EMS Policies and Procedures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Public Notices & the Courts
PUBLIC NOTICES B1 DAILY BUSINESS REVIEW TUESDAY, SEPTEMBER 28, 2021 dailybusinessreview.com & THE COURTS BROWARD PUBLIC NOTICES BUSINESS LEADS THE COURTS WEB SEARCH FORECLOSURE NOTICES: Notices of Action, NEW CASES FILED: US District Court, circuit court, EMERGENCY JUDGES: Listing of emergency judges Search our extensive database of public notices for Notices of Sale, Tax Deeds B5 family civil and probate cases B2 on duty at night and on weekends in civil, probate, FREE. Search for past, present and future notices in criminal, juvenile circuit and county courts. Also duty Miami-Dade, Broward and Palm Beach. SALES: Auto, warehouse items and other BUSINESS TAX RECEIPTS (OCCUPATIONAL Magistrate and Federal Court Judges B14 properties for sale B8 LICENSES): Names, addresses, phone numbers Simply visit: CALENDARS: Suspensions in Miami-Dade, Broward, FICTITIOUS NAMES: Notices of intent and type of business of those who have received https://www.law.com/dailybusinessreview/public-notices/ and Palm Beach. Confirmation of judges’ daily motion to register business licenses B3 calendars in Miami-Dade B14 To search foreclosure sales by sale date visit: MARRIAGE LICENSES: Name, date of birth and city FAMILY MATTERS: Marriage dissolutions, adoptions, https://www.law.com/dailybusinessreview/foreclosures/ DIRECTORIES: Addresses, telephone numbers, and termination of parental rights B8 of those issued marriage licenses B3 names, and contact information for circuit and CREDIT INFORMATION: Liens filed against PROBATE NOTICES: Notices to Creditors, county -

No Limits Freediving
1 No Limits Freediving "The challenges to the respiratory function of the breath-hold diver' are formidable. One has to marvel at the ability of the human body to cope with stresses that far exceed what normal terrestrial life requires." Claes Lundgren, Director, Center for Research and Education in Special Environments A woman in a deeply relaxed state floats in the water next to a diving buoy. She is clad in a figure-hugging wetsuit, a dive computer strapped to her right wrist, and another to her calf. She wears strange form-hugging silicone goggles that distort her eyes, giving her a strange bug-eyed appearance. A couple of meters away, five support divers tread water near a diving platform, watching her perform an elaborate breathing ritual while she hangs onto a metal tube fitted with two crossbars. A few meters below the buoy, we see that the metal tube is in fact a weighted sled attached to a cable descending into the dark-blue water. Her eyes are still closed as she begins performing a series of final inhalations, breathing faster and faster. Photographers on the media boats snap pictures as she performs her final few deep and long hyperventilations, eliminating carbon dioxide from her body. Then, a thumbs-up to her surface crew, a pinch of the nose clip, one final lungful of air, and the woman closes her eyes, wraps her knees around the bottom bar of the sled, releases a brake device, and disappears gracefully beneath the waves. The harsh sounds of the wind and waves suddenly cease and are replaced by the effervescent bubbling of air being released from the regulators of scuba-divers. -

18. Fluctuations in Productivity and Upwelling Intensity at Site 1083
Wefer, G., Berger, W.H., and Richter, C. (Eds.) Proceedings of the Ocean Drilling Program, Scientific Results Volume 175 18. FLUCTUATIONS IN PRODUCTIVITY AND UPWELLING INTENSITY AT SITE 1083 DURING THE INTENSIFICATION OF THE 1Ettwein, V.J., Stickley, C.E., Maslin, M.A., Laurie, E.R., Rosell-Melé, A., NORTHERN HEMISPHERE GLACIATION Vidal, L., and Brownless, M., 2001. Fluctuations in productivity and (2.40–2.65 MA)1 upwelling intensity at Site 1083 during the intensification of the Northern Hemisphere glaciation V.J. Ettwein,2,3 C.E. Stickley,2 M.A. Maslin,2 E.R. Laurie,2,3 (2.40–2.65 Ma). In Wefer, G., Berger, A. Rosell-Melé,4 L. Vidal,5 and M. Brownless6 W.H., and Richter, C. (Eds.), Proc. ODP, Sci. Results,175, 1–25 [Online]. Available from World Wide Web: <http://www-odp.tamu.edu/ publications/175_SR/VOLUME/ CHAPTERS/SR175_18.PDF>. [Cited YYYY-MM-DD] 2Environmental Change Research Centre, Department of Geography, University College London, 26 Bedford Way, London WC1H 0AP, United Kingdom. Correspondence ABSTRACT author: [email protected] 3Centre for Quaternary Research, Coastal upwelling regions play an important role in regulating the Department of Geography, Royal Holloway, University of London, partial pressure of CO2, because they are zones of intense productivity and therefore contribute considerably to the drawdown mechanism. Egham, Surrey TW20 0EX, United Kingdom. One of the major aims of Leg 175 was to develop an understanding of 4Quaternary Environmental Change the relationship between wind-driven upwelling intensity and surface Research Group, Department of water productivity. In this paper, such a relationship during the late Geography, University of Durham, Pliocene intensification of the Northern Hemisphere glaciation (INHG) Science Site, South Road, Durham ~2.54 Ma is examined. -

