transcription. On the -

Relapsed Mantle Cell Lymphoma: Current Management, Recent Progress, and Future Directions
Journal of Clinical Medicine Review Relapsed Mantle Cell Lymphoma: Current Management, Recent Progress, and Future Directions David A Bond 1,*, Peter Martin 2 and Kami J Maddocks 1 1 Division of Hematology, The Ohio State University, Columbus, OH 43210, USA; [email protected] 2 Division of Hematology and Oncology, Weill Cornell Medical College, New York, NY 11021, USA; [email protected] * Correspondence: [email protected] Abstract: The increasing number of approved therapies for relapsed mantle cell lymphoma (MCL) provides patients effective treatment options, with increasing complexity in prioritization and se- quencing of these therapies. Chemo-immunotherapy remains widely used as frontline MCL treatment with multiple targeted therapies available for relapsed disease. The Bruton’s tyrosine kinase in- hibitors (BTKi) ibrutinib, acalabrutinib, and zanubrutinib achieve objective responses in the majority of patients as single agent therapy for relapsed MCL, but differ with regard to toxicity profile and dosing schedule. Lenalidomide and bortezomib are likewise approved for relapsed MCL and are active as monotherapy or in combination with other agents. Venetoclax has been used off-label for the treatment of relapsed and refractory MCL, however data are lacking regarding the efficacy of this approach particularly following BTKi treatment. Anti-CD19 chimeric antigen receptor T-cell (CAR-T) therapies have emerged as highly effective therapy for relapsed MCL, with the CAR-T treatment brexucabtagene autoleucel now approved for relapsed MCL. In this review the authors summarize evidence to date for currently approved MCL treatments for relapsed disease including Citation: Bond, D.A; Martin, P.; sequencing of therapies, and discuss future directions including combination treatment strategies Maddocks, K.J Relapsed Mantle Cell and new therapies under investigation. -

151109EN ASH Abstract
Onxeo Reports Initial Results of Phase 1 Trial Evaluating Belinostat in Combination with CHOP in Peripheral T-cell Lymphoma (PTCL) Full results to be reported in Oral Presentation at 2015 ASH (American Society of Hematology) Annual Meeting Data demonstrate 89% objective response rate, 72% complete response rate, and good safety profile of belinostat in combination with CHOP Study supports the interest of belinostat in combination with CHOP as first-line treatment for PTCL Paris (France), Copenhagen (Denmark), November 9, 2015 – Onxeo S.A. (Euronext Paris, NASDAQ Copenhagen: ONXEO), an innovative company specializing in the development of orphan oncology drugs, announced the initial results from its Phase 1 trial of belinostat, its potent, pan-HDAC (histone deacetylase) inhibitor, in combination with CHOP chemotherapy regimen as first-line treatment in patients with peripheral T-cell lymphoma (PTCL). The Bel-CHOP combination has demonstrated to be well-tolerated with all components of belinostat and CHOP given at their approved therapeutic doses. Furthermore, the efficacy data indicate that the combination is a promising new regimen in PTCL that Onxeo together with its partner Spectrum Pharmaceuticals will further evaluate in a Phase 3 randomized trial, planned to begin in 2016. The abstract has been accepted for oral presentation at the 57th American Society of Hematology (ASH) Annual Meeting & Exposition, being held December 5-8 in Orlando, FL, USA. The open-label, randomized, two-part trial enrolled a total of 23 patients, of which 11 were enrolled in the dose-escalation Part A to determine the study’s primary endpoint, the maximum tolerated dose (MTD), followed by 12 patients treated in Part B at this dose level. -

Childhood Cancer Staging for Population Registries
Childhood cancer staging for population registries according to the 1 Toronto Childhood Cancer Stage Guidelines Acknowledgements This project was funded by Cancer Australia through an initiative to strengthen national data capacity for reporting cancer stage at diagnosis. We also acknowledge and thank the Australasian Association of Cancer Registries, all Australian State and Territory Cancer Registries, the Australian Institute of Health and Welfare and the treating hospitals listed below for their support of the Australian Childhood Cancer Registry and of this project: Lady Cilento Children’s Hospital, Brisbane Sydney Children’s Hospital, Sydney The Children’s Hospital at Westmead, Sydney John Hunter Hospital, Newcastle Royal Children’s Hospital, Melbourne Monash Medical Centre, Melbourne The Women’s and Children’s Hospital, Adelaide Princess Margaret Hospital for Children, Perth Royal Hobart Hospital, Hobart Suggested citation Aitken JF, Youlden DR, Moore AS, Baade PD, Ward LJ, Thursfield VJ, Valery PC, Green AC, Gupta S, Frazier AL. Childhood cancer staging for population registries according to the Toronto Childhood Cancer Stage Guidelines. Cancer Council Queensland and Cancer Australia: Brisbane, Australia; 2017. Available at https://cancerqld.blob.core.windows.net/content/docs/childhood-cancer-staging-for- population-registries.pdf. Childhood cancer staging for population registries – November 2017 2 Table of contents Acknowledgements ........................................................................................................................................