Clinical Practice Guideline for Bronchiolitis Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Allergic Bronchopulmonary Aspergillosis Revealing Asthma
CASE REPORT published: 22 June 2021 doi: 10.3389/fimmu.2021.695954 Case Report: Allergic Bronchopulmonary Aspergillosis Revealing Asthma Houda Snen 1,2*, Aicha Kallel 2,3*, Hana Blibech 1,2, Sana Jemel 2,3, Nozha Ben Salah 1,2, Sonia Marouen 3, Nadia Mehiri 1,2, Slah Belhaj 3, Bechir Louzir 1,2 and Kalthoum Kallel 2,3 1 Pulmonary Department, Hospital Mongi Slim, La Marsa, Tunisia, 2 Faculty of Medicine, Tunis El Manar University, Tunis, Tunisia, 3 Parasitology and Mycology Department, La Rabta Hospital, Tunis, Tunisia Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder caused by hypersensitivity to Aspergillus which colonizes the airways of patients with asthma and cystic fibrosis. Its diagnosis could be difficult in some cases due to atypical Edited by: presentations especially when there is no medical history of asthma. Treatment of ABPA is Brian Stephen Eley, frequently associated to side effects but cumulated drug toxicity due to different molecules University of Cape Town, South Africa is rarely reported. An accurate choice among the different available molecules and Reviewed by: effective on ABPA is crucial. We report a case of ABPA in a woman without a known Shivank Singh, Southern Medical University, China history of asthma. She presented an acute bronchitis with wheezing dyspnea leading to an Richard B. Moss, acute respiratory failure. She was hospitalized in the intensive care unit. The Stanford University, United States bronchoscopy revealed a complete obstruction of the left primary bronchus by a sticky *Correspondence: Houda Snen greenish material. The culture of this material isolated Aspergillus fumigatus and that of [email protected] bronchial aspiration fluid isolated Pseudomonas aeruginosa. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Rhinitis and Sinusitis
Glendale Animal Hospital 623-934-7243 www.familyvet.com Rhinitis and Sinusitis (Inflammation of the Nose and Sinuses) Basics OVERVIEW Rhinitis—inflammation of the lining of the nose Sinusitis—inflammation of the sinuses The nasal cavity communicates directly with the sinuses; thus inflammation of the nose (rhinitis) and inflammation of the sinuses (sinusitis) often occur together (known as “rhinosinusitis”) “Upper respiratory tract” (also known as the “upper airways”) includes the nose, nasal passages, throat (pharynx), and windpipe (trachea) “Lower respiratory tract” (also known as the “lower airways”) includes the bronchi, bronchioles, and alveoli (the terminal portion of the airways, in which oxygen and carbon dioxide are exchanged) SIGNALMENT/DESCRIPTION OF PET Species Dogs Cats Breed Predilections Short-nosed, flat-faced (known as “brachycephalic”) cats are more prone to long-term (chronic) inflammation of the nose (rhinitis), and possibly fungal rhinitis Dogs with a long head and nose (known as “dolichocephalic dogs,” such as the collie and Afghan hound) are more prone to Aspergillus (a type of fungus) infection and nasal tumors Mean Age and Range Cats—sudden (acute) viral inflammation of the nose and sinuses (rhinosinusitis) and red masses in the nasal cavity and throat (known as “nasopharyngeal polyps”) are more common in young kittens (6–12 weeks of age) Congenital (present at birth) diseases (such as cleft palate) are more common in young pets Tumors/cancer and dental disease—are more common in older pets Foreign -
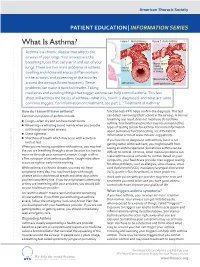
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Other Work-Related Respiratory Disease Statistics in Great Britain, 2020 Allergic Alveolitis, Byssinosis and Allergic Rhinitis
Health and Safety Executive Data up to December 2019 Annual Statistics Published 4th November 2019 Other work-related respiratory disease statistics in Great Britain, 2020 Allergic alveolitis, byssinosis and allergic rhinitis Contents Other respiratory diseases 2 Farmer's lung and other allergic alveolitis 2 Byssinosis 3 Allergic rhinitis 3 The document can be found at: www.hse.gov.uk/statistics/causdis/ This document is available from www.hse.gov.uk/statistics/ Page 1 of 4 Other respiratory diseases This document outlines the available statistics for occupational respiratory diseases other than asbestos- related disease, asthma, Chronic Obstructive Pulmonary Disease (COPD) and pneumoconiosis which are covered elsewhere – see https://www.hse.gov.uk/statistics/causdis/index.htm. Farmer's lung and other allergic alveolitis Occupational Extrinsic Allergic Alveolitis (EAA) – also known as Occupational Hypersensitivity Pneumonitis – is inflammation of the alveoli within the lungs caused by an allergic reaction to inhaled material. “Farmer's lung”, which is caused by the inhalation of dust or spores arising from mouldy hay, grain or straw, is a common form of the disease. It is typically characterised by acute flu-like effects but can, in some cases, also lead to serious longer-term effects on lung function. There has been an average of 7 new cases of occupational EAA assessed for Industrial Injuries Disablement Benefit (IIDB) each year over the last decade, with about 15% of total cases being among women (Table IIDB01 www.hse.gov.uk/statistics/tables/iidb01.xlsx). There has also been an average of 7 deaths where farmer's lung (or a similar condition) was recorded as the underlying cause each year over the last decade (Table DC01 www.hse.gov.uk/statistics/tables/dc01.xlsx), with less than 10% of total deaths among women. -

