Atypical Antipsychotics Policy Number: C5016-A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anaesthesia and Past Use Of
177 Correspondence were using LSD. It is more popular than other commonly Anaesthesia and past use of used hallucinogens whose quoted incidence of clients are: LSD ketamine 0.1% (super-K/vitamin K.I), psilocybin and psilocin 0.6% (the active alkaloids in the Mexican "magic To the Editor: mushroom"), and 3,4 methylenedioxymethamphetamine We report the case of a 43-yr-old lady who was admitted ~MDMA" 1% (ecstasy). The effects of the concurrent to the Day Surgery Unit for release of her carpal tunnel ingestion of LSD on anaesthesia are well described. 2-4 retinaculum. During the preoperative visit, she reported The long-term effects of the past use of LSD are largely no intercurrent illnesses, drug therapy or allergies. She unknown. We wonder if the hallucinations experienced did say, however, that she was frightened of general anaes- by our patient during anaesthesia were due to her LSD thesia, since she had experienced terrifying dreams during intake many years before. We would be interested to surgery under general anaesthesia on three occasions dur- know if others have had experience anaesthetising patients ing the previous ten years. On further questioning, she who are past users of phencyclidine-derived drugs. admitted that she had used lysergic acid diethylamide (LSD) during the late 1960's, the last occasion being 1968 Geoffrey N. Morris MRCGPFRCA when she had experienced characterstic hallucinations. Patrick T. Magee MSe FRCA She had not experienced hallucinations in the ensuing Anaesthetic Department years, except on the surgical occasions mentioned. Royal United Hospital One of the three previous operations had been per- Combe Park formed at our hospital and the anaesthetic record was Bath BA1 3NG checked. -

ADHD Parents Medication Guide Revised July 2013
ADHD Parents Medication Guide Revised July 2013 Attention-Deficit/Hyperactivity Disorder Prepared by: American Academy of Child & Adolescent Psychiatry and American Psychiatric Association Supported by the Elaine Schlosser Lewis Fund Physician: ___________________________________________________ Address: ___________________________________________________ ___________________________________________________ ___________________________________________________ Phone: ___________________________________________________ Email: ___________________________________________________ ADHD Parents Medication Guide – July 2013 2 Introduction Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by difficulty paying attention, excessive activity, and impulsivity (acting before you think). ADHD is usually identified when children are in grade school but can be diagnosed at any time from preschool to adulthood. Recent studies indicate that almost 10 percent of children between the ages of 4 to 17 are reported by their parents as being diagnosed with ADHD. So in a classroom of 30 children, two to three children may have ADHD.1,2,3,4,5 Short attention spans and high levels of activity are a normal part of childhood. For children with ADHD, these behaviors are excessive, inappropriate for their age, and interfere with daily functioning at home, school, and with peers. Some children with ADHD only have problems with attention; other children only have issues with hyperactivity and impulsivity; most children with ADHD have problems with all three. As they grow into adolescence and young adulthood, children with ADHD may become less hyperactive yet continue to have significant problems with distraction, disorganization, and poor impulse control. ADHD can interfere with a child’s ability to perform in school, do homework, follow rules, and develop and maintain peer relationships. When children become adolescents, ADHD can increase their risk of dropping out of school or having disciplinary problems. -
Reveiw Week 3 Final with Questions
REVIEW 3 SOMATIZATION AND RELATED DISORDERS SOMATIZATION AND RELATED DISORDERS SOMATIZATION ▸ Psychological problems or concerns that are converted into and communicated as physical distress ▸ Anxiety is either Conscious or Unconscious ▸ Physical Illness is Real SOMATIZATION AND RELATED DISORDERS - SSD SOMATIC SYMPTOM DISORDER A. One or more somatic symptoms that are distressing or result in significant disruption of daily life B. Excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns as manifested by at least one of the following 1. Disproportionate and persistent thoughts about the seriousness or one’s symptoms 2. Persistently high level of anxiety about health or symptoms 3. Excessive time and energy devoted to these symptoms or health concerns C. Although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent (typically more than 6 months) SOMATIZATION AND RELATED DISORDERS - SSD TREATMENT ▸ Regular office visits with the same physician ▸ Psychotherapy ▸ Validate the patient’s feelings/experience of symptoms SOMATIZATION AND RELATED DISORDERS - ILLNESS ANXIETY DISORDER ILLNESS ANXIETY DISORDER A. Formerly hypochondriasis B. Preoccupation with having or acquiring a serious illness C. Somatic symptoms are not present or, if present, are only mild in intensity. If another medical condition is present or there is a high risk for developing a medical condition (strong FH), the preoccupation is clearly excessive or disproportionate D. There is a high level of anxiety about health, and the individual is easily alarmed about personal health status (preoccupation with idea one is sick) E. The individual performs excessive health-related behaviors (checking body) or exhibits maladaptive avoidance (avoids doctors) F. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
Guanfacine Extended Release for ADHD
Out of the Pipeline p Guanfacine extended release for ADHD Floyd R. Sallee, MD, PhD uanfacine extended release (GXR)— Table 1 α Once-daily a selective -2 adrenergic agonist Guanfacine extended release: GFDA-approved for the treatment formulation may of attention-defi cit/hyperactivity disor- Fast facts improve adherence der (ADHD)—has demonstrated effi cacy Brand name: Intuniv and control for inattentive and hyperactive/impulsive Indication: Attention-defi cit/hyperactivity symptoms across disorder symptom domains in 2 large trials lasting® Dowden Health Media a full day 8 and 9 weeks.1,2 GXR’s once-daily formu- Approval date: September 3, 2009 lation may increase adherence and deliver Availability date: November 2009 consistent control of symptomsCopyright across a For personalManufacturer: use Shire only full day (Table 1). Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets Recommended dosage: 0.05 to 0.12 mg/kg Clinical implications once daily GXR exhibits enhancement of noradren- ergic pathways through selective direct receptor action in the prefrontal cortex.3 brain believed to play a major role in at- This mechanism of action is different from tentional and organizational functions that that of other FDA-approved ADHD medi- preclinical research has linked to ADHD.3 cations. GXR can be used alone or in com- The postsynaptic α-2A receptor is bination with stimulants or atomoxetine thought to play a central role in the opti- for treating complex ADHD, such as cases mal functioning of the PFC as illustrated accompanied by oppositional features and by the “inverted U hypothesis of PFC ac- emotional dysregulation or characterized tivation.”4 In this model, cyclic adenos- by partial stimulant response. -

Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the Use of Antiemetics Author(S): Dr Annette Edwards (Chai
Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the use of Antiemetics Author(s): Dr Annette Edwards (Chair) and Deborah Royle on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group Overall objective : To provide guidance on the evidence for the use of antiemetics in specialist palliative care. Search Strategy: Search strategy: Medline, Embase and Cinahl databases were searched using the words nausea, vomit$, emesis, antiemetic and drug name. Review Date: March 2008 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Clinical Guidelines Group. They are intended to be used by qualified, specialist palliative care professionals as an information resource. They should be used in the clinical context of each individual patient’s needs. The clinical guidelines group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact Details: Dr Annette Edwards, Macmillan Consultant in Palliative Medicine, Department of Palliative Medicine, Pinderfields General Hospital, Aberford Road, Wakefield, WF1 4DG Tel: 01924 212290 E-mail: [email protected] 1 Introduction: Nausea and vomiting are common symptoms in patients with advanced cancer. A careful history, examination and appropriate investigations may help to infer the pathophysiological mechanism involved. Where possible and clinically appropriate aetiological factors should be corrected. Antiemetics are chosen based on the likely mechanism and the neurotransmitters involved in the emetic pathway. However, a recent systematic review has highlighted that evidence for the management of nausea and vomiting in advanced cancer is sparse. (Glare 2004) The following drug and non-drug treatments were reviewed to assess the strength of evidence for their use as antiemetics with particular emphasis on their use in the palliative care population. -