Maryland Casualty Producer State and General Sections Series 20-07 & 20-08 80 Scored Questions (Plus 10 Unscored)
Maryland Casualty Producer State and General Sections Series 20-07 & 20-08 80 scored questions (plus 10 unscored) Casualty Producer State Section Series 20-08 35 questions- 45-minute time limit 1.0 Insurance Regulation 1.1 Licensing 17% (5 items) Purpose Process (Insurance Article Annotated Code- Sec. 10-115; Sec.10-116; Sec. 10-104) Initial Licensure Qualifications Examination License fee & application Exemptions to Licensure Types of licensees Producers Business entity producers Nonresident producers Temporary Advisers Public insurance adjusters Limited Lines Producer Portable Electronics Insurance Limited Lines license Maintenance and duration (Insurance Article Annotated Code- Sec. 10-116; Sec. 10-117(b)(1)) Reinstatement and renewal Address change Reporting of actions Assumed names Continuing education requirements, exemptions and penalties Disciplinary actions Cease and desist order Hearings Probation, suspension, revocation, refusal to issue or renew Penalties and fines 1.2 State regulation 17% (5 items) Commissioner's general duties and powers (Insurance Article Annotated Code-Sec. 2-205 (a)(2)) State Specific Definitions (Insurance Article Annotated Code- Sec. 10-401; Sec. 27-209; Sec. 27-213; Sec. 10-201; Sec 10-126; Ref: COMAR Sec. 31.08.06.02) Company regulation Certificate of authority Solvency Rates Policy forms Examination of books and records Producer appointments Producer's Contract with Insurer versus Producer's Appointment with Insurer 1 Producer's Individual Appointment versus Business Entity Appointment Maintaining Record of Appointment Notice Termination of producer appointment Producer regulation (Insurance Article Annotated Code-Sec. 27-212(d)) Examination of Books and Records Insurance Information and Privacy Protection Fiduciary Responsibilities (COMAR- Sec. 31.03.03) Bail Bond (COMAR- Sec. -
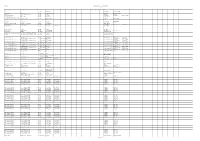
DACIN SARA Repartitie Aferenta Trimestrului III 2019 Straini TITLU
DACIN SARA Repartitie aferenta trimestrului III 2019 Straini TITLU TITLU ORIGINAL AN TARA R1 R2 R3 R4 R5 R6 R7 R8 R9 R10 R11 S1 S2 S3 S4 S5 S6 S7 S8 S9 S10 S11 S12 S13 S14 S15 Greg Pruss - Gregory 13 13 2010 US Gela Babluani Gela Babluani Pruss 1000 post Terra After Earth 2013 US M. Night Shyamalan Gary Whitta M. Night Shyamalan 30 de nopti 30 Days of Night: Dark Days 2010 US Ben Ketai Ben Ketai Steve Niles 300-Eroii de la Termopile 300 2006 US Zack Snyder Kurt Johnstad Zack Snyder Michael B. Gordon 6 moduri de a muri 6 Ways to Die 2015 US Nadeem Soumah Nadeem Soumah 7 prichindei cuceresc Broadway-ul / Sapte The Seven Little Foys 1955 US Melville Shavelson Jack Rose Melville Shavelson prichindei cuceresc Broadway-ul A 25-a ora 25th Hour 2002 US Spike Lee David Benioff Elaine Goldsmith- A doua sansa Second Act 2018 US Peter Segal Justin Zackham Thomas A fost o data in Mexic-Desperado 2 Once Upon a Time in Mexico 2003 US Robert Rodriguez Robert Rodriguez A fost odata Curly Once Upon a Time 1944 US Alexander Hall Lewis Meltzer Oscar Saul Irving Fineman A naibii dragoste Crazy, Stupid, Love. 2011 US Glenn Ficarra John Requa Dan Fogelman Abandon - Puzzle psihologic Abandon 2002 US Stephen Gaghan Stephen Gaghan Acasa la coana mare 2 Big Momma's House 2 2006 US John Whitesell Don Rhymer Actiune de recuperare Extraction 2013 US Tony Giglio Tony Giglio Acum sunt 13 Ocean's Thirteen 2007 US Steven Soderbergh Brian Koppelman David Levien Acvila Legiunii a IX-a The Eagle 2011 GB/US Kevin Macdonald Jeremy Brock - ALCS Les aventures extraordinaires d'Adele Blanc- Adele Blanc Sec - Aventurile extraordinare Luc Besson - Sec - The Extraordinary Adventures of Adele 2010 FR/US Luc Besson - SACD/ALCS ale Adelei SACD/ALCS Blanc - Sec Adevarul despre criza Inside Job 2010 US Charles Ferguson Charles Ferguson Chad Beck Adam Bolt Adevarul gol-golut The Ugly Truth 2009 US Robert Luketic Karen McCullah Kirsten Smith Nicole Eastman Lebt wohl, Genossen - Kollaps (1990-1991) - CZ/DE/FR/HU Andrei Nekrasov - Gyoergy Dalos - VG. -

