T Lymphocytes and Testicular Immunity: a New Insight Into Immune Regulation in Testes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Longitudinal Study of Leukocyte DNA Methylation and Biomarkers for Cancer Risk in Older Adults
bioRxiv preprint doi: https://doi.org/10.1101/597666; this version posted April 3, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Longitudinal Study of Leukocyte DNA Methylation and 2 Biomarkers for Cancer Risk in Older Adults 3 Alexandra H. Bartlett1, Jane W Liang1, Jose Vladimir Sandoval-Sierra1, Jay H 4 Fowke 1, Eleanor M Simonsick2, Karen C Johnson1, Khyobeni Mozhui1* 5 1Department of Preventive Medicine, University of Tennessee Health Science 6 Center, Memphis, Tennessee, USA 7 2Intramural Research Program, National Institute on Aging, Baltimore Maryland, 8 USA 9 AHB: [email protected]; JWL: [email protected]; JVSS: 10 [email protected]; JHF: [email protected]; EMS: [email protected]; 11 KCJ: [email protected]; KM: [email protected] 12 *Corresponding author: Khyobeni Mozhui 13 14 15 16 17 18 1 bioRxiv preprint doi: https://doi.org/10.1101/597666; this version posted April 3, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 19 Abstract 20 Background: Changes in DNA methylation over the course of life may provide 21 an indicator of risk for cancer. We explored longitudinal changes in CpG 22 methylation from blood leukocytes, and likelihood of a future cancer diagnosis. -

Longitudinal Study of Leukocyte DNA Methylation and Biomarkers for Cancer Risk in Older Adults Alexandra H
Bartlett et al. Biomarker Research (2019) 7:10 https://doi.org/10.1186/s40364-019-0161-3 RESEARCH Open Access Longitudinal study of leukocyte DNA methylation and biomarkers for cancer risk in older adults Alexandra H. Bartlett1, Jane W. Liang1, Jose Vladimir Sandoval-Sierra1, Jay H. Fowke1, Eleanor M. Simonsick2, Karen C. Johnson1 and Khyobeni Mozhui1* Abstract Background: Changes in DNA methylation over the course of life may provide an indicator of risk for cancer. We explored longitudinal changes in CpG methylation from blood leukocytes, and likelihood of future cancer diagnosis. Methods: Peripheral blood samples were obtained at baseline and at follow-up visit from 20 participants in the Health, Aging and Body Composition prospective cohort study. Genome-wide CpG methylation was assayed using the Illumina Infinium Human MethylationEPIC (HM850K) microarray. Results: Global patterns in DNA methylation from CpG-based analyses showed extensive changes in cell composition over time in participants who developed cancer. By visit year 6, the proportion of CD8+ T-cells decreased (p-value = 0. 02), while granulocytes cell levels increased (p-value = 0.04) among participants diagnosed with cancer compared to those who remained cancer-free (cancer-free vs. cancer-present: 0.03 ± 0.02 vs. 0.003 ± 0.005 for CD8+ T-cells; 0.52 ± 0. 14 vs. 0.66 ± 0.09 for granulocytes). Epigenome-wide analysis identified three CpGs with suggestive p-values ≤10− 5 for differential methylation between cancer-free and cancer-present groups, including a CpG located in MTA3, agene linked with metastasis. At a lenient statistical threshold (p-value ≤3×10− 5), the top 10 cancer-associated CpGs included a site near RPTOR that is involved in the mTOR pathway, and the candidate tumor suppressor genes REC8, KCNQ1,andZSWIM5. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Pinto Mariaetelvina D.Pdf
i ii iii Dedico À minha família Meu porto seguro... iv Agradecimentos À professora Dra. Rejane Maira Góes, pela sua orientação, ética e confiança. Obrigada por ter contribuído imensamente para o meu amadurecimento profissional e pessoal. Ao professor Dr. Sebastião Roberto Taboga pela sua atenção e auxílio durante a realização deste trabalho. Aos professores: Dr. Luis Antonio Violin Dias Pereira, Dra. Maria Tercilia Vilela de Azeredo Oliveira e Dra. Mary Anne Heidi Dolder pelo cuidado e atenção na análise prévia da tese e pelas valiosas sugestões. Aos professores: Dra. Maria Tercília Vilela de Azeredo Oliveira, Dr. Marcelo Emílio Beletti, Dra. Cristina Pontes Vicente e Dra. Wilma De Grava kempinas pela atenção dispensada e sugestões para o aprimoramento deste trabalho. Ao Programa de Pós-graduação em Biologia Celular e Estrutural e a todos os docentes que dele participa, principalmente àqueles que batalham para que esse curso seja reconhecido como um dos melhores do país. v A secretária Líliam Alves Senne Panagio, pela presteza, eficiência e auxílio concedido durantes esses anos de UNICAMP, principalmente nos momentos de mais correria. À Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – CAPES, pelo imprescindível suporte financeiro. Ao Instituto de Biociências, Letras e Ciências Exatas de São José do Rio Preto, IBILCE-UNESP, por ter disponibilizado espaço físico para a realização da parte experimental deste trabalho. Ao técnico Luiz Roberto Falleiros Júnior do Laboratório de Microscopia e Microanálise, IBILCE-UNESP, pela assistência técnica e amizade. Aos amigos do Laboratório de Microscopia e Microanálise, IBILCE- UNESP: Fernanda Alcântara, Lara Corradi, Sérgio de Oliveira, Bianca Gonçalves, Ana Paula Perez, Manoel Biancardi, Marina Gobbo, Cíntia Puga, Fanny Arcolino, Flávia Cabral e Samanta Maeda, e todos que por ali passaram durante todos esses anos. -

