Case Reports in Clinical Practice a Brown Tumor Simulating Bone Metastases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Rare Cause of Lytic Lesion: the Brown Tumors
MOJ Orthopedics & Rheumatology Case Report Open Access A rare cause of lytic lesion: the brown tumors Abstract Volume 11 Issue 6 - 2019 Introduction: Brown tumor is a tumor-like lesion that represents the terminal stage of the bone remodeling process in prolonged hyperparathyroidism and has an overall incidence of Maroua Khaloui, Fatma Daoud, Imène Rachdi, 3%. It may not be distinguishable from other osteolytic lesions of malignancy. We illustrate Mehdi Somai, Hana Zoubeidi, Zohra Aydi, a case of primary hyperparathyroidism with brown tumour which was initially mistaken for Nedia Hammami, Wided Hizem, Besma Ben malignant disease. Dhaou, Fatma Boussema Department of Internal medicine, Habib Thameur Hospital, Tunis Case report: A 64-year-old female patient with a medical history of dyslipidemia repeated El Manar University, Tunisia acute pancreatitis and retrobulbar neuritis was referred to our department for evaluation of hypercalcemia. The association with a hypogammaglobulinemia gave rise to the initial Correspondence: Imène Rachdi, Department of Internal diagnosis of humoral hypercalcemia of multiple myeloma. The radiological evaluation medicine, Habib Thameur Hospital, Tunis El Manar University, Ali of the skeleton showed an isolated lytic lesion on the humerus. No electrophoretic signs Ben Ayed Street, 1089 Tunis, Tunisia, of monoclonal secretion in the blood or urine were found. Nevertheless, laboratory Email investigations revealed a constellation of primary hyperparathyroidism. Computed tomography localized a right parathyroid adenoma, which was surgically removed. Also, Received: October 25, 2019 | Published: November 15, 2019 we concluded that the humeral lesion was in fact a Brown tumor. Conclusion: This case reinforces the need to consider brown tumor of hyperparathyroidism in the differential diagnosis of an osteolytic lesion with hypercalcemia. -

Jaw Tumor: an Uncommon Presenting Manifestation of Primary Hyperparathyroidism Jaw Tumor: an Uncommon Presenting Manifestation of Primary Hyperparathyroidism
WJOES CASE REPORT Jaw Tumor: An Uncommon Presenting Manifestation of Primary Hyperparathyroidism Jaw Tumor: An Uncommon Presenting Manifestation of Primary Hyperparathyroidism 1Roy Phitayakorn, 2Christopher R McHenry 1Department of Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, MA 2Department of Surgery, MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH Correspondence: Roy Phitayakorn, Department of Surgery, Massachusetts General Hospital, WACC 460 E, 15 Parkman Street, Boston, MA 02114, USA, Phone: (617) 643-0544, Fax: (617) 724-2574, e-mail: [email protected] ABSTRACT Introduction: To report two unusual cases of primary hyperparathyroidism (HPT) that initially manifested with a “ jaw tumor” and to discuss the clinical implications of a giant cell granuloma vs an ossifying fibroma of the jaw. Material and methods: The history, physical examination, laboratory values and the imaging and pathologic findings are described in two patients who presented with a “jaw tumor” and were subsequently diagnosed with primary HPT. The diagnosis and management of osteitis fibrosa cystica and HPT-jaw tumor syndrome are reviewed. Results: Patient #1 was a 70-year-old male who presented with hypercalcemia, severe jaw pain, and an enlarging mass in his mandible. Biopsy of the mass revealed a giant cell tumor and he was subsequently diagnosed with primary HPT. A sestamibi scan demonstrated a single focus of abnormal radiotracer accumulation, corresponding to a 13,470 mg parathyroid adenoma, which was resected. Postoperatively, the serum calcium normalized and the giant cell granuloma regressed spontaneously. Patient #2 was a 36-year-old male with four incidentally discovered tumors of the mandible and maxilla, who was diagnosed with normocalcemic HPT and vitamin D deficiency. -

