Pain Therapy E Are There New Options on the Horizon?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Example of a Scientific Poster
Janet Robishaw, PhD Senior Associate Dean for Research Chair and Professor, Biomedical Science Florida Atlantic University Charles E. Schmidt College of Medicine Disclosures and Conflicts • I have no actual or potential conflict of interest in relation to this program/presentation. • Research support: Robishaw, MPI Robishaw, MPI R01 DA044015 R01 HL134015 Genetic Predictors of Opioid Addiction Genetic Heterogeneity of Sleep Apnea 2017-2022 2016-2021 Robishaw, PI Robishaw, MPI R01 GM114665 R01 GM111913 Novel Aspects of Golf Signaling GPCR Variants in Complex Diseases 2015-2019 2015-2019 Learning Objectives 1. Review the scope and root cause of opioid use disorder 2. Discuss the effects of opioid medications on the brain and body 3. Stress the importance of clinical judgement and discovery to address the opioid crisis 4. Highlight the clinical implications between opioid use disorder and heroin abuse Two Endemic Problems Chronic Pain Opioid Use Disorder Debilitating disorder Chronic, relapsing disorder 100 million Americans 2 million Americans Costs $630 billion dollars per year Costs $80 billion per year #1 presenting complaint to doctors # 1 cause of accidental death #1 reason for lost productivity #1 driver of heroin epidemic #1 treatment –opioid medications ? treatment Pain Relief and “Addiction” Share A Common Mechanism of Action m-Opioid Receptor Brain Regions Involved in Pleasure and Reward Increase dopamine release Brain Regions Involved in Pain Perception Brainstem Involved in Respiratory Control Spinal Cord Involved in Pain Transmission Prevent ascending transmission Turn on descending inhibitory systems These receptors are dispersed Inhibit peripheral nocioceptors throughout the body, thereby accounting for their differential Body effects on pain and reward paths. -

Biased Versus Partial Agonism in the Search for Safer Opioid Analgesics
molecules Review Biased versus Partial Agonism in the Search for Safer Opioid Analgesics Joaquim Azevedo Neto 1 , Anna Costanzini 2 , Roberto De Giorgio 2 , David G. Lambert 3 , Chiara Ruzza 1,4,* and Girolamo Calò 1 1 Department of Biomedical and Specialty Surgical Sciences, Section of Pharmacology, University of Ferrara, 44121 Ferrara, Italy; [email protected] (J.A.N.); [email protected] (G.C.) 2 Department of Morphology, Surgery, Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] (A.C.); [email protected] (R.D.G.) 3 Department of Cardiovascular Sciences, Anesthesia, Critical Care and Pain Management, University of Leicester, Leicester LE1 7RH, UK; [email protected] 4 Technopole of Ferrara, LTTA Laboratory for Advanced Therapies, 44122 Ferrara, Italy * Correspondence: [email protected] Academic Editor: Helmut Schmidhammer Received: 23 July 2020; Accepted: 23 August 2020; Published: 25 August 2020 Abstract: Opioids such as morphine—acting at the mu opioid receptor—are the mainstay for treatment of moderate to severe pain and have good efficacy in these indications. However, these drugs produce a plethora of unwanted adverse effects including respiratory depression, constipation, immune suppression and with prolonged treatment, tolerance, dependence and abuse liability. Studies in β-arrestin 2 gene knockout (βarr2( / )) animals indicate that morphine analgesia is potentiated − − while side effects are reduced, suggesting that drugs biased away from arrestin may manifest with a reduced-side-effect profile. However, there is controversy in this area with improvement of morphine-induced constipation and reduced respiratory effects in βarr2( / ) mice. Moreover, − − studies performed with mice genetically engineered with G-protein-biased mu receptors suggested increased sensitivity of these animals to both analgesic actions and side effects of opioid drugs. -

