Clinical Features and Management of Snakebite Envenoming in French Guiana
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phylogenetic Diversity, Habitat Loss and Conservation in South
Diversity and Distributions, (Diversity Distrib.) (2014) 20, 1108–1119 BIODIVERSITY Phylogenetic diversity, habitat loss and RESEARCH conservation in South American pitvipers (Crotalinae: Bothrops and Bothrocophias) Jessica Fenker1, Leonardo G. Tedeschi1, Robert Alexander Pyron2 and Cristiano de C. Nogueira1*,† 1Departamento de Zoologia, Universidade de ABSTRACT Brasılia, 70910-9004 Brasılia, Distrito Aim To analyze impacts of habitat loss on evolutionary diversity and to test Federal, Brazil, 2Department of Biological widely used biodiversity metrics as surrogates for phylogenetic diversity, we Sciences, The George Washington University, 2023 G. St. NW, Washington, DC 20052, study spatial and taxonomic patterns of phylogenetic diversity in a wide-rang- USA ing endemic Neotropical snake lineage. Location South America and the Antilles. Methods We updated distribution maps for 41 taxa, using species distribution A Journal of Conservation Biogeography models and a revised presence-records database. We estimated evolutionary dis- tinctiveness (ED) for each taxon using recent molecular and morphological phylogenies and weighted these values with two measures of extinction risk: percentages of habitat loss and IUCN threat status. We mapped phylogenetic diversity and richness levels and compared phylogenetic distances in pitviper subsets selected via endemism, richness, threat, habitat loss, biome type and the presence in biodiversity hotspots to values obtained in randomized assemblages. Results Evolutionary distinctiveness differed according to the phylogeny used, and conservation assessment ranks varied according to the chosen proxy of extinction risk. Two of the three main areas of high phylogenetic diversity were coincident with areas of high species richness. A third area was identified only by one phylogeny and was not a richness hotspot. Faunal assemblages identified by level of endemism, habitat loss, biome type or the presence in biodiversity hotspots captured phylogenetic diversity levels no better than random assem- blages. -

De Los Reptiles Del Yasuní
guía dinámica de los reptiles del yasuní omar torres coordinador editorial Lista de especies Número de especies: 113 Amphisbaenia Amphisbaenidae Amphisbaena bassleri, Culebras ciegas Squamata: Serpentes Boidae Boa constrictor, Boas matacaballo Corallus hortulanus, Boas de los jardines Epicrates cenchria, Boas arcoiris Eunectes murinus, Anacondas Colubridae: Dipsadinae Atractus major, Culebras tierreras cafés Atractus collaris, Culebras tierreras de collares Atractus elaps, Falsas corales tierreras Atractus occipitoalbus, Culebras tierreras grises Atractus snethlageae, Culebras tierreras Clelia clelia, Chontas Dipsas catesbyi, Culebras caracoleras de Catesby Dipsas indica, Culebras caracoleras neotropicales Drepanoides anomalus, Culebras hoz Erythrolamprus reginae, Culebras terrestres reales Erythrolamprus typhlus, Culebras terrestres ciegas Erythrolamprus guentheri, Falsas corales de nuca rosa Helicops angulatus, Culebras de agua anguladas Helicops pastazae, Culebras de agua de Pastaza Helicops leopardinus, Culebras de agua leopardo Helicops petersi, Culebras de agua de Peters Hydrops triangularis, Culebras de agua triángulo Hydrops martii, Culebras de agua amazónicas Imantodes lentiferus, Cordoncillos del Amazonas Imantodes cenchoa, Cordoncillos comunes Leptodeira annulata, Serpientes ojos de gato anilladas Oxyrhopus petolarius, Falsas corales amazónicas Oxyrhopus melanogenys, Falsas corales oscuras Oxyrhopus vanidicus, Falsas corales Philodryas argentea, Serpientes liana verdes de banda plateada Philodryas viridissima, Serpientes corredoras -