Oncogenic Osteomalacia
ONCOGENIC_Martini 14/06/2006 10.27 Pagina 76 Case report Oncogenic osteomalacia Giuseppe Martini choice; if the tumour cannot be found or if the tumour is unre- Fabrizio Valleggi sectable for its location, chronic administration of phosphate Luigi Gennari and calcitriol is indicated. Daniela Merlotti KEY WORDS: oncogenic osteomalacia, hypophosphoremia, fractures, oc- Vincenzo De Paola treotide scintigraphy. Roberto Valenti Ranuccio Nuti Introduction Department of Internal Medicine, Endocrine-Metabolic Sciences and Biochemistry, University of Siena, Italy Osteomalacia is a metabolic bone disorder characterized by reduced mineralization and increase in osteoid thickness. Address for correspondence: This disorder typically occurs in adults, due to different condi- Prof. Giuseppe Martini tions impairing matrix mineralization. Its major symptoms are Dipartimento di Medicina Interna e Malattie Metaboliche diffuse bone pain, muscle weakness and bone fractures with Azienda Ospedaliera Senese minimal trauma. When occurs in children, it is associated with Policlinico “S. Maria alle Scotte” a failure or delay in the mineralization of endochondral new Viale Bracci 7, 53100 Siena, Italy bone formation at the growth plates, causing gait distur- Ph. 0577586452 bances, growth retardation, and skeletal deformities, and it is Fax 0577233446 called rickets. E-mail: [email protected] Histologically patients with osteomalacia present an abun- dance of unmineralized matrix, sometimes to the extent that whole trabeculae appeared to be composed of only osteoid -

Pathological Fracture of the Tibia As a First Sign Of
ANTICANCER RESEARCH 41 : 3083-3089 (2021) doi:10.21873/anticanres.15092 Pathological Fracture of the Tibia as a First Sign of Hyperparathyroidism – A Case Report and Systematic Review of the Current Literature ALEXANDER KEILER 1, DIETMAR DAMMERER 1, MICHAEL LIEBENSTEINER 1, KATJA SCHMITZ 2, PETER KAISER 1 and ALEXANDER WURM 1 1Department of Orthopaedics and Traumatology, Medical University of Innsbruck, Innsbruck, Austria; 2Institute for Pathology, INNPATH GmbH, Innsbruck, Austria Abstract. Background/Aim: Pathological fractures are rare, of the distal clavicles, a “salt and pepper” appearance of the suspicious and in some cases mentioned as the first sign of a skull, bone cysts, and brown tumors of the bones (3). malignant tumor. We present an uncommon case with a Primary hyperparathyroidism (PHPT), also known as “brown pathological fracture of the tibia diaphysis as the first sign of tumor”, also involves unifocal or multifocal bone lesions, which severe hyperparathyroidism. Case Report: We report the case represent a terminal stage of hyperparathyroidism-dependent of a female patient who was referred to the emergency bone pathology (4). This focal lesion is not a real neoplasm. In department with a history of progressively worsening pain in localized regions where bone loss is particularly rapid, the lower left leg and an inability to fully bear weight. No hemorrhage, reparative granulation tissue, and active, vascular, history of trauma or any other injury was reported. An x-ray proliferating fibrous tissue may replace the healthy marrow revealed an extensive osteolytic lesion in the tibial shaft with contents, resulting in a brown tumor. cortical bone destruction. Conclusion: Our case, together with Histologically, the tumor shows bland spindle cell very few cases described in the current literature, emphasizes proliferation with multinucleated osteoclastic giant cells and that in the presence of hypercalcemia and lytic lesions primary signs of bone resorption. -

Musculoskeletal Radiology
MUSCULOSKELETAL RADIOLOGY Developed by The Education Committee of the American Society of Musculoskeletal Radiology 1997-1998 Charles S. Resnik, M.D. (Co-chair) Arthur A. De Smet, M.D. (Co-chair) Felix S. Chew, M.D., Ed.M. Mary Kathol, M.D. Mark Kransdorf, M.D., Lynne S. Steinbach, M.D. INTRODUCTION The following curriculum guide comprises a list of subjects which are important to a thorough understanding of disorders that affect the musculoskeletal system. It does not include every musculoskeletal condition, yet it is comprehensive enough to fulfill three basic requirements: 1.to provide practicing radiologists with the fundamentals needed to be valuable consultants to orthopedic surgeons, rheumatologists, and other referring physicians, 2.to provide radiology residency program directors with a guide to subjects that should be covered in a four year teaching curriculum, and 3.to serve as a “study guide” for diagnostic radiology residents. To that end, much of the material has been divided into “basic” and “advanced” categories. Basic material includes fundamental information that radiology residents should be able to learn, while advanced material includes information that musculoskeletal radiologists might expect to master. It is acknowledged that this division is somewhat arbitrary. It is the authors’ hope that each user of this guide will gain an appreciation for the information that is needed for the successful practice of musculoskeletal radiology. I. Aspects of Basic Science Related to Bone A. Histogenesis of developing bone 1. Intramembranous ossification 2. Endochondral ossification 3. Remodeling B. Bone anatomy 1. Cellular constituents a. Osteoblasts b. Osteoclasts 2. Non cellular constituents a. -