Civilian Killings and Disappearances During Civil War in El Salvador (1980–1992)
DEMOGRAPHIC RESEARCH A peer-reviewed, open-access journal of population sciences DEMOGRAPHIC RESEARCH VOLUME 41, ARTICLE 27, PAGES 781–814 PUBLISHED 1 OCTOBER 2019 http://www.demographic-research.org/Volumes/Vol41/27/ DOI: 10.4054/DemRes.2019.41.27 Research Article Civilian killings and disappearances during civil war in El Salvador (1980–1992) Amelia Hoover Green Patrick Ball c 2019 Amelia Hoover Green & Patrick Ball. This open-access work is published under the terms of the Creative Commons Attribution 3.0 Germany (CC BY 3.0 DE), which permits use, reproduction, and distribution in any medium, provided the original author(s) and source are given credit. See https://creativecommons.org/licenses/by/3.0/de/legalcode Contents 1 Introduction 782 2 Background 783 3 Methods 785 3.1 Methodological overview 785 3.2 Assumptions of the model 786 3.3 Data sources 787 3.4 Matching and merging across datasets 790 3.5 Stratification 792 3.6 Estimation procedure 795 4 Results 799 4.1 Spatial variation 799 4.2 Temporal variation 802 4.3 Global estimates 803 4.3.1 Sums over strata 805 5 Discussion 807 6 Conclusions 808 References 810 Demographic Research: Volume 41, Article 27 Research Article Civilian killings and disappearances during civil war in El Salvador (1980–1992) Amelia Hoover Green1 Patrick Ball2 Abstract BACKGROUND Debate over the civilian toll of El Salvador’s civil war (1980–1992) raged throughout the conflict and its aftermath. Apologists for the Salvadoran regime claimed no more than 20,000 had died, while some activists placed the toll at 100,000 or more. -

American War and Military Operations Casualties: Lists and Statistics
American War and Military Operations Casualties: Lists and Statistics Updated July 29, 2020 Congressional Research Service https://crsreports.congress.gov RL32492 American War and Military Operations Casualties: Lists and Statistics Summary This report provides U.S. war casualty statistics. It includes data tables containing the number of casualties among American military personnel who served in principal wars and combat operations from 1775 to the present. It also includes data on those wounded in action and information such as race and ethnicity, gender, branch of service, and cause of death. The tables are compiled from various Department of Defense (DOD) sources. Wars covered include the Revolutionary War, the War of 1812, the Mexican War, the Civil War, the Spanish-American War, World War I, World War II, the Korean War, the Vietnam Conflict, and the Persian Gulf War. Military operations covered include the Iranian Hostage Rescue Mission; Lebanon Peacekeeping; Urgent Fury in Grenada; Just Cause in Panama; Desert Shield and Desert Storm; Restore Hope in Somalia; Uphold Democracy in Haiti; Operation Enduring Freedom (OEF); Operation Iraqi Freedom (OIF); Operation New Dawn (OND); Operation Inherent Resolve (OIR); and Operation Freedom’s Sentinel (OFS). Starting with the Korean War and the more recent conflicts, this report includes additional detailed information on types of casualties and, when available, demographics. It also cites a number of resources for further information, including sources of historical statistics on active duty military deaths, published lists of military personnel killed in combat actions, data on demographic indicators among U.S. military personnel, related websites, and relevant CRS reports. Congressional Research Service American War and Military Operations Casualties: Lists and Statistics Contents Introduction .................................................................................................................................... -