A Clinical Case of Fournier's Gangrene: Imaging Ultrasound
J Ultrasound (2014) 17:303–306 DOI 10.1007/s40477-014-0106-5 CASE REPORT A clinical case of Fournier’s gangrene: imaging ultrasound Marco Di Serafino • Chiara Gullotto • Chiara Gregorini • Claudia Nocentini Received: 24 February 2014 / Accepted: 17 March 2014 / Published online: 1 July 2014 Ó Societa` Italiana di Ultrasonologia in Medicina e Biologia (SIUMB) 2014 Abstract Fournier’s gangrene is a rapidly progressing Introduction necrotizing fasciitis involving the perineal, perianal, or genital regions and constitutes a true surgical emergency Fournier’s gangrene is an acute, rapidly progressive, and with a potentially high mortality rate. Although the diagnosis potentially fatal, infective necrotizing fasciitis affecting the of Fournier’s gangrene is often made clinically, emergency external genitalia, perineal or perianal regions, which ultrasonography and computed tomography lead to an early commonly affects men, but can also occur in women and diagnosis with accurate assessment of disease extent. The children [1]. Although originally thought to be an idio- Authors report their experience in ultrasound diagnosis of pathic process, Fournier’s gangrene has been shown to one case of Fournier’s gangrene of testis illustrating the main have a predilection for patients with state diabetes mellitus sonographic signs and imaging diagnostic protocol. as well as long-term alcohol misuse. However, it can also affect patients with non-obvious immune compromise. Keywords Fournier’s gangrene Á Sonography Comorbid systemic disorders are being identified more and more in patients with Fournier’s gangrene. Diabetes mel- Riassunto La gangrena di Fournier e` una fascite necro- litus is reported to be present in 20–70 % of patients with tizzante a rapida progressione che coinvolge il perineo, le Fournier’s Gangrene [2] and chronic alcoholism in regioni perianale e genitali e costituisce una vera emer- 25–50 % patients [3]. -