Distribution and Natural History of the Ecuadorian Toad-Headed Pitvipers of the Genus Bothrocophias (Squamata: Serpentes: Viperidae: Crotalinae)
©Österreichische Gesellschaft für Herpetologie e.V., Wien, Austria, download unter www.biologiezentrum.at HERPETOZOA 19 (1/2): 17-26 17 Wien, 30. Juli 2006 Distribution and natural history of the Ecuadorian Toad-headed Pitvipers of the genus Bothrocophias (Squamata: Serpentes: Viperidae: Crotalinae) Verbreitung und Naturgeschichte der ecuadorianischen Krötenkopf-Grubenottern der Gattung Bothrocophias (Squamata: Serpentes: Viperidae: Crotalinae) DIEGO F. CISNEROS-HEREDIA & MARIA OLGA BORJA & DANIEL PROANO & JEAN-MARC TOUZET KURZFASSUNG Spärlich sind die Kenntnisse über Grubenottern der Gattung Bothrocophias. Die vorliegende Arbeit enthält Informationen zu drei Bothrocophias Arten aus Ecuador: Bothrocophias campbelli (FREIRE LASCANO, 1991), B. hyoprora (AMARAL, 1935) und B. microphthalmus (COPE, 1875), einschließlich Angaben zur geographischen und vertikalen Verbreitung, zu Nachweisen in den Provinzen, sympatrischen Grubenotternarten, Aktivitätsmustern, Verhalten, Körpergröße, Fortpflanzungsbiologie, Nahrung und Lebensalter. Bothrocophias campbelli bewohnt die nördlichen, zentralen und südlichen Gebiete der pazifischen Andenabhänge Ecuadors zwischen 800 und 2000 m; Bothrocophias hyoprora kommt im nördlichen und südlichen Amazonastiefland und an den unteren östlichen Hän- gen der Anden Ecuadors zwischen 210 und 1500 m vor, Bothrocophias microphthalmus an deren Südosthängen zwischen 600 und 2350 m. Die Arbeit berichtet über den zweiten Fundortnachweis von B. campbelli in der Provinz Imbabura und den westlichsten Fundort von B. hyoprora im Tal des Nangaritza Flusses. Das ympatrische Vorkom- men von B. hyoprora und B. microphthalmus im Makuma-Gebiet, Provinz Morona-Santiago, wird bestätigt, was die bisher bekannte obere Verbreitungsgrenze von B. microphthalmus auf zumindest 600 m anhebt. Das Weiß- bauch-Mausopossum Marmosops noctivagus wird erstmals als Beutetier von B. microphthalmus beschrieben. Die neuen Daten über die Fortpflanzungsbiologie von Grubenottern der Gattung Bothrocophias umfassen Wurfgröße und Körperlänge Neugeborener bei B. -

J Venom Anim Toxins Incl Trop Dis, 2020, 26:E20190103 Page 2 of 14
RESEARCH OPEN ACCESS ISSN 1678-9199 www.jvat.org Venomics and antivenomics of the poorly studied Brazil’s lancehead, Bothrops brazili (Hoge, 1954), from the Brazilian State of Pará Libia Sanz1, Alicia Pérez1, Sarai Quesada-Bernat1, Rafaela Diniz-Sousa2,3,4, Leonardo A. Calderón2,3,5,6, 2,3,4,5,7 1,* 2,3,5 Andreimar M. Soares , Juan J. Calvete , Cleópatra A.S. Caldeira 1 Evolutionary and Translational Venomics Laboratory, Spanish National Research Council (CSIC), Valencia, Spain. 2 Center for the Study of Biomolecules Applied to Health (CEBio), Oswaldo Cruz Foundation Rondônia, Porto Velho, RO, Brazil. 3 Graduate Program in Experimental Biology (PGBIOEXP), Federal University of Rondônia (UNIR), Porto Velho, RO, Brazil. 4 São Lucas University Center (UniSL), Porto Velho, RO, Brazil. 5 Graduate Program in Biodiversity and Biotechnology, BIONORTE Network, Porto Velho, RO, Brazil. 6 Aparício Carvalho University Center (FIMCA), Porto Velho, RO, Brazil. 7 National Institute of Science and Technology in Epidemiology of the Western Amazônia, (INCT-EpiAmO), Porto Velho, RO, Brazil. Keywords: Abstract Snake venom Background: The Brazil’s lancehead, Bothrops brazili, is a poorly studied pit viper Bothrops brazili distributed in lowlands of the equatorial rainforests of southern Colombia, northeastern Venomics Peru, eastern Ecuador, southern and southeastern Venezuela, Guyana, Suriname, Third-generation French Guiana, Brazil, and northern Bolivia. Few studies have been reported on toxins antivenomics isolated from venom of Ecuadorian and Brazilian B. brazili. The aim of the present study was to elucidate the qualitative and quantitative protein composition of B. brazili Brazilian antibothropic venom from Pará (Brazil), and to carry out a comparative antivenomics assessment polyvalent antivenom of the immunoreactivity of the Brazilian antibothropic pentavalent antivenom [soro antibotrópico (SAB) in Portuguese] against the venoms of B. -

