Relative Afferent Pupillary Defect
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pupillary Disorders LAURA J
13 Pupillary Disorders LAURA J. BALCER Pupillary disorders usually fall into one of three major cat- cortex generally do not affect pupillary size or reactivity. egories: (1) abnormally shaped pupils, (2) abnormal pupillary Efferent parasympathetic fibers, arising from the Edinger– reaction to light, or (3) unequally sized pupils (anisocoria). Westphal nucleus, exit the midbrain within the third nerve Occasionally pupillary abnormalities are isolated findings, (efferent arc). Within the subarachnoid portion of the third but in many cases they are manifestations of more serious nerve, pupillary fibers tend to run on the external surface, intracranial pathology. making them more vulnerable to compression or infiltration The pupillary examination is discussed in detail in and less susceptible to vascular insult. Within the anterior Chapter 2. Pupillary neuroanatomy and physiology are cavernous sinus, the third nerve divides into two portions. reviewed here, and then the various pupillary disorders, The pupillary fibers follow the inferior division into the orbit, grouped roughly into one of the three listed categories, are where they then synapse at the ciliary ganglion, which lies discussed. in the posterior part of the orbit between the optic nerve and lateral rectus muscle (Fig. 13.3). The ciliary ganglion issues postganglionic cholinergic short ciliary nerves, which Neuroanatomy and Physiology initially travel to the globe with the nerve to the inferior oblique muscle, then between the sclera and choroid, to The major functions of the pupil are to vary the quantity of innervate the ciliary body and iris sphincter muscle. Fibers light reaching the retina, to minimize the spherical aberra- to the ciliary body outnumber those to the iris sphincter tions of the peripheral cornea and lens, and to increase the muscle by 30 : 1. -

Taking the Mystery out of Abnormal Pupils
Taking the mystery out of abnormal pupils No financial disclosures Course Title: Taking the mystery out [email protected] of abnormal pupils Lecturer: Brad Sutton, OD, FAAO Clinical Professor IU School of Optometry . •Review of Anatomy Iris anatomy Iris sphincter Iris dilator Parasympathetic pathway Sympathetic pathway Parasympathetic Pathway Parasympathetic Pathway Light stimulates the retina then impulse Four neuron arc travels with the ganglion cells through the Retina to the pretectal nucleus in the chiasm into the optic tracts. 80% go to the midbrain (1) LGN , 20% to the pretectal nuclei.They Pretectal nucleus to the EW nucleus (2) then hemidecussate and terminate at the EW nucleus EW nucleus to the ciliary ganglion (3) Ciliary ganglion to the iris sphincter with short ciliary nerves (4) 1 Points of Interest Sympathetic Pathway Within the second order neuron there are Three neuron arc 30 near response fibers for every light Posterior hypothalamus to ciliospinal response fiber. This allows for light - near center of Budge ( C8 - T2 ). (1) dissociation. Center of Budge to the superior cervical The third order neuron runs with cranial ganglion in the neck (2) nerve III from the brain stem to the ciliary Superior cervical ganglion to the dilator ganglion. Superficially located prior to the muscle (3) cavernous sinus. Points of Interest Second order neuron runs along the surface of the lung, can be affected by a Pancoast tumor Third order neuron runs with the carotid artery then with the ophthalmic division of cranial nerve V 2 APD Testing testing……………….AKA……… … APD / reverse APD Direct and consensual response Which is the abnormal pupil ? Very simple rule. -
Complete and Incomplete Forms of the Benign Disorder Characterised By
Br J Ophthalmol: first published as 10.1136/bjo.16.8.449 on 1 August 1932. Downloaded from THE BRITISH JOURNAL OF OPHTHALMOLOGY AUGUST, 1932 COMMUNICATIONS COMPLETE AND INCOMPLETE FORMS OF THE BENIGN DISORDER CHARACTERISED BY TONIC PUPILS AND ABSENT copyright. TENDON REFLEXES BY W. J. ADIE, M.D., F.R.C.P. PHYSICIAN, CHARING CROSS HOSPITAL AND ROYAL LONDON OPHTHALMIC HOSPITAL. OUT-PATIENT PHYSICIAN, THE NATIONAL HOSPITAL FOR NERVOUS DISEASES, QUEEN SQUARE http://bjo.bmj.com/ IN earlier papers on this subject it has been suggested that certain apparently dissimilar abnormal pupillary reactions formerly described as occurring in unrelated conditions are manifestations of the same disorder. The abnormal reactions are, on the one hand, the tonic pupillary reaction (syn. pupillotonia, myotonic reaction, tonic convergence reaction of pupils apparently inactive to light, on September 30, 2021 by guest. Protected Marcus's peculiar pupil phenomenon, non-luetic Argyll Robertson pupil, pseudo-Argyll Robertson pupil) and, on the other hand what may be called atypical phases of the tonic pupil. In the atypical phases tonic reactions are absent or difficult to detect and the state of the pupil in cases that present them is usually desig- nated by the term fixed pupil, ophthalmoplegia interna, iridoplegia or partial iridoplegia, of unknown origin. The disorder referred to, if the views expressed here are correct, may manifest itself in the following clinical forms: A. The complete form characterized by the presence in one or both eyes of the tonic convergence reaction in a pupil apparently Br J Ophthalmol: first published as 10.1136/bjo.16.8.449 on 1 August 1932. -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