Male Reproductive System
MALE REPRODUCTIVE SYSTEM DR RAJARSHI ASH M.B.B.S.(CAL); D.O.(EYE) ; M.D.-PGT(2ND YEAR) DEPARTMENT OF PHYSIOLOGY CALCUTTA NATIONAL MEDICAL COLLEGE PARTS OF MALE REPRODUCTIVE SYSTEM A. Gonads – Two ovoid testes present in scrotal sac, out side the abdominal cavity B. Accessory sex organs - epididymis, vas deferens, seminal vesicles, ejaculatory ducts, prostate gland and bulbo-urethral glands C. External genitalia – penis and scrotum ANATOMY OF MALE INTERNAL GENITALIA AND ACCESSORY SEX ORGANS SEMINIFEROUS TUBULE Two principal cell types in seminiferous tubule Sertoli cell Germ cell INTERACTION BETWEEN SERTOLI CELLS AND SPERM BLOOD- TESTIS BARRIER • Blood – testis barrier protects germ cells in seminiferous tubules from harmful elements in blood. • The blood- testis barrier prevents entry of antigenic substances from the developing germ cells into circulation. • High local concentration of androgen, inositol, glutamic acid, aspartic acid can be maintained in the lumen of seminiferous tubule without difficulty. • Blood- testis barrier maintains higher osmolality of luminal content of seminiferous tubules. FUNCTIONS OF SERTOLI CELLS 1.Germ cell development 2.Phagocytosis 3.Nourishment and growth of spermatids 4.Formation of tubular fluid 5.Support spermiation 6.FSH and testosterone sensitivity 7.Endocrine functions of sertoli cells i)Inhibin ii)Activin iii)Follistatin iv)MIS v)Estrogen 8.Sertoli cell secretes ‘Androgen binding protein’(ABP) and H-Y antigen. 9.Sertoli cell contributes formation of blood testis barrier. LEYDIG CELL • Leydig cells are present near the capillaries in the interstitial space between seminiferous tubules. • They are rich in mitochondria & endoplasmic reticulum. • Leydig cells secrete testosterone,DHEA & Androstenedione. • The activity of leydig cell is different in different phases of life. -
Urologic Disorders
Urologic Disorders Abdulaziz Althunayan Consultant Urologist Assistant professor of Surgery Urologic Disorders Urinary tract infections Urolithiasis Benign Prostatic Hyperplasia and voiding dysfunction Urinary tract infections Urethritis Acute Pyelonephritis Epididymitis/orchitis Chronic Pyelonephritis Prostatitis Renal Abscess cystitis URETHRITIS S&S – urethral discharge – burning on urination – Asymptomatic Gonococcal vs. Nongonococcal DX: – incubation period(3-10 days vs. 1-5 wks) – Urethral swab – Serum: Chlamydia-specific ribosomal RNA URETHRITIS Epididymitis Acute : pain, swelling, of the epididymis <6wk chronic :long-standing pain in the epididymis and testicle, usu. no swelling. DX – Epididymitis vs. Torsion – U/S – Testicular scan – Younger : N. gonorrhoeae or C. trachomatis – Older : E. coli Epididymitis Prostatitis Syndrome that presents with inflammation± infection of the prostate gland including: – Dysuria, frequency – dysfunctional voiding – Perineal pain – Painful ejaculation Prostatitis Prostatitis Acute Bacterial Prostatitis : – Rare – Acute pain – Storage and voiding urinary symptoms – Fever, chills, malaise, N/V – Perineal and suprapubic pain – Tender swollen hot prostate. – Rx : Abx and urinary drainage cystitis S&S: – dysuria, frequency, urgency, voiding of small urine volumes, – Suprapubic /lower abdominal pain – ± Hematuria – DX: dip-stick urinalysis Urine culture Pyelonephritis Inflammation of the kidney and renal pelvis S&S : – Chills – Fever – Costovertebral angle tenderness (flank Pain) – GI:abdo pain, N/V, and -

Non-Certified Epididymitis DST.Pdf
Clinical Prevention Services Provincial STI Services 655 West 12th Avenue Vancouver, BC V5Z 4R4 Tel : 604.707.5600 Fax: 604.707.5604 www.bccdc.ca BCCDC Non-certified Practice Decision Support Tool Epididymitis EPIDIDYMITIS Testicular torsion is a surgical emergency and requires immediate consultation. It can mimic epididymitis and must be considered in all people presenting with sudden onset, severe testicular pain. Males less than 20 years are more likely to be diagnosed with testicular torsion, but it can occur at any age. Viability of the testis can be compromised as soon as 6-12 hours after the onset of sudden and severe testicular pain. SCOPE RNs must consult with or refer all suspect cases of epididymitis to a physician (MD) or nurse practitioner (NP) for clinical evaluation and a client-specific order for empiric treatment. ETIOLOGY Epididymitis is inflammation of the epididymis, with bacterial and non-bacterial causes: Bacterial: Chlamydia trachomatis (CT) Neisseria gonorrhoeae (GC) coliforms (e.g., E.coli) Non-bacterial: urologic conditions trauma (e.g., surgery) autoimmune conditions, mumps and cancer (not as common) EPIDEMIOLOGY Risk Factors STI-related: condomless insertive anal sex recent CT/GC infection or UTI BCCDC Clinical Prevention Services Reproductive Health Decision Support Tool – Non-certified Practice 1 Epididymitis 2020 BCCDC Non-certified Practice Decision Support Tool Epididymitis Other considerations: recent urinary tract instrumentation or surgery obstructive anatomic abnormalities (e.g., benign prostatic -