Developments in Opioid Drugs
Spotlight on drugs Developments in opioid Advanced courses 2019 analgesics Dr Andrew Wilcock DM FRCP [email protected] 1 2 1 2 Outline of talk • background – cancer pain / strong opioids Background • pharmacology • new approaches (as we go) • summary • discussion/questions. 3 4 Opioids WHO analgesic ladder for cancer pain • central to the management of moderate–severe acute pain and cancer pain. 5 6 1 Broad-spectrum analgesia Opioids: why improve? Ultimate aim to: • improve efficacy • eliminate / reduce risk of undesirable effects, e.g.: – constipation – dependence – respiratory depression – sedation – tolerance. 7 8 Opioids: chemical classification Pharmacology 9 10 Opioid: receptors Four main types: • μ • κ • δ • opioid-receptor-like 1 (OPRL-1) – opioid-related nociceptin receptor 1 – nociceptin opioid peptide (NOP) – nociceptin/orphanin FQ (N/OFQ). 11 12 2 Opioid: receptors Opioids Generally: • μ-opioid receptor clinically most relevant for analgesia and undesirable effects • Centrally: dorsal horn, higher centres – pre-synaptic: inhibit release of neurotransmitters – post-synaptic: hyperpolarize neurone • Peripherally: nerve endings, DRG, (immune cells) – inflammation upregulates opioid receptors 13 14 15 16 New approaches for opioid analgesics 17 18 3 New approaches for opioid analgesics Include: 1. Broad-spectrum 2. Injury-targeted 1. ‘Broad-spectrum’ opioid agonists 3. Biased agonists Not exhaustive list, but main finds when searching the literature. Gunther T et al. (2018); Chan HCS et al. (2017) 19 20 ‘Broad-spectrum’ opioid agonists Differential analgesic and UE of opioid receptors Targeting multiple receptors may have synergistic analgesic effects & lower UE • μ most important analgesia / UE • selective κ and δ agonists – limited analgesia / own UE – κ (e.g. -

Measuring Ligand Efficacy at the Mu- Opioid Receptor Using A
RESEARCH ARTICLE Measuring ligand efficacy at the mu- opioid receptor using a conformational biosensor Kathryn E Livingston1,2, Jacob P Mahoney1,2, Aashish Manglik3, Roger K Sunahara4, John R Traynor1,2* 1Department of Pharmacology, University of Michigan Medical School, Ann Arbor, United States; 2Edward F Domino Research Center, University of Michigan, Ann Arbor, United States; 3Department of Pharmaceutical Chemistry, School of Pharmacy, University of California San Francisco, San Francisco, United States; 4Department of Pharmacology, University of California San Diego School of Medicine, La Jolla, United States Abstract The intrinsic efficacy of orthosteric ligands acting at G-protein-coupled receptors (GPCRs) reflects their ability to stabilize active receptor states (R*) and is a major determinant of their physiological effects. Here, we present a direct way to quantify the efficacy of ligands by measuring the binding of a R*-specific biosensor to purified receptor employing interferometry. As an example, we use the mu-opioid receptor (m-OR), a prototypic class A GPCR, and its active state sensor, nanobody-39 (Nb39). We demonstrate that ligands vary in their ability to recruit Nb39 to m- OR and describe methadone, loperamide, and PZM21 as ligands that support unique R* conformation(s) of m-OR. We further show that positive allosteric modulators of m-OR promote formation of R* in addition to enhancing promotion by orthosteric agonists. Finally, we demonstrate that the technique can be utilized with heterotrimeric G protein. The method is cell- free, signal transduction-independent and is generally applicable to GPCRs. DOI: https://doi.org/10.7554/eLife.32499.001 *For correspondence: [email protected] Competing interests: The authors declare that no Introduction competing interests exist. -

Better Agonist for the Opioid Receptors Syed Lal Badshah1* , Asad Ullah1, Salim S
Badshah et al. Chemistry Central Journal (2018) 12:13 https://doi.org/10.1186/s13065-018-0383-8 COMMENTARY Open Access Better agonist for the opioid receptors Syed Lal Badshah1* , Asad Ullah1, Salim S. Al‑showiman2 and Yahia Nasser Mabkhot2* Abstract This commentary highlights the recent work published in journal Nature on the structural based discovery of novel analgesic compounds for opioid receptors with minimal efects. Manglik et al. selectively targeted the Gi based μOR pathway instead of the β-arrestin pathway of the opioids. The computational screening of millions of compounds showed a list of several competent ligands. From these ligands they synthesized the compounds with the best docking score, which were further optimized by adding side residues for better interaction with the μOR. A promis‑ ing compound, PZM21, was a selective agonist of μOR. It has better analgesic properties with minimal side efects of respiratory depression and constipation. This work is a step towards better drug designing and synthesizing in terms of efcacy, specifcity with least side efects of targeted GPCR proteins present in the human proteome. Keywords: Opioid receptors, Analgesics, Agonists, Molecular docking, Selectivity Introduction for GPCRs includes lipids, fatty acids, neurotransmitters, Morphine is the natural alkaloid present in opium and it photons, cytokines, hormones and metal ions [8, 9]. Tey is obtained from poppy plant. Opium has been used as an transduce the signal across the plasma membrane by analgesic and as a recreational drug since ancient times. binding with these ligands that causes certain conforma- Other common analgesics used include natural alkaloids tional changes into the seven trans-membrane alpha heli- like codeine, oxycodone, etc. -