9781441967237.Pdf
The Neurologic Diagnosis wwwwwwwwww Jack N. Alpert The Neurologic Diagnosis A Practical Bedside Approach Jack N. Alpert, MD St. Luke’s Episcopal Hospital Department of Neurology University of Texas Medical School at Houston Houston, TX, USA [email protected] ISBN 978-1-4419-6723-7 e-ISBN 978-1-4419-6724-4 DOI 10.1007/978-1-4419-6724-4 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011941214 © Springer Science+Business Media, LLC 2012 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) In Memory of Morris B. -

Pupil and Accomodation Abnormalities
PPUUPPIILL AANNDD AACCCCOOMMOODDAATTIIOONN AABBNNOORRMMAALLIITTIIEESS SympatheticSympathetic pathwaypathway ofof pupillarypupillary innervationinnervation PPuuppiillllaarryy lliigghhtt rreefflleexxeess ••PupilPupil diameterdiameter isis subjectsubject toto continuouscontinuous variationsvariations asas aa functionfunction ofof changeschanges inin luminanceluminance,, fixationfixation andand psychosensitivepsychosensitive stimulistimuli.. •• PupilsPupils mustmust bebe studiedstudied byby evaluatingevaluating theirtheir sizesize,, shapeshape,, symmetrysymmetry andand activityactivity ((dilationdilation andand constrictionconstriction).). •• ToTo evaluateevaluate sizesize andand symmetrysymmetry ofof pupilspupils,, patientspatients areare invitedinvited toto fixatefixate aa farawayfaraway objectobject,, whichwhich mustmust notnot bebe aa sourcesource ofof excessiveexcessive lightlight stimulationstimulation.. ••SSuubbsseeqquueennttllyy,, bbyy iilllluummiinnaattiinngg tthhee ppaattiieennttss’’ ffaaccee ffrroomm bbeellooww wwiitthh aa wweeaakk lliigghhtt ssoouurrccee,, bbootthh ppuuppiillss aarree ssiimmuullttaanneeoouussllyy oobbsseerrvveedd aanndd tthheeiirr ddiiaammeetteerrss aarree ddeetteerrmmiinneedd ((mmmm)).. •• IInn tthhee nnoorrmmaall ppooppuullaattiioonn,, ppuuppiill ddiiaammeetteerr tteennddss ttoo bbee ssmmaalllleerr iinn cchhiillddrreenn,, iinn tthhee eellddeerrllyy aanndd iinn ssuubbjjeeccttss wwiitthh ddaarrkk iirriiss.. •In general, anisocoria which changes with changes of luminance conditions must be considered pathologic, -

Keratoglobus BS Wallang and S Das
Eye (2013) 27, 1004–1012 & 2013 Macmillan Publishers Limited All rights reserved 0950-222X/13 www.nature.com/eye REVIEW Keratoglobus BS Wallang and S Das Abstract Keratoglobus is a rare noninflammatory The exact cause remains largely unknown corneal thinning disorder characterised by although various theories have been proposed generalised thinning and globular protrusion based on its similarities with other more of the cornea. It was first described as a common noninflammatory ectasia such as separate clinical entity by Verrey in 1947. Both keratoconus. In fact, these similarities have congenital and acquired forms have been brought about confusion as to whether the shown to occur, and may be associated with disorders comprising this group are separate various other ocular and systemic syndromes clinical disorders, or rather a spectrum of the including the connective tissue disorders. same disease process. Similarities have been found with other noninflammatory thinning disorders like keratoconus that has given rise to hypotheses Aetiological factors about the aetiopathogenesis. However, the exact Keratoglobus is primarily considered a genetics and pathogenesis are still unclear. congenital disorder present since birth.3–5 Clinical presentation is characterised by pro- However, in more recent years, there have been gressive diminution resulting from irregular reports of acquired forms of keratoglobus. corneal topography with increased corneal The congenital form of the disorder is always fragility due to extreme thinning. Conservative bilateral. The exact genetics of the disorder have and surgical management for visual rehabilita- not been studied in detail and no definite tion and improved tectonic stability have been inheritance pattern has been described. It is described, but remains challenging. -