Vanishing Mandible -.:: Journal of Nepal Dental Association
Case Report Vanishing Mandible: Report of a Rare Entity Dr. Bidhata Ojha,1 Dr. Radha Baral,2 Dr. Subrato Bhattacharyya,3 Dr. Dipshikha Bajracharya,4 Dr. Sumit Singh5 1,2,3,4Department of Oral and Maxillofacial Pathology, Kantipur Dental College, Kathmandu, Nepal; 5Department of Oral and Maxillofacial Surgery, Kantipur Dental College, Kathmandu, Nepal Correspondence: Dr. Dipshikha Bajracharya. Email: [email protected] ABSTRACT Vanishing mandible is an important manifestation of Gorham-Stout disease. GSD is a rare osteolytic bone disease of unknown etiology. It is characterised by massive osteolysis and gradual disappearance of bone. It may affect any bone of the body. Herein we report a case of vanished mandible in 16 years male with an emphasis on its differential diagnosis and a brief review of literature. Keywords: Differential diagnosis; Gorham-Stout disease; osteolysis; vanishing mandible. INTRODUCTION He also complaints of discharge of pus from his ear for one month. On extraoral examination there Gorham’s disease is a rare skeletal disorder which was facial asymmetry of lower half of face (Figure is characterised by massive osteolysis where 1A). The swelling was firm on palpation extending the bone is destroyed and does not regenerate two inches below the chin. Intraoral examination or repair and is replaced by fibrous connective 1 revealed mobile lower teeth, erythematous and tissue. It is also known as Phantom bone disease, edematous overlying mucosa with pain on palpation. Vanishing bone disease, Gorham-Stout syndrome, Massive osteolysis, Idiopathic massive osteolysis, Cone beam computed tomography (CBCT) was Progressive osteolysis, Massive Gorham osteolysis, done as a radiological assessment which revealed Morbus Gorham-Stout disease (GSD). -

Musculoskeletal Tumor Information
Tumor Information Bone Tumors Soft Tissue Tumors Bone Tumors Bone tumors are a rare cause of musculoskeletal pain but should always be considered in the patient with otherwise unexplained pain. Most bone tumors present with pain and/or a mass. Care must be taken to ensure the correct diagnosis is made, and early consultation with an orthopaedic oncologist is advised to avoid potential complications. In general, these tumors are best treated at a referral practice that specializes in bone tumors. Benign Presenting symptoms Benign bone tumors can have a wide variety of presenting symptoms; in general, benign bone tumors present with pain. Tumors can occur in any bone, and can occur in all age groups. In general, these tumors are a rare cause of musculoskeletal pain, but should be considered when the diagnosis is in question. Often, benign tumors are found incidentally when patients are imaged for other reasons (i.e., a football player hurts his knee and gets an X- ray to rule out fracture; a suspicious tumor is seen). These are usually benign tumors, but need to be carefully evaluated by an orthopaedic tumor specialist. Diagnostic Imaging Imaging is necessary to diagnose a bone tumor. Often, multiple tests are ordered, but must be evaluated carefully by an orthopaedic tumor specialist to make sure that the most accurate diagnosis is rendered. X-Ray Usually done in the office, this is the most basic imaging test. Plain X- rays can provide essential diagnostic information, and must be of high quality. It is not uncommon to have to repeat these in order to make sure a high quality digital image is obtained. -