First Report of an Accident with the Speckled Forest Pit Viper (Bothriopsis Taeniata) in Brazil
RELATO DE CASO/CASE REPOT Revista da Sociedade Brasileira de Medicina Tropical 42(3):342-344, mai-jun, 2009 First report of an accident with the speckled forest pit viper (Bothriopsis taeniata) in Brazil Primeiro registro de acidente pela jararaca estrela (Bothriopsis taeniata) no Brasil Pasesa Q. Torrez¹, Marcelo R. Duarte³, Francisco O.S. França¹,², Ligia Figueiredo¹, Paulo Abati¹, Luciana R. Campos¹, Pedro Pereira de Oliveira Pardal4, Mariana Quiroga¹, Melissa Mascheretti¹ and Marcos Boulos¹ RESUMO Relatamos o primeiro caso de acidente por Bothriopsis taeniata no Brasil. A vítima, trabalhador rural com 43 anos de idade, foi picada pouco acima do calcanhar direito, apresentando quadro clínico compatível por envenenamento botrópico leve: discreto edema com hemorragia no local da picada e dor, embora com ausência de coagulopatia. Palavras-chaves: Bothriopsis taeniata. Acidente botrópico. Amazônia. ABSTRACT The first reported case of an accident withBothriopsis taeniata in Brazil is described. The victim, a 43-year-old man, was bitten just above his right heel and presented a clinical condition compatible with mild Bothrops poisoning: local edema with hemorrhage at the bite site and pain, although without coagulopathy. Key-words: Bothriopsis taeniata. Bothrops accident. Amazon region. Viperidae snake poisoning is considered a public health CASE REPORT problem in many regions, especially in subtropical and tropical countries4 11 16, causing both morbidity and mortality. 25,364 In November 2007, a 43-year-old man was bitten just above snakebites were notified in Brazil in 2008, with a mortality rate of his right ankle by a snake, while working on a rural site. He did 100 deaths/year9. -

The Envira Amazonia Project a Tropical Forest Conservation Project in Acre, Brazil
The Envira Amazonia Project A Tropical Forest Conservation Project in Acre, Brazil Prepared by Brian McFarland from: 853 Main Street East Aurora, New York - 14052 (240) 247-0630 With significant contributions from: James Eaton, TerraCarbon JR Agropecuária e Empreendimentos EIRELI Pedro Freitas, Carbon Securities Ayri Rando, Independent Community Specialist A Climate, Community and Biodiversity Standard Project Implementation Report TABLE OF CONTENTS COVER PAGE .................................................................................................................... Page 4 INTRODUCTION …………………………………………………………..……………. Page 5 GENERAL SECTION G1. Project Goals, Design and Long-Term Viability …………………………….………. Page 6 A. Project Overview 1. Project Proponents 2. Project’s Climate, Community and Biodiversity Objectives 3. Project Location and Parameters B. Project Design and Boundaries 4. Project Area and Project Zone 5. Stakeholder Identification and Analysis 6. Communities, Community Groups and Other Stakeholders 7. Map Identifying Locations of Communities and Project 8. Project Activities, Outputs, Outcomes and Impacts 9. Project Start Date, Lifetime and GHG Accounting Period C. Risk Management and Long-Term Viability 10. Natural and Human-Induced Risks 11. Enhance Benefits Beyond Project Lifetime 12. Financial Mechanisms Adopted G2. Without-Project Land Use Scenario and Additionality ………………..