Contribution of Enhancer-Driven and Master-Regulator Genes to Autoimmune Disease Revealed Using Functionally Informed SNP-To-Gene Linking Strategies Kushal K
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.02.279059; this version posted March 31, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Contribution of enhancer-driven and master-regulator genes to autoimmune disease revealed using functionally informed SNP-to-gene linking strategies Kushal K. Dey1, Steven Gazal1, Bryce van de Geijn 1,3, Samuel Sungil Kim 1,4, Joseph Nasser5, Jesse M. Engreitz5, Alkes L. Price 1,2,5 1 Department of Epidemiology, Harvard T. H. Chan School of Public Health, Boston, MA, USA 2 Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, MA 3 Genentech, South San Francisco, CA 4 Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA 5 Broad Institute of MIT and Harvard, Cambridge, MA, USA Abstract Gene regulation is known to play a fundamental role in human disease, but mechanisms of regulation vary greatly across genes. Here, we explore the con- tributions to disease of two types of genes: genes whose regulation is driven by enhancer regions as opposed to promoter regions (Enhancer-driven) and genes that regulate many other genes in trans (Master-regulator). We link these genes to SNPs using a comprehensive set of SNP-to-gene (S2G) strategies and apply stratified LD score regression to the resulting SNP annotations to draw three main conclusions about 11 autoimmune diseases and blood cell traits (average Ncase=13K across 6 autoimmune diseases, average N=443K across 5 blood cell traits). -

LEYDIG CELLS AS a MODEL of MALE REPRODUCTIVE SYSTEM Tomáš Jambor*1, Eva Tvrdá1, Jana Lukáčová1, Norbert Lukáč1
LEYDIG CELLS AS A MODEL OF MALE REPRODUCTIVE SYSTEM Tomáš Jambor*1, Eva Tvrdá1, Jana Lukáčová1, Norbert Lukáč1 Address(es): Ing. Tomáš Jambor, 1Slovak University of Agriculture, Faculty of Biotechnology and Food Sciences, Department of Animal Physiology, Trieda A. Hlinku 2, 949 76 Nitra, Slovak Republic, phone number: +421-37-6414288. *Corresponding author: [email protected] ARTICLE INFO ABSTRACT Received 25. 10. 2013 During the past decades, a large anount of information concerning the infertility, which can be caused by malfunction at the level of Revised 20. 11. 2013 sperm or production of testosterone was published. It is about androgene which is from 95 percent synthetized in testes. It plays Accepted 16. 12. 2013 significant role in development of individual´s sexual signs and is also the starter of spermatogenesis. The main mechanism ensuring the Published 1. 2. 2014 production of this important hormone is the process determined as a steroidogenesis. This process runs in cells located in testes and are known as Leydig cells (LC). Several types of LC are classified as for example fetal, adult, stem, progenitor or immature cells. There are mutual differences, but their common feature is a production of androgenes. Mitochondria and endoplasmic reticulum have irreplaceable Review position within LC and they, together with relevant enzymes and cascades of reactions, ensure the metamorphosis of cholesterol up to testosterone. With rising age the activity of steroidogenesis declines what is, however, natural. But there are many cases when this process in cells of developing individual is impaired by external or internal factors. Their identification and consequent elimination is for sufficient production of testosterone very important. -

Leydig Cell Differentation, Steroid Metabolism by the Interstitium in Vitro and the Growth of the Accessory Sex Organs in the Rat
LEYDIG CELL DIFFERENTATION, STEROID METABOLISM BY THE INTERSTITIUM IN VITRO AND THE GROWTH OF THE ACCESSORY SEX ORGANS IN THE RAT W. N. TSANG, D. LACY and P. M. COLLINS Department of Zoology, St Bartholomew's Medical College, Charterhouse Square, London, E.C.1 (Received 14th December 1972) Several workers have studied various parameters as an index of Leydig cell differentiation and attempted to correlate them with the growth of the accessory sex organs. In the prepuberal rat, little correlation seems to have been achieved (see Niemi & Ikonen, 1963; Clegg, 1966). Others have examined testosterone production in vitro by the immature testis and attempted to correlate this with the increase in weight of the seminal vesicles and prostate gland. In this connec- tion, a good deal of attention has been paid to the production of testosterone in vitro and its apparent regulation by 5\g=a\-reductaseactivity. Nayfeh, Barefoot & Baggett (1966) reported an increase in testosterone production per unit weight of tissue at about the time of sexual maturity and suggested that this might be due mainly to reduced metabolism to 5\g=a\-androstane-3\g=a\, 17\g=b\-diol (androstanediol). Inano, Hori & Tamaoki (1967) found a remarkable increase in the activity of various enzymes associated with testosterone formation from Days 20 to 30 and a marked decline in the yields per testis of androsterone and 3\g=a\,17\g=a\-dihydroxy-5\g=a\-pregnan-20-one from Days 40 to 60. The same authors also found a dramatic increase in the weight of the seminal vesicles from Days 50 to 60. -
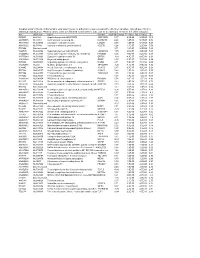
Supplementary File 2A Revised
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06