MASS CASUALTY TRAUMA TRIAGE PARADIGMS and PITFALLS July 2019
1 Mass Casualty Trauma Triage - Paradigms and Pitfalls EXECUTIVE SUMMARY Emergency medical services (EMS) providers arrive on the scene of a mass casualty incident (MCI) and implement triage, moving green patients to a single area and grouping red and yellow patients using triage tape or tags. Patients are then transported to local hospitals according to their priority group. Tagged patients arrive at the hospital and are assessed and treated according to their priority. Though this triage process may not exactly describe your agency’s system, this traditional approach to MCIs is the model that has been used to train American EMS As a nation, we’ve got a lot providers for decades. Unfortunately—especially in of trailers with backboards mass violence incidents involving patients with time- and colored tape out there critical injuries and ongoing threats to responders and patients—this model may not be feasible and may result and that’s not what the focus in mis-triage and avoidable, outcome-altering delays of mass casualty response is in care. Further, many hospitals have not trained or about anymore. exercised triage or re-triage of exceedingly large numbers of patients, nor practiced a formalized secondary triage Dr. Edward Racht process that prioritizes patients for operative intervention American Medical Response or transfer to other facilities. The focus of this paper is to alert EMS medical directors and EMS systems planners and hospital emergency planners to key differences between “conventional” MCIs and mass violence events when: • the scene is dynamic, • the number of patients far exceeds usual resources; and • usual triage and treatment paradigms may fail. -

Hawaii Administrative Rules Title 13 Department of Land
HAWAII ADMINISTRATIVE RULES TITLE 13 DEPARTMENT OF LAND AND NATURAL RESOURCES SUBTITLE 4 FISHERIES PART II MARINE FISHERIES MANAGEMENT AREAS CHAPTER 47 HILO BAY, WAILOA RIVER AND WAILUKU RIVER, HAWAII §13-47-1 Definitions §13-47-2 Prohibited activities §13-47-3 Permitted activities §13-47-4 Penalty Historical Note. Chapter 47 of Title 13 is based substantially upon Regulation 35 of the Division of Fish and Game, Department of Land and Natural Resources, State of Hawaii. [Eff 3/23/70; am 11/22/73; R 5/26/81] §13-47-1 Definitions. As used in this chapter unless otherwise provided: “Hilo Harbor” means the waters of that portion of the bay in Hilo bounded by the breakwater, thence along a line from the tip of the breakwater southwestward to Alealea Point, then along the shoreline to the inshore end of the breakwater as delineated in “Locations and Landmarks of Hilo Harbor, Wailoa River and Wailuku River, Hawaii 11/12/87” attached at the end of this chapter. “Moi” means any fish known as Polydactylus sexfilis or a recognized synonym. Also known as, among other names, moi li’i, mana moi, pala moi, pacific threadfin, and six-fingered threadfin. “Mullet” means any fish known as Mugil cephalus or a recognized synonym. The young of this species are known as, among other names, pua ama’ama, pua, po’ola, and o’ola. Also known as, among other names, ama’ama, 47-1 §13-47-1 anae, anaeholo, anaepali, gray mullet and striped mullet. “Netting” means the taking or killing of fish by means of any net except throw nets, opae/dip nets, crab nets, and nehu nets. -