…………….. Page 52 1. Most Likely Land-Use Scenario 2. Additionality of Project Benefits G3. Stakeholder Engagement ……………………………………………………………. Page 57 A. Access to Information 1. Accessibility of Full Project Documentation 2. Information on Costs, Risks and Benefits 3. Community Explanation of Validation and Verification Process B. Consultation 4. Community Influence on Project Design 5. Consultations Directly with Communities C. Participation in Decision-Making and Implementation 6. Measures to Enable Effective Participation D. Anti-Discrimination 7. Measures to Ensure No Discrimination E. Feedback and Grievance Redress Procedure 8. -

Reptiles of Ecuador: a Resource-Rich Online Portal, with Dynamic
Offcial journal website: Amphibian & Reptile Conservation amphibian-reptile-conservation.org 13(1) [General Section]: 209–229 (e178). Reptiles of Ecuador: a resource-rich online portal, with dynamic checklists and photographic guides 1Omar Torres-Carvajal, 2Gustavo Pazmiño-Otamendi, and 3David Salazar-Valenzuela 1,2Museo de Zoología, Escuela de Ciencias Biológicas, Pontifcia Universidad Católica del Ecuador, Avenida 12 de Octubre y Roca, Apartado 17- 01-2184, Quito, ECUADOR 3Centro de Investigación de la Biodiversidad y Cambio Climático (BioCamb) e Ingeniería en Biodiversidad y Recursos Genéticos, Facultad de Ciencias de Medio Ambiente, Universidad Tecnológica Indoamérica, Machala y Sabanilla EC170301, Quito, ECUADOR Abstract.—With 477 species of non-avian reptiles within an area of 283,561 km2, Ecuador has the highest density of reptile species richness among megadiverse countries in the world. This richness is represented by 35 species of turtles, fve crocodilians, and 437 squamates including three amphisbaenians, 197 lizards, and 237 snakes. Of these, 45 species are endemic to the Galápagos Islands and 111 are mainland endemics. The high rate of species descriptions during recent decades, along with frequent taxonomic changes, has prevented printed checklists and books from maintaining a reasonably updated record of the species of reptiles from Ecuador. Here we present Reptiles del Ecuador (http://bioweb.bio/faunaweb/reptiliaweb), a free, resource-rich online portal with updated information on Ecuadorian reptiles. This interactive portal includes encyclopedic information on all species, multimedia presentations, distribution maps, habitat suitability models, and dynamic PDF guides. We also include an updated checklist with information on distribution, endemism, and conservation status, as well as a photographic guide to the reptiles from Ecuador. -

2016-2018 Envira Amazonia Project Monitoring Report
MONITORING REPORT: CCB Version 3, VCS Version 3 2016-2018 ENVIRA AMAZONIA PROJECT MONITORING REPORT Document Prepared By CarbonCo, LLC,1 East Aurora, NY - USA and Ostrya Conservation, Inc.2, Scottsville, VA - USA The Envira Amazonia Project – A Tropical Forest Conservation Project Title Project in Acre, Brazil Project ID 1382 Version 5.0 Report ID 1.0 Date of Issue 2-December-2019 Project Location Acre, Brazil Brian McFarland, CarbonCo, LLC 853 Main Street, East Aurora, New York - 14052 Phone: (240) 247-0630 Email: [email protected] Website: www.CarbonCoLLC.com JR Agropecuária e Empreendimentos EIRELI José Elves Araruna de Sousa Project Proponent(s) Travessa Alagoas, Number 49, Altos, Bairro Centro Rio Branco, Acre, Brazil, CEP (Zip Code) 69900-412 Phone: +55 (68) 9 8402 8151 Email: [email protected] Freitas International Group, Doing Business as Carbon Securities Pedro Freitas 201 S. Biscayne Boulevard, 28th Floor, Miami, Florida, 33131, USA Phone: (305) 209-0909 Email: [email protected] Prepared By Brian McFarland1 and James Eaton2 CCB v3.0, VCS v3.4 1 MONITORING REPORT: CCB Version 3, VCS Version 3 SCS Global Services Letty B. Brown, Ph.D. Validation/Verification Body Email: [email protected] Phone: +1 (510) 452-8000 2000 Powell Street, Suite 600 Emeryville, California, 94608, USA The Project Start Date is August 2, 2012 with a 10 year GHG Accounting Period and the Project Lifetime is 30 years. The initial GHG Accounting/ Crediting baseline period started on August 2, 2012 and is set to continue Period through August 1, 2022. The Project Lifetime is: 2 August 2012 – 1 August 2042; 30-year total period. -