Rubiscolins Are Naturally Occurring G Protein-Biased Delta Opioid Receptor Peptides
European Neuropsychopharmacology (2019) 29, 450–456 www.elsevier.com/locate/euroneuro SHORT COMMUNICATION Rubiscolins are naturally occurring G protein-biased delta opioid receptor peptides a , 1 a, 1 a Robert J. Cassell , Kendall L. Mores , Breanna L. Zerfas , a a, b , c a ,b , c Amr H. Mahmoud , Markus A. Lill , Darci J. Trader , a, b ,c , ∗ Richard M. van Rijn a Department of Medicinal Chemistry and Molecular Pharmacology, College of Pharmacy, Purdue University, West Lafayette, IN 47907, USA b Purdue Institute for Drug Discovery, West Lafayette, IN 47907, USA c Purdue Institute for Integrative Neuroscience, West Lafayette, IN 47907, USA Received 6 August 2018; received in revised form 19 November 2018; accepted 16 December 2018 KEYWORDS Abstract Delta opioid receptor; The impact that β-arrestin proteins have on G protein-coupled receptor trafficking, signaling Beta-arrestin; and physiological behavior has gained much appreciation over the past decade. A number of Natural products; studies have attributed the side effects associated with the use of naturally occurring and syn- Biased signaling; thetic opioids, such as respiratory depression and constipation, to excessive recruitment of Rubisco; β-arrestin. These findings have led to the development of biased opioid small molecule ago- G protein-coupled nists that do not recruit β-arrestin, activating only the canonical G protein pathway. Similar G receptor protein-biased small molecule opioids have been found to occur in nature, particularly within kratom, and opioids within salvia have served as a template for the synthesis of other G protein- biased opioids. Here, we present the first report of naturally occurring peptides that selectively activate G protein signaling pathways at δ opioid receptors, but with minimal β-arrestin recruit- ment. -

Influence of G Protein-Biased Agonists of Μ-Opioid Receptor on Addiction-Related Behaviors
Pharmacological Reports https://doi.org/10.1007/s43440-021-00251-1 SPECIAL ISSUE: REVIEW Infuence of G protein‑biased agonists of μ‑opioid receptor on addiction‑related behaviors Lucja Kudla1 · Ryszard Przewlocki1 Received: 31 January 2021 / Revised: 5 March 2021 / Accepted: 16 March 2021 © The Author(s) 2021 Abstract Opioid analgesics remain a gold standard for the treatment of moderate to severe pain. However, their clinical utility is seriously limited by a range of adverse efects. Among them, their high-addictive potential appears as very important, espe- cially in the context of the opioid epidemic. Therefore, the development of safer opioid analgesics with low abuse potential appears as a challenging problem for opioid research. Among the last few decades, diferent approaches to the discovery of novel opioid drugs have been assessed. One of the most promising is the development of G protein-biased opioid agonists, which can activate only selected intracellular signaling pathways. To date, discoveries of several biased agonists acting via μ-opioid receptor were reported. According to the experimental data, such ligands may be devoid of at least some of the opioid side efects, such as respiratory depression or constipation. Nevertheless, most data regarding the addictive properties of biased μ-opioid receptor agonists are inconsistent. A global problem connected with opioid abuse also requires the search for efective pharmacotherapy for opioid addiction, which is another potential application of biased compounds. This review discusses the state-of-the-art on addictive properties of G protein-biased μ-opioid receptor agonists as well as we analyze whether these compounds can diminish any symptoms of opioid addiction. -