Discoverer of the Pupillary Syndrome
Br J Vener Dis: first published as 10.1136/sti.53.4.244 on 1 August 1977. Downloaded from British Journal of Venereal Disease, 1977, 53, 244-246 Douglas Argyll Robertson, 1837-1909 Discoverer of the pupillary syndrome A. LENNOX THORBURN From H.M. Prison, Styal, Cheshire Douglas Moray Cooper Lamb Argyll Robertson was born in Edinburgh and went to school at the -N sf,p Edinburgh Institution. He had a strong surgical background. His father and two uncles were Fellows of the Royal College of Surgeons of Edinburgh and his father, John Argyll Robertson, had been President; with others, he had established the Edinburgh Eye Dispensary. Douglas Argyll Robertson graduated MD in 1857 from the University of St Andrews after a four-year course, and in the same year, took the Licence of the Royal College of Surgeons of Edinburgh. After a year at the Edinburgh Royal Infirmary, he decided copyright. to specialise in ophthalmic surgery. In those days this choice was a departure from the normal practice of concentrating on general surgery while under- taking several forms of specialist surgery. It could also be financially hazardous, and this narrow avenue in surgery was not popular with many of the profession; Britain in this respect lagged behind European medicine and surgery. Argyll Robertson travelled to Berlin and Prague to meet ophthalmic Douglas Argyll Robertson http://sti.bmj.com/ surgeons, and to study and work under them. There were many excellent physicians and surgeons on the Chirurgical Society of Edinburgh and appeared in continent in the latter half of the last century, the Edinburgh Medical Journal (Argyll Robertson, attracting brilliant young men; foremost in ocular 1863a) and the Boston Medical Journal (Argyll surgery were Von Graefe and Von Arfelt. -

Eye Health 115 27
CURRICULUM, STATUTES & REGULATIONS FOR MS OPHTHALMOLOGY RAWALPINDI MEDICAL UNIVERSITY I PREFACE The horizons of Medical Education are widening & there has been a steady rise of global interest in Post Graduate Medical Education, an increased awareness of the necessity for experience in education skills for all healthcare professionals and the need for some formal recognition of postgraduate training in Ophthalmology. We are seeing a rise in the uptake of places on postgraduate courses in medical education, more frequent issues of medical education journals and the further development of e-journals and other new online resources. There is therefore a need to provide active support in Post Graduate Medical Education for a larger, national group of colleagues in all specialties and at all stages of their personal professional development. If we were to formulate a statement of intent to explain the purpose of this log book, we might simply say that our aim is to help clinical colleagues to teach and to help students to learn in a better and advanced way. This book is a state of the art log book with representation of all activities of the MS Ophthalmology program at RMU.A summary of the curriculum is incorporated in the logbook for convenience of supervisors and residents. MS curriculum is based on six Core Competencies of ACGME (Accreditation Council for Graduate Medical Education) including Patient Care, Medical Knowledge, System Based Practice, Practice Based Learning, Professionalism, Interpersonal and Communication Skills. A perfect monitoring system of a training program including monitoring of teaching and learning strategies, assessment and Research Activities cannot be denied so we at RMU have incorporated evaluation by Quality Assurance Cell and its comments in the logbook in addition to evaluation by University Training Monitoring Cell (URTMC). -