A New Species of Pitviper of the Genus Bothrops (Serpentes: Viperidae: Crotalinae) from the Central Andes of South America
Zootaxa 4656 (1): 099–120 ISSN 1175-5326 (print edition) https://www.mapress.com/j/zt/ Article ZOOTAXA Copyright © 2019 Magnolia Press ISSN 1175-5334 (online edition) https://doi.org/10.11646/zootaxa.4656.1.4 http://zoobank.org/urn:lsid:zoobank.org:pub:62FC927B-8DEC-4649-933A-F5FE7C0D5E83 A new species of pitviper of the genus Bothrops (Serpentes: Viperidae: Crotalinae) from the Central Andes of South America JUAN TIMMS1, JUAN C. CHAPARRO2,3, PABLO J. VENEGAS4, DAVID SALAZAR-VALENZUELA5, GUSTAVO SCROCCHI6, JAIRO CUEVAS7, GERARDO LEYNAUD8,9 & PAOLA A. CARRASCO8,9,10 1Asociación Herpetológica Española, Museo Nacional de Ciencias Naturales. José Gutiérrez Abascal 2, 28006 Madrid, España. 2Museo de Biodiversidad del Perú, Urbanización Mariscal Gamarra A-61, Zona 2, Cusco, Perú. 3Museo de Historia Natural de la Universidad Nacional de San Antonio Abad del Cusco, Paraninfo Universitario (Plaza de Armas s/n), Cusco, Perú. 4División de Herpetología, Centro de Ornitología y Biodiversidad (CORBIDI), Santa Rita 10536, Of. 202, Huertos de San Antonio, Surco, Lima, Perú. 5Centro de Investigación de la Biodiversidad y Cambio Climático (BioCamb) e Ingeniería en Biodiversidad y Recursos Genéticos, Facultad de Ciencias de Medio Ambiente, Universidad Tecnológica Indoamérica, Machala y Sabanilla, Quito, Ecuador EC170301. 6UEL-CONICET and Fundación Miguel Lillo, Miguel Lillo 251, San Miguel de Tucumán, Tucumán, Argentina. 7Universidad Complutense de Madrid, Av. Séneca, 2, 28040 Madrid, España. 8Universidad Nacional de Córdoba, Facultad de Ciencias Exactas, Físicas y Naturales, Centro de Zoología Aplicada, Rondeau 798, Córdoba 5000, Argentina. 9Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), Instituto de Diversidad y Ecología Animal (IDEA), Rondeau 798, Córdoba 5000, Argentina. -

Brazilian Reptiles: List of Species
BRAZILIAN REPTILES: LIST OF SPECIES Concluded on September 30, 2012 ORGANIZED BY Renato Silveira Bérnils ([email protected]) and Henrique Caldeira Costa ([email protected]) The present List must be cited as: Bérnils, R. S. and H. C. Costa (org.). 2012. Brazilian reptiles: List of species. Version 2012.1. Available at http://www.sbherpetologia.org.br/. Sociedade Brasileira de Herpetologia. Downloaded on... [date of your download] ENDEMIC TOTAL OF TOTAL OF TAXA OF BRAZIL SPECIES TAXA* REPTILES no 738 784 TESTUDINES BATSCH, 1788 no 36 36 CRYPTODIRA COPE, 1868 no 11 11 Chelonioidea Baur, 1893 no 5 5 Cheloniidae Oppel, 1811 no 4 4 1 Caretta caretta (Linnaeus, 1758) no 2 Chelonia mydas (Linnaeus, 1758) no 3 Eretmochelys imbricata (Linnaeus, 1766) no 4 Lepidochelys olivacea (Eschscholtz, 1829) no Dermochelyidae Fitzinger, 1843 no 1 1 5 Dermochelys coriacea (Linnaeus, 1766) no Kinosternoidea Joyce, Parham & Gauthier, 2004 no 1 1 Kinosternidae Agassiz, 1857 no 1 1 Kinosterninae Agassiz, 1857 no 1 1 6 Kinosternon scorpioides scorpioides (Linnaeus, 1766) no Testudinoidea Fitzinger, 1826 no 5 5 Emydidae Rafinesque, 1815 no 2 2 Deirochelyinae Agassiz, 1857 no 2 2 7 Trachemys adiutrix Vanzolini, 1995 1 yes 8 Trachemys dorbigni (Duméril & Bibron, 1835) 1 no Geoemydidae Theobald, 1868 no 1 1 9 Rhinoclemmys punctularia punctularia (Daudin, 1801) no Testudinidae Batsch, 1788 no 2 2 10 Chelonoidis carbonaria (Spix, 1824) no 11 Chelonoidis denticulata (Linnaeus, 1766) no 1 ENDEMIC TOTAL OF TOTAL OF TAXA OF BRAZIL SPECIES TAXA* PLEURODIRA COPE, 1864 -