Diagnosis of a Maxillary Brown Tumor Associated with Hyperparathyroidism Secondary to Chronic Renal Failure – a Case Report
CASE REPORT Diagnosis of a Maxillary Brown Tumor Associated with Hyperparathyroidism Secondary to Chronic Renal Failure – a Case Report Demetrios Andreadesa/Maria Belazia/Demetrios Antoniadesa Summary: Brown tumor associated with hyperparathyroidism secondary to chronic renal failure has been increasingly documented of late. This intraosseous giant cell lesion is indistinguishable from a central giant cell granuloma and is considered as an unusual local complication of renal osteodystrophy. This report presents a case of a maxillary brown tumor in an uremic, non-hemodialysis patient with secondary hyperparathyroidism. The radiographic, biochemical, and histopathological examinations are reported and the possible pathogenesis is also discussed. Key words: brown tumor, secondary hyperparathyroidism, chronic renal failure Oral Health Prev Dent 2004; 2: 143–147. Submitted for publication: 08.12.03; accepted for publication: 26.02.04. rown tumors represent non-neoplastic, giant Renal osteodystrophy refers to the skeletal B cell lesions that are histopathologically indis- changes resulting from chronic renal disease and tinguishable from giant cell granulomas, and are is caused by disorders in calcium and phosphorus the result of a bone remodeling process during metabolism, abnormal vitamin D metabolism and hyperparathyroidism (HPT). Although these lesions increased parathyroid activity (Cohen, 1994; Mal- are not uncommon in cases of primary hyperpa- luche and Faugere, 1990). rathyroidism (PHPT), there are also some examples The role of parathormone (PTH) is to control cal- associated with HPT and osteitis fibrosa secondary cium and phosphorus levels in plasma and in extra- to renal failure. cellular fluid, and this is potentially achieved by mod- Brown tumors are more commonly seen in hemo- ulating the balance between osteoblastic and os- dialysis patients and can be found in any bones teoclastic activities. -
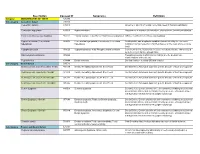
Description Concept ID Synonyms Definition
Description Concept ID Synonyms Definition Category ABNORMALITIES OF TEETH 426390 Subcategory Cementum Defect 399115 Cementum aplasia 346218 Absence or paucity of cellular cementum (seen in hypophosphatasia) Cementum hypoplasia 180000 Hypocementosis Disturbance in structure of cementum, often seen in Juvenile periodontitis Florid cemento-osseous dysplasia 958771 Familial multiple cementoma; Florid osseous dysplasia Diffuse, multifocal cementosseous dysplasia Hypercementosis (Cementation 901056 Cementation hyperplasia; Cementosis; Cementum An idiopathic, non-neoplastic condition characterized by the excessive hyperplasia) hyperplasia buildup of normal cementum (calcified tissue) on the roots of one or more teeth Hypophosphatasia 976620 Hypophosphatasia mild; Phosphoethanol-aminuria Cementum defect; Autosomal recessive hereditary disease characterized by deficiency of alkaline phosphatase Odontohypophosphatasia 976622 Hypophosphatasia in which dental findings are the predominant manifestations of the disease Pulp sclerosis 179199 Dentin sclerosis Dentinal reaction to aging OR mild irritation Subcategory Dentin Defect 515523 Dentinogenesis imperfecta (Shell Teeth) 856459 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield I 977473 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield II 976722 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; -

Brown Tumor of the Facial Bones
1179 Brown Tumor of the Facial Bones Russell Gelman 1 and Fouad E. Gel lad Brown tumors are expansile osteolytic lesions of bone, prominence was palpated in the left maxilla. A 2 x 2 em firm nontender occurring in hyperparathyroidism. They occur more commonly mass was felt in the inferior pole of the thyroid on the right side . in primary hyperparathyroidism, and tend to regress after the Plain radiographs of the face revealed an expansile mass occupy removal of parathyroid adenomas [1]. They are much less ing the majority of the left maxillary antrum causing destruction of common in secondary hyperparathyroidism but have been the lateral maxillary wall. Diffuse osteopenia of the skull and other bones was present. Subperiosteal resorption of the radial side cortex reported [1]. Brown tumors occur most commonly in ribs , of the fingers was present, especially in both index fingers. Early mandible, clavicle, and pelvis, and are uncommon in the facial acroosteolysis was also present. A CT scan revealed an expansile bones [2, 3]. We report two cases, one of primary hyperpar aggressive process arising from the inferior wall of the maxillary athyroidism and one of secondary hyperparathyroidism in antrum with bone and soft-tissue components (Fig . 2). A dynamic CT volving the paranasal sinuses. after a bolus injection of IV contrast medium showed the lesion to be moderately hypervascular. Results of needle and incisional biopsies of the maxillary lesion showed bone marrow fibrosis and multinucle Case Reports ated giant cell infiltration consistent with Brown tumor or reparative giant cell granuloma. Case 1 A right parathyroid adenoma was diagnosed and a partial parathy A 37-year-old woman had a 9-year history of chronic renal failure roidectomy was performed. -