February 2019 Director's Report
TABLE OF CONTENTS RESEARCH HIGHLIGHTS…………….………………………………………………………. 1 GRANTEE HONORS AND AWARDS…………………………………………………………. 36 STAFF HONORS AND AWARDS…………………………………………………………….... 37 STAFF CHANGES…………………………………………………………………………….…. 43 IN MEMORIAM………………………………………………………………………………….. 48 RESEARCH FINDINGS BASIC AND BEHAVIORAL RESEARCH Adolescent Exposure To Δ9-Tetrahydrocannabinol Alters the Transcriptional Trajectory and Dendritic Architecture of Prefrontal Pyramidal Neurons Michael L. Miller, Benjamin Chadwick, Dara L. Dickstein, Immanuel Purushothaman, Gabor Egervari, Tanni Rahman, Chloe Tessereau, Patrick R. Hof, Panos Roussos, Li Shen, Mark G. Baxter, Yasmin L. Hurd; Mol. Psychiatry 2018. Neuronal circuits within the prefrontal cortex (PFC) mediate higher cognitive functions and emotional regulation that are disrupted in psychiatric disorders. The PFC undergoes significant maturation during adolescence, a period when cannabis use in humans has been linked to subsequent vulnerability to psychiatric disorders such as addiction and schizophrenia. Here, the authors investigated in a rat model the effects of adolescent exposure to Δ9-tetrahydrocannabinol (THC), a psychoactive component of cannabis, on the morphological architecture and transcriptional profile of layer III pyramidal neurons-using cell type- and layer-specific high- resolution microscopy, laser capture microdissection and next-generation RNA-sequencing. The results confirmed known normal expansions in basal dendritic arborization and dendritic spine pruning during the transition from late -

Replacement of Current Opioid Drugs Focusing on MOR-Related Strategies
JPT-107519; No of Pages 17 Pharmacology & Therapeutics xxx (2020) xxx Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Replacement of current opioid drugs focusing on MOR-related strategies Jérôme Busserolles a,b, Stéphane Lolignier a,b, Nicolas Kerckhove a,b,c, Célian Bertin a,b,c, Nicolas Authier a,b,c, Alain Eschalier a,b,⁎ a Université Clermont Auvergne, INSERM, CHU, NEURO-DOL Pharmacologie Fondamentale et Clinique de la douleur, F-63000 Clermont-Ferrand, France b Institut ANALGESIA, Faculté de Médecine, F-63000 Clermont-Ferrand, France c Observatoire Français des Médicaments Antalgiques (OFMA), French monitoring centre for analgesic drugs, CHU, F-63000 Clermont-Ferrand, France article info abstract Available online xxxx The scarcity and limited risk/benefit ratio of painkillers available on the market, in addition to the opioid crisis, warrant reflection on new innovation strategies. The pharmacopoeia of analgesics is based on products that are often old and derived from clinical empiricism, with limited efficacy or spectrum of action, or resulting in Keywords: an unsatisfactory tolerability profile. Although they are reference analgesics for nociceptive pain, opioids are sub- Analgesia ject to the same criticism. The use of opium as an analgesic is historical. Morphine was synthesized at the begin- Mu opioid receptors (MORs) ning of the 19th century. The efficacy of opioids is limited in certain painful contexts and these drugs can induce Opioid adverse side effects potentially serious and fatal adverse effects. The current North American opioid crisis, with an ever-rising number Opioid abuse and misuse of deaths by opioid overdose, is a tragic illustration of this. -

Director's Report to the National Advisory Council on Drug Abuse
Director’s Report to the National Advisory Council on Drug Abuse Nora D. Volkow, M.D. Director National Institute on Drug Abuse May 11, 2021 1 NIDA BUDGET FY 2020 ($k) FY 2021 ($k) FY 2022 PB ($k) Base $1,191,362 $1,210,014 HEAL $266,321* $270,295* TBD Total $1,457,683 $1,480,309 *NIH’s total HEAL funding is split evenly between NIDA and NINDS FY 20 Funding Overview Non-HEAL Research HEAL Research* *Includes all NIDA HEAL projects regardless of funding source Adolescent Brain Cognitive Development Study 98.5 Percent Retained As of April 2021 Adolescent Brain Cognitive Development Study (ABCD): Progress up to April 2021 145 papers, half from ABCD, half from non-ABCD investigators Imaging Completion QUESTIONNAIRE AND COGNITIVE DATA Baseline 1-year 2-year 3-year ABCD Baseline 2-year FU 100 90 80 70 60 50 40 30 PERCENT OF OF PERCENT PARTICIPANTS 20 10 0 REDCAP KSADS PARENT KSADS YOUTH NIH TB hBCD Study Longitudinal study to understand normative neurodevelopment from birth to 9-10 years with an emphasis on assessing the impact of in utero exposures to drugs and harmful environments Phase 1 Accomplishments • Training for research coordinators • Purchased Sprinter van to demonstrate feasibility of scanning remotely • MRI compatible crib to image newborns and infants • Developed a multimodal protocol using EEG and • Summit of families, legal scholars, ethicists, healthcare MRI to assess brain structure, function, and providers, and relevant agencies to mitigate risk and connectivity. maximize benefit to women and children enrolled • Conducted extensive literature review of • Workshop on bioethics recruitment and retention with vulnerable • Motion correction system developed and tested populations • Protocols for remotely collecting saliva and stool • Conducted state by state assessment of legal and ethical issues related to substance use and Protocols for MRI data collection in infants with • pregnancy in research neonatal abstinence syndrome (NAS) created 6 6 Intersection Between Drug Crisis and COVID-19 . -