Effectiveness of Olanzapine for the Treatment of Breakthrough
Effectiveness of Olanzapine for the Treatment of Breakthrough Chemotherapy Induced Nausea and Vomiting Suthan Chanthawong BPharm*, Suphat Subongkot PharmD*, Aumkhae Sookprasert MD** * Division of Clinical Pharmacy, Faculty of Pharmaceutical Sciences, Khon Kaen University, Khon Kaen, Thailand ** Department of Internal Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand Objective: To evaluate safety and efficacy of olanzapine for breakthrough emesis in addition to standard antiemetic regimen in cancer patients receiving highly emetogenic chemotherapy. Material and Method: A phase II prospective open label clinical trial was conducted in tertiary care based hospital. Forty-six cancer patients diagnosed with solid tumors were enrolled to receive at least one cycle of highly emetogenic chemotherapy (HEC) every two to four weeks. Each patient was provided standard antiemetic consisting of the generic form of ondansetron plus corticosteroids and metoclopramide according to clinical practice guideline. Olanzapine was administered as 5 mg orally every 12 hours for two doses in patients experiencing breakthrough emesis for at least one episode despite standard prevention. The efficacy and tolerability were evaluated every six hours for 24 hours (utilizing Index of Nausea, Vomiting and Retching: INVR tool). Results: Of 46 evaluable patients receiving HEC and additional olanzapine between September 2009 and July 2010, the complete response of breakthrough emesis, retching, and nausea control among patients were 60.9%, 71.7%, and 50.0%, respectively. Adverse events reported were mild and tolerable including dizziness, fatigue, and dyspepsia. Conclusion: Olanzapine is considered to be safe and effective treatment of breakthrough vomiting in cancer patients undergoing highly emetogenic chemotherapy in the present study. Keywords: Olanzapine, Chemotherapy induced nausea and vomiting, Breakthrough vomiting, Ondansetron, Metoclopramide, Dexamethasone J Med Assoc Thai 2014; 97 (3): 349-55 Full text. -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment............................................................... -

The Vomiting Center and the Chemoreceptor Trigger Zone
Pharmacologic Control of Vomiting Todd R. Tams, DVM, Dipl. ACVIM VCA West Los Angeles Animal Hospital Pharmacologic Control of Acute Vomiting Initial nonspecific management of vomiting includes NPO (in minor cases a 6-12 hour period of nothing per os may be all that is required), fluid support, and antiemetics. Initial feeding includes small portions of a low fat, single source protein diet starting 6-12 hours after vomiting has ceased. Drugs used to control vomiting will be discussed here. The most effective antiemetics are those that act at both the vomiting center and the chemoreceptor trigger zone. Vomiting is a protective reflex and when it occurs only occasionally treatment is not generally required. However, patients that continue to vomit should be given antiemetics to help reduce fluid loss, pain and discomfort. For many years I strongly favored chlorpromazine (Thorazine), a phenothiazine drug, as the first choice for pharmacologic control of vomiting in most cases. The HT-3 receptor antagonists ondansetron (Zofran) and dolasetron (Anzemet) have also been highly effective antiemetic drugs for a variety of causes of vomiting. Metoclopramide (Reglan) is a reasonably good central antiemetic drug for dogs but not for cats. Maropitant (Cerenia) is a superior broad spectrum antiemetic drug and is now recognized as an excellent first choice for control of vomiting in dogs. Studies and clinical experience have now also shown maropitant to be an effective and safe antiemetic drug for cats. While it is labeled only for dogs, clinical experience has shown it is safe to use the drug in cats as well. Maropitant is also the first choice for prevention of motion sickness vomiting in both dogs and cats. -
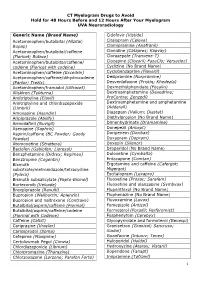
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

PRESCRIBED DRUGS and NEUROLOGICAL COMPLICATIONS K a Grosset, D G Grosset Iii2
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.045757 on 16 August 2004. Downloaded from PRESCRIBED DRUGS AND NEUROLOGICAL COMPLICATIONS K A Grosset, D G Grosset iii2 J Neurol Neurosurg Psychiatry 2004;75(Suppl III):iii2–iii8. doi: 10.1136/jnnp.2004.045757 treatment history is a fundamental part of the healthcare consultation. Current drugs (prescribed, over the counter, herbal remedies, drugs of misuse) and how they are taken A(frequency, timing, missed and extra doses), drugs tried previously and reason for discontinuation, treatment response, adverse effects, allergies, and intolerances should be taken into account. Recent immunisations may also be of importance. This article examines the particular relevance of medication in patients presenting with neurological symptoms. Drugs and their interactions may contribute in part or fully to the neurological syndrome, and treatment response may assist diagnostically or in future management plans. Knowledge of medicine taking behaviour may clarify clinical presentations such as analgesic overuse causing chronic daily headache, or severe dyskinesia resulting from obsessive use of dopamine replacement treatment. In most cases, iatrogenic symptoms are best managed by withdrawal of the offending drug. Indirect mechanisms whereby drugs could cause neurological problems are beyond the scope of the current article—for example, drugs which raise blood pressure or which worsen glycaemic control and consequently increase the risk of cerebrovascular disease, or immunosupressants