Allergic/Non-Allergic Rhinitis
Tips to Remember: Rhinitis Do you have a runny or stuffy nose that doesn't seem to go away? If so, you may have rhinitis, which is an inflammation of the mucous membranes of the nose. Rhinitis is one of the most common allergic conditions in the United States, affecting about 40 million people. It often coexists with other allergic disorders, such as asthma. It is important to treat rhinitis because it can contribute to other conditions such as sleep disorders, fatigue and learning problems. There are two general types of rhinitis: Allergic rhinitis is caused by substances called allergens. Allergens are often common, usually harmless substances that can cause an allergic reaction in some people. Causes • When allergic rhinitis is caused by common outdoor allergens, such as airborne tree, grass and weed pollens or mold, it is called seasonal allergic rhinitis, or "hay fever." • Allergic rhinitis is also triggered by common indoor allergens, such as animal dander (dried skin flakes and saliva), indoor mold or droppings from cockroaches or dust mites. This is called perennial allergic rhinitis. Symptoms • Sneezing • Congestion • Runny nose • Itchiness in the nose, roof of the mouth, throat, eyes and ears Diagnosis If you have symptoms of allergic rhinitis, an allergist/immunologist can help determine which specific allergens are triggering your reaction. He or she will take a thorough health history, and then test you to determine if you have allergies. Skin tests or Blood (RAST) tests are the most common methods for determining your allergic triggers. Treatment Once your allergic triggers are determined, your physician or nurse will work with you to develop a plan to avoid the allergens that trigger your symptoms. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

Respiratory Problems – Occupational and Environmental Exposures
The respiratory tract Respiratory problems Occupational and environmental exposures Ryan F Hoy Background Case study The respiratory tract comes into contact with approximately A man, 23 years of age and previously well, presents with 14 000 litres of air during a standard working week. The 2 months of cough, shortness of breath and weight loss. quality of the air we breathe has major implications for our He reports intermittent fevers and flu-like symptoms over respiratory health. Any part of the respiratory tract, from the the same period. During a recent 2 week holiday to Bali nose to the alveoli, may be adversely affected by exposure to he felt significantly better, but after returning home he airborne contaminants. has had a recurrence of symptoms. Objective Occupational and exposure history identifies him as This article outlines some common occupational and commencing work at a mushroom farm 12 months environmental exposures that can lead to respiratory problems. ago where he is exposed to dust from the mixing of mushroom compost. He is not required to use respiratory Discussion protection at work. His cough and chest tightness Some of the effects of exposures may be immediate, whereas usually start in the afternoon at work and persist into others such as asbestos-related lung disease may not present the evening. Other workers at the mushroom farm have for many decades. Airborne contaminants may be the primary reported similar symptoms and have had to leave the cause of respiratory disease or can exacerbate pre-existing workplace as a result. respiratory conditions such as asthma and chronic obstructive pulmonary disease. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS. -

Interstitial Lung Disease
Interstitial Lung Disease Nitin Bhatt, MD Assistant Professor of Internal Medicine Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine Ohio State University Medical Center Interstitial Lung Disease Jim Allen, MD Professor of Internal Medicine Division of Pulmonary & Critical Care Medicine Ohio State University Medical Center 1 Case #1 Case #1 • 57 y.o. WM with a history of shortness of breath and cough that has been present for 1 year • Initially worse with walking, moderate exertion. No resting symptoms. • Now activity limiting • Associated with a dry, nonproductive cough • Negative cardiac evaluation • PMHx: HTN • Meds: HCTZ • SOCHx: 30 pack year smoking history, quit 10 years ago 2 Case #1 • PE: HR 78, BP 138/67, sats 96% on room air • Lungs with bibasilar dry crackles • Ext with clubbing • PFTs: • FVC 69% predicted • FEV1 72% • TLC 62% • DLCO 53% • 6 Minute walk: Walks 1100 feet with an initial sat of 96% dropping to 79% on room air Case #1 • CT scan • Subpleural fibrosis 3 Case #1 • CT scan • TtibTraction bronchi hitiectasis • • Honeycombing Case #1 • Lunggpy biopsy • Interstitial thickening • Temporal heterogeneity • Fibroblastic foci 4 Idiopathic Pulmonary Fibrosis • Most common ILD of unknown etiology • MilMainly aff fftects peopl e > >50 50 yo, mos t are over the age of 60 yo • Incidence is estimated at 7.4-10.7 cases per 100,000 per year • Prevalence of IPF is estimated at 13-20/100,000 • Most are current or former smokers • Potential risk factors for developing IPF include cigarette smoking, occupational/environmental