Notes on the Conservation Status, Geographic Distribution and Ecology of Bothrops Muriciensis Ferrarezzi & Freire, 2001 (Serpentes, Viperidae)
NORTH-WESTERN JOURNAL OF ZOOLOGY 8 (2): 338-343 ©NwjZ, Oradea, Romania, 2012 Article No.: 121133 http://biozoojournals.3x.ro/nwjz/index.html Notes on the conservation status, geographic distribution and ecology of Bothrops muriciensis Ferrarezzi & Freire, 2001 (Serpentes, Viperidae) Marco Antonio de FREITAS1,*, Daniella Pereira Fagundes de FRANÇA2, Roberta GRABOSKI3, Vivian UHLIG4 and Diogo VERÍSSIMO5,* 1. Instituto Chico Mendes de Conservação da Biodiversidade (ICMBio) Rua do Maria da Anunciação n 208 Eldorado, CEP 69932-000. Eldorado, Brasiléia, Acre, Brazil. 2. Universidade Federal do Acre – UFAC, Campus Universitário. BR 364, km 04, Distrito Industrial, CEP 69915-900. Rio Branco, AC, Brazil. 3. Pontifica Universidade Católica do Rio Grande do Sul - PUCRS. Avenida Ipiranga, 6681, Paternon, CEP: 90619-900. Porto Alegre, Rio Grande do Sul, Brazil. 4. Centro Nacional de Pesquisa e Conservação de Répteis e Anfíbios – RAN/ICMBio, Rua 229, nº 95, Setor Leste Universitário, CEP: 74.605.090, Goiânia, Goiás, Brazil. 5. Durrell Institute of Conservation and Ecology, University of Kent, CT2 7NR, Canterbury, Kent, UK. * Corresponding authors, D. Veríssimo, E-mail: [email protected]; M.A. de Freitas, E-mail: [email protected] Received: 27. October 2011 / Accepted: 11. September 2012 / Available online: 21. October 2012 / Printed: December 2012 Abstract. The Atlantic forest of Brazil is one of the most biodiverse regions in the world. However, in the last centuries this biome has suffered unparalled fragmentation and degradation of its forest cover, with only 8% of its original area remaining. The region of Murici, in the state of Alagoas, Brazil, houses some of the largest forest fragments of Atlentic forest and is of one of the regions within the biome with more threatened and endemic taxa. -
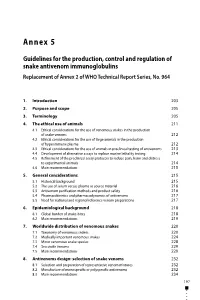
Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No
Annex 5 Guidelines for the production, control and regulation of snake antivenom immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No. 964 1. Introduction 203 2. Purpose and scope 205 3. Terminology 205 4. The ethical use of animals 211 4.1 Ethical considerations for the use of venomous snakes in the production of snake venoms 212 4.2 Ethical considerations for the use of large animals in the production of hyperimmune plasma 212 4.3 Ethical considerations for the use of animals in preclinical testing of antivenoms 213 4.4 Development of alternative assays to replace murine lethality testing 214 4.5 Refinement of the preclinical assay protocols to reduce pain, harm and distress to experimental animals 214 4.6 Main recommendations 215 5. General considerations 215 5.1 Historical background 215 5.2 The use of serum versus plasma as source material 216 5.3 Antivenom purification methods and product safety 216 5.4 Pharmacokinetics and pharmacodynamics of antivenoms 217 5.5 Need for national and regional reference venom preparations 217 6. Epidemiological background 218 6.1 Global burden of snake-bites 218 6.2 Main recommendations 219 7. Worldwide distribution of venomous snakes 220 7.1 Taxonomy of venomous snakes 220 7.2 Medically important venomous snakes 224 7.3 Minor venomous snake species 228 7.4 Sea snake venoms 229 7.5 Main recommendations 229 8. Antivenoms design: selection of snake venoms 232 8.1 Selection and preparation of representative venom mixtures 232 8.2 Manufacture of monospecific or polyspecific antivenoms 232 8.3 Main recommendations 234 197 WHO Expert Committee on Biological Standardization Sixty-seventh report 9.