Medical Research to Address the Opioid Crisis in the United States
Medical research to address the opioid crisis in the United States Iván D. Montoya, M.D., M.P.H. Deputy Director, Division of Therapeutics and Medical Consequences NIDA Bolliger, 2019 • “Aggressive, trans-agency effort to speed scientific solutions to stem the national opioid public health crisis.” • Build on extensive, well-established NIH research including: • Basic science of neurological pathways involved in pain and OUD • Clinical studies of safer and more effective treatments for pain and OUD • Implementation science to develop and test treatment models Clinical Pre-Clinical Research in Research in Pain Pain Enhancing Pain Management Management Expand Enhance Treatments Therapeutic Improving Treatments for Affected Options for Misuse and Newborns Addiction Develop New/ Improved Optimize Prevention & Effective Treatment Treatments Strategies NIDA HEAL Projects • Expanding therapeutic options for Opioid Use Disorder and Overdose • Enhancing the NIDA Clinical Trials Network • HEALing Communities Study • Justice Community Opioid Innovation Network (JCOIN) • Preventing At-Risk Adolescents Transitioning into Adulthood from Developing Opioid Use Disorder • HEALthy Brain and Child Development Study https://www.drugabuse.gov/drugs-abuse/opioids/nidas-role-in-nih-heal-initiative FDA-Approved Medications for Opioid Addiction and Overdose • Methadone • Buprenorphine • Sublingual • Monthly injection • Six month implant • Naltrexone • Oral • Monthly • Lofexidine • Naloxone • Parenteral • Nasal Close interaction with FDA Expand therapeutic options -
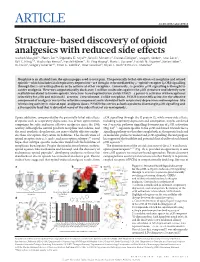
Structure-Based Discovery of Opioid Analgesics with Reduced Side Effects Aashish Manglik1*, Henry Lin2*, Dipendra K
ARTICLE doi:10.1038/nature19112 Structure-based discovery of opioid analgesics with reduced side effects Aashish Manglik1*, Henry Lin2*, Dipendra K. Aryal3*, John D. McCorvy3, Daniela Dengler4, Gregory Corder5, Anat Levit2, Ralf C. Kling4,6, Viachaslau Bernat4, Harald Hübner4, Xi-Ping Huang3, Maria F. Sassano3, Patrick M. Giguère3, Stefan Löber4, Da Duan2, Grégory Scherrer1,5, Brian K. Kobilka1, Peter Gmeiner4, Bryan L. Roth3 & Brian K. Shoichet2 Morphine is an alkaloid from the opium poppy used to treat pain. The potentially lethal side effects of morphine and related opioids—which include fatal respiratory depression—are thought to be mediated by μ-opioid-receptor (μOR) signalling through the β-arrestin pathway or by actions at other receptors. Conversely, G-protein μOR signalling is thought to confer analgesia. Here we computationally dock over 3 million molecules against the μOR structure and identify new scaffolds unrelated to known opioids. Structure-based optimization yields PZM21—a potent Gi activator with exceptional selectivity for μOR and minimal β-arrestin-2 recruitment. Unlike morphine, PZM21 is more efficacious for the affective component of analgesia versus the reflexive component and is devoid of both respiratory depression and morphine-like reinforcing activity in mice at equi-analgesic doses. PZM21 thus serves as both a probe to disentangle μOR signalling and a therapeutic lead that is devoid of many of the side effects of current opioids. Opiate addiction, compounded by the potentially lethal side effects μ OR signalling through the G protein Gi, while many side effects, of opiates such as respiratory depression, has driven optimization including respiratory depression and constipation, may be conferred campaigns for safer and more effective analgesics since the 19th via β -arrestin pathway signalling downstream of μ OR activation 4–6 century.