James Hillier
14 City Lofts 112-116 Tabernacle Street London EC2A 4LE offi[email protected] +44 (0) 20 7734 6441 JAMES HILLIER Shadow & Bone Small Axe The Crown Television Role Title Production Company Director DCI Bill Raynott STEPHEN Hat Trick for ITV Alrick Riley Tony Leech DECEIT Story Films Niall MacCormack Jack Cocker CLOSE TO ME Viaplay / Channel 4 Michael Samuels Captain Churik SHADOW & BONE 21 Laps Entertainment / Netflix Lee Toland Krieger / Eric Heisserer Chief Inspector SMALL AXE BBC / Amazon Studios Steve McQueen Dr Stu Ford DOCTORS BBC Dan Wilson The Equerry (Series Regular) THE CROWN SEASON TWO Left Bank Pictures / Netflix Stephen Daldry Nathan Stone PRIME SUSPECT 1973 Noho / ITV David Caffrey The Equerry (Series Regular) THE CROWN SEASON ONE TVE Various Oliver Grau (Series Regular) MERLÍ SEASON 1 Left Bank Pictures / Netflix Stephen Daldry Joseph McCoy FRONTIER Raw TV Ben Chanan James Downing CASUALTY BBC Jon Sen Admiral Nelson THE BRITISH Nutopia Jenny Ash Chris LONDON’S BURNING Juniper Justin Hardy Mick SURVIVORS BBC Ian B. McDonald Sgt Christian Young (Series HOLBY BLUE SERIES TWO BBC / Kudos Martin Hutchins Regular) Damian EASTENDERS BBC Michael Kellior Sgt Christian Young (Series HOLBY BLUE SERIES ONE BBC / Kudos Martin Hutchins Regular) Keith Spalding GOLDPLATED Channel 4 Julie Ann Robinson / Robert Delamere Robert Barrie (Recurring) THE BILL Talkback Thames Bill Scot-Rider Marcus Octavius THE RISE AND FALL OF ROME: BBC Chris Spencer REVOLUTION Garret Gibbens BLACKBEARD Dangerous Films Richard Dale Darren HOLBY CITY BBC Nick Adams Jeremy -

Breath-Hold Diving – in Contrast to Carefully Developed a Proposed 60-Second Rule Scuba Courses, Most Divers Don't Get Specific Instruction in Breath-Hold by Capt
Breath-Hold Diving – In contrast to carefully developed A Proposed 60-second Rule scuba courses, most divers don't get specific instruction in breath-hold By Capt. Dr. Frank Butler, dive techniques before they begin; they pretty much do what comes Medical Corps, USN naturally, which is to take a deep CASE STUDY breath and stay down until the urge to breathe becomes overpowering Late last year DAN SEAP was called in to assist one of our members who (the so-called "breakpoint"). had nearly perished after attempting multiple, extended breathhold dives. This strategy works well - most of The diver, a very experienced breathhold diver, had been attempting the time. Many deaths occur from a series of breathhold dives near the rear of the boat. He decided to breath-hold diving because some continue after his companions left the water. Fortunately he was noticed divers have enough willpower to quickly after surfacing, unconscious. He was rapidly retrieved into the suppress the urge to breathe long tender and rolled onto his side before vomiting his stomach contents. enough that they suffer an underwater He was initially incoherent, but later became more responsive, was hypoxic loss of consciousness (HLOC). provided with supplemental oxygen and improved steadily. He was transported to hospital for assessment and later discharged. Luckily, The competitive spirit common he had only suffered from salt water aspiration syndrome. If he had among freedivers probably increases not been seen and recovered so quickly and effectively, he could easily have drowned. He had done a series of 13 consecutive breathhold dives. This last dive was to around 21m for approximately 1 minute 28 seconds. -

Tuesday September 3, 1996
9±3±96 Tuesday Vol. 61 No. 171 September 3, 1996 Pages 46373±46528 Briefings on How To Use the Federal Register For information on briefings in New York, NY and Washington, DC, see announcement on the inside cover of this issue. federal register 1 II Federal Register / Vol. 61, No. 171 / Tuesday, September 3, 1996 SUBSCRIPTIONS AND COPIES PUBLIC Subscriptions: Paper or fiche 202±512±1800 FEDERAL REGISTER Published daily, Monday through Friday, Assistance with public subscriptions 512±1806 (not published on Saturdays, Sundays, or on official holidays), by General online information 202±512±1530 the Office of the Federal Register, National Archives and Records Administration, Washington, DC 20408, under the Federal Register Single copies/back copies: Act (49 Stat. 500, as amended; 44 U.S.C. Ch. 15) and the Paper or fiche 512±1800 regulations of the Administrative Committee of the Federal Register Assistance with public single copies 512±1803 (1 CFR Ch. I). Distribution is made only by the Superintendent of Documents, U.S. Government Printing Office, Washington, DC FEDERAL AGENCIES 20402. Subscriptions: The Federal Register provides a uniform system for making Paper or fiche 523±5243 available to the public regulations and legal notices issued by Assistance with Federal agency subscriptions 523±5243 Federal agencies. These include Presidential proclamations and For other telephone numbers, see the Reader Aids section Executive Orders and Federal agency documents having general applicability and legal effect, documents required to be published at the end of this issue. by act of Congress and other Federal agency documents of public interest. Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless FEDERAL REGISTER WORKSHOP earlier filing is requested by the issuing agency.