Differential Diagnoses
Differential diagnoses RETINA • CNVM Degenerative ARMD myopic degeneration angioid streaks choroidal hemangioma juxtafoveal retinal telangiectasia osteogenesis imperfecta optic nerve head pit retinochoroidal coloboma tilted optic disc Heredodegenerative Vitelliform macular dystrophy Fundus flavimaculatus Optic nerve head drusen choroideremia RP with exudate Inflammatory Ocular histoplasmosis syndrome Multifocal choroiditis (white dot syndromes) Serpiginous choroiditis Toxoplasmosis Toxocariasis Rubella Vogt-Koyanagi-Harada syndrome Behcet syndrome Sympathetic ophthalmia Central serous retinopathy sarcoid syphilis chronic uveitis AMPEE Neoplastic Choroidal nevus Choroidal hemangioma Metastatic choroidal tumors Hamartoma of the RPE choroidal osteoma malignant melanoma optic nerve glioma with chronically swollen nerve Traumatic Choroidal rupture Intense photocoagulation IOFB retinal cryoinjury surgical trauma subretinal fluid drainage site Idiopathic • CME post-op Irvine-Gass syndrome corneal surgery retinal surgery laser iridotomy cryo for retinal tear PRP aphakia pseudophakia inherited / dystrophies RP autosomal dominant CME juvenile retinoschisis Goldmann-Favre disease medications Xalatan topical epinephrine nicotinic acid tumors differentials 1 choroidal melanoma / nevi choroidal hemangioma retinal capillary hemangioma tractional ERM vitreomacular traction syndrome inflammatory Eale's CMV pars planitis Behcet Birdshot sarcoidosis idiopathic vitritis scleritis toxo vascular DR CRVO BRVO OIS retinal juxtafoveal telangiectasia CNVM Coat's -
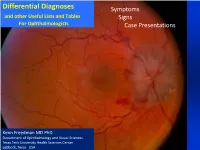
Differential Diagnoses Symptoms and Other Useful Lists and Tables Signs for Ophthalmologists Case Presentations
Differential Diagnoses Symptoms and other Useful Lists and Tables Signs For Ophthalmologists Case Presentations Kenn Freedman MD PhD Department of Ophthalmology and Visual Sciences Texas Tech University Health Sciences Center Lubbock, Texas USA Acknowledgments and Disclaimer The differential diagnoses and lists contained herein are not meant to be exhaustive, but are to give in most cases the most common causes of many ocular / visual symptoms, signs and situations. Included also in these lists are also some less common, but serious conditions that must be “ruled-out”. These lists have been based on years of experience, and I am grateful for God’s help in developing them. I also owe gratitude to several sources* including Roy’s classic text on Ocular Differential Diagnosis. * Please see references at end of document This presentation, of course, will continue to be a work in progress and any concerns or suggestions as to errors or omissions or picture copyrights will be considered. Please feel free to contact me at [email protected] Kenn Freedman Lubbock, Texas - October 2018 Disclaimer: The diagnostic algorithm for the diagnosis and management of Ocular or Neurological Conditions contained in this presentation is not intended to replace the independent medical or professional judgment of the physician or other health care providers in the context of individual clinical circumstances to determine a patient’s care. Use of this Presentation The lists are divided into three main areas 1. Symptoms 2. Signs from the Eight Point Eye Exam 3. Common Situations and Case Presentations The index for all of the lists is given on the following 3 pages. -

“Prostitute's Pupil” Through Argyll Robertson
Rev Bras Neurol. 55(1):38-41, 2019 HISTORICAL NOTE FROM THE “SMALL DOLL” UNTIL “PROSTITUTE’S PUPIL” THROUGH ARGYLL ROBERTSON: THE ARGYLL ROBERTSON´S SIGN, ONE HUNDRED FIFTY YEARS FROM HIS FINDINGS (1869) DA “PEQUENA BONECA” ATÉ “PUPILA DA PROSTITUTA” ATRAVÉS DE ARGYLL ROBERTSON: O SINAL DE ARGYLL ROBERTSON, CENTO E CINQUENTA ANOS DE SEUS ACHADOS (1869) M. da Mota Gomes1 ABSTRACT RESUMO A tiny structure, the pupil, attracts too much attention, since the an- Uma estrutura minúscula, a pupila, atrai muita atenção, desde a anti- tiquity. The pupil as part of the “‘window of/to the soul”, the eyes, it guidade. A pupila como parte da “'janela da alma'”, os olhos, poderia can demonstrate a clinical disorder sign, or simply a psychological demonstrar um sinal de desordem clínica, ou, simplesmente, uma expression. In this paper, it is studied the situation in which the pu- expressão psicológica. Neste trabalho, estuda-se a situação em que o pillary reflex to light is compromised, but the accommodation reflex reflexo pupilar à luz é comprometido, mas o reflexo de acomodação is preserved, what is named after Argyll Robertson, the first Scottish é preservado, o que leva o nome de Argyll Robertson, o primeiro of- ophthalmologist, who besides described the signal (1869), he also talmologista escocês que além de descrever o sinal (1869), também tried to defined its clinical significance. Afterwards, it was clearly -de tentou definiu seu significado clínico. Posteriormente, foi claramente monstrated its relationship with tertiary neurosyphilis. demonstrada sua relação com a neurossífilis terciária. Key words: Pupil, reflex, miosis, Argyll Robertson, autonomous nerve Palavras-chave: Pupila, reflexo, Argyll Robertson, sistema nervoso system, neurology, ophthalmology autônomo, neurologia, oftalmologia 1Associate Professor, Institute of Neurology, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil Endereço para correspondência: Marleide da Mota Gomes; Universidade Federal do Rio de Janeiro, Instituto de Neurologia Deolindo Couto; Av.