1 Gorham-Stout Disease with Involvement of The
1 Gorham-Stout disease with involvement of the jaws: a systematic review Short title: Gorham-Stout disease of the jaws Bruno Ramos Chrcanovic 1* Ricardo Santiago Gomez 2 1 Department of Prosthodontics, Faculty of Odontology, Malmö University, Malmö, Sweden. [email protected]; [email protected] 2 Department of Oral Surgery and Pathology, School of Dentistry, Universidade Federal de Minas Gerais, Belo Horizonte, Brazil. [email protected] DEPARTMENT OF PROSTHODONTICS, FACULTY OF ODONTOLOGY, MALMÖ UNIVERSITY, MALMÖ, SWEDEN; DEPARTMENT OF ORAL SURGERY AND PATHOLOGY, SCHOOL OF DENTISTRY, UNIVERSIDADE FEDERAL DE MINAS GERAIS, BELO HORIZONTE, BRAZIL * Corresponding author: Bruno Ramos Chrcanovic. Department of Prosthodontics, Faculty of Odontology, Malmö University, Carl Gustafs väg 34, SE-214 21, Malmö, Sweden. [email protected]; [email protected] Mobile: +46 725 541 545 Fax: +46 40 6658503 Funding/grant support: none KEYWORDS Gorham-Stout disease; massive osteolysis; jaw; clinical features; treatment; persistence following treatment 2 ABSTRACT The purpose was to systematically review all published cases of Gorham-Stout disease (GSD) involving the jaws, identify the clinic-radiological and histopathological features associated with the persistence of the lesions, and the best treatment options available. An electronic search was undertaken in November/2018. Eligibility criteria included publications having enough information to confirm the diagnosis. Eighty-six publications reporting 89 cases were included. Features observed: symptomatic (51.1%), swelling (34.1%), pathological fracture (31.8%), history of previous trauma (32.1%), high levels of alkaline phosphatase (24.3%), predominance of vascular tissue (72.4%). Nearly 1/4 of the patients were only followed up and no treatment was implemented. -

A Rare Manifestation of Primary Hyperparathyroidism Vikram Singh Shekhawat, Anil Bhansali
Images in… BMJ Case Reports: first published as 10.1136/bcr-2017-220676 on 1 August 2017. Downloaded from Vanishing metatarsal: a rare manifestation of primary hyperparathyroidism Vikram Singh Shekhawat, Anil Bhansali Department of Endocrinology, DESCRIPTION Post Graduate Institute A 31-year-old woman presented with a history of Medical Education and of bone pains, difficulty in walking and painless Research, Chandigarh, India swelling of the left foot for the last 1 year (figure 1). X-ray of the left foot showed multiple lytic lesions Correspondence to Dr Anil Bhansali, in metatarsal bones and the absence of proximal anilbhansa lien docr ine@ gma il. half of shaft of second metatarsal. Biochemistry com, ashuendo@ gmail. com results revealed corrected serum calcium 11.2 mg/ dL, phosphate 2.0 mg/dL, alkaline phosphatase Accepted 25 July 2017 1049 IU/mL, intact parathyroid hormone (iPTH) 2543 pg/mL, 25-hydroxyvitamin D 16.2 ng/mL, and serum creatinine 0.6 mg/dL. She had no history of pancreatitis or evidence of renal/gall stone disease. The skeletal survey showed multiple osteitis fibrosa cystica (OFC) lesions, pathological Figure 2 (A) X–ray of both foot showing generalised fracture of shaft of the left femur and salt and demineralization of foot bones, multiple lytic lesions pepper appearance of the skull (figure 2a, b, c). (brown tumours) and apparent disappearance of proximal Sestamibi scan revealed right inferior parathyroid half of second metatarsal of the left foot. (B) X–ray of adenoma measuring 3.0×2.9×2.2 cm. Based on pelvis showing ill-defined lucencies in bilateral iliac, pubic the above findings, a diagnosis of primary hyper- and ischial bones, and pathological fracture of left femur.