Hypermutation in Mantle Cell Lymphoma Does Not Indicate a Clinical Or Biological Subentity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Lymphoma and Multiple Myeloma Center
The Lymphoma and Multiple Myeloma Center What Sets Us Apart We provide multidisciplinary • Experienced, nationally and internationally recognized physicians dedicated exclusively to treating patients with lymphoid treatment for optimal survival or plasma cell malignancies and quality of life for patients • Cellular therapies such as Chimeric Antigen T-Cell (CAR T) therapy for relapsed/refractory disease with all types and stages of • Specialized diagnostic laboratories—flow cytometry, cytogenetics, and molecular diagnostic facilities—focusing on the latest testing lymphoma, chronic lymphocytic that identifies patients with high-risk lymphoid malignancies or plasma cell dyscrasias, which require more aggresive treatment leukemia, multiple myeloma and • Novel targeted therapies or intensified regimens based on the other plasma cell disorders. cancer’s genetic and molecular profile • Transplant & Cellular Therapy program ranked among the top 10% nationally in patient outcomes for allogeneic transplant • Clinical trials that offer tomorrow’s treatments today www.roswellpark.org/partners-in-practice Partners In Practice medical information for physicians by physicians We want to give every patient their very best chance for cure, and that means choosing Roswell Park Pathology—Taking the best and Diagnosis to a New Level “ optimal front-line Lymphoma and myeloma are a diverse and heterogeneous group of treatment.” malignancies. Lymphoid malignancy classification currently includes nearly 60 different variants, each with distinct pathophysiology, clinical behavior, response to treatment and prognosis. Our diagnostic approach in hematopathology includes the comprehensive examination of lymph node, bone marrow, blood and other extranodal and extramedullary tissue samples, and integrates clinical and diagnostic information, using a complex array of diagnostics from the following support laboratories: • Bone marrow laboratory — Francisco J. -

Low-Grade Non-Hodgkin Lymphoma Book
Low-grade non-Hodgkin lymphoma Low-grade non-Hodgkin lymphoma Follicular lymphoma Mantle cell lymphoma Marginal zone lymphomas Lymphoplasmacytic lymphoma Waldenström’s macroglobulinaemia This book has been researched and written for you by Lymphoma Action, the only UK charity dedicated to people affected by lymphoma. We could not continue to support you, your clinical team and the wider lymphoma community, without the generous donations of our incredible supporters. As an organisation we do not receive any government or NHS funding and so every penny received is truly valued. To make a donation towards our work, please visit lymphoma-action.org.uk/Donate 2 Your lymphoma type and stage Your treatment Key contact Name: Role: Contact details: Job title/role Name and contact details GP Consultant haematologist/ oncologist Clinical nurse specialist or key worker Treatment centre 3 About this book Low-grade (or indolent) non-Hodgkin lymphoma is a type of blood cancer that develops from white blood cells called lymphocytes. It is a broad term that includes lots of different types of lymphoma. This book explains what low-grade non-Hodgkin lymphoma is and how it is diagnosed and treated. It includes tips on coping with treatment and dealing with day-to-day life. The book is split into chapters. You can dip in and out of it and read the sections that are relevant to you at any given time. Important and summary points are written in the chapter colour. Lists practical tips and chapter summaries. Gives space for questions and notes. Lists other resources you might find useful, some of which are online. -

Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy
cancers Review Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy Miriam Marangon 1, Carlo Visco 2 , Anna Maria Barbui 3, Annalisa Chiappella 4, Alberto Fabbri 5, Simone Ferrero 6,7 , Sara Galimberti 8 , Stefano Luminari 9,10 , Gerardo Musuraca 11, Alessandro Re 12 , Vittorio Ruggero Zilioli 13 and Marco Ladetto 14,15,* 1 Department of Hematology, Azienda Sanitaria Universitaria Giuliano Isontina, 34129 Trieste, Italy; [email protected] 2 Section of Hematology, Department of Medicine, University of Verona, 37134 Verona, Italy; [email protected] 3 Hematology Unit, ASST Papa Giovanni XXIII, 24127 Bergamo, Italy; [email protected] 4 Division of Hematology, Fondazione IRCCS, Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] 5 Hematology Division, Department of Oncology, Azienda Ospedaliero-Universitaria Senese, 53100 Siena, Italy; [email protected] 6 Hematology Division, Department of Molecular Biotechnologies and Health Sciences, Università di Torino, 10126 Torino, Italy; [email protected] 7 Hematology 1, AOU Città della Salute e della Scienza di Torino, 10126 Torino, Italy 8 Hematology Unit, Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy; [email protected] 9 Hematology Unit, Azienda Unità Sanitaria Locale IRCCS di Reggio Emilia, 42123 Modena, Italy; [email protected] 10 Surgical, Medical and Dental Department of Morphological Sciences Related -

Primary Splenic and Nodal Marginal Zone Lymphoma
J. Clin. Exp. Hematopathol Vol. 45, No. 1, Aug 2005 Review Article Primary Splenic and Nodal Marginal Zone Lymphoma: Jacques Diebold, Agne`s Le Tourneau, Eva Comperat, Thierry Molina and Jose´ e Audouin Primary splenic and nodal marginal zone (MZ) lymphomas are rare small B cell lymphomas presenting with similar histopathologic features. The neoplastic cell population mostly consists of monocytoid B cells organized in a MZ pattern, associated with centrocytoid cells colonizing follicles. About 50% of cases have a monotypic plasma cell component. The different histopathologic patterns and differential diagnosis are discussed here. Both diseases share a similar immunophenotype, with the expression of B-cell associated antigens and restriction of immunoglobulin light chain. The only difference is the more frequent expression of IgD in splenic than in nodal lymphomas. The most recent findings in genetics and molecular biology are presented and discussed. The main clinical and biological symptoms are described and the similarity of some cases with Waldenstro¨ms macroglobulinemia is stressed. Both lymphomas present with the same type of bone marrow involvement with a high frequency of intravascular infiltrates, which can be associated with interstitial and nodular infiltrates. Transformation into diffuse large B cell lymphoma occurs in about 10 to 15% of the cases. The outcome in many splenic MZ lymphomas is characterized by a lengthy survival after splenectomy (9 to 13 years or longer), despite the absence of a consensus on the optimal treatment. Nodal MZ lymphoma has a more aggressive evolution and seems to only be curable at an early stage. Further studies are needed of both lymphomas to improve treatment and prognosis. -

Cells, Tissues and Organs of the Immune System
Immune Cells and Organs Bonnie Hylander, Ph.D. Aug 29, 2014 Dept of Immunology [email protected] Immune system Purpose/function? • First line of defense= epithelial integrity= skin, mucosal surfaces • Defense against pathogens – Inside cells= kill the infected cell (Viruses) – Systemic= kill- Bacteria, Fungi, Parasites • Two phases of response – Handle the acute infection, keep it from spreading – Prevent future infections We didn’t know…. • What triggers innate immunity- • What mediates communication between innate and adaptive immunity- Bruce A. Beutler Jules A. Hoffmann Ralph M. Steinman Jules A. Hoffmann Bruce A. Beutler Ralph M. Steinman 1996 (fruit flies) 1998 (mice) 1973 Discovered receptor proteins that can Discovered dendritic recognize bacteria and other microorganisms cells “the conductors of as they enter the body, and activate the first the immune system”. line of defense in the immune system, known DC’s activate T-cells as innate immunity. The Immune System “Although the lymphoid system consists of various separate tissues and organs, it functions as a single entity. This is mainly because its principal cellular constituents, lymphocytes, are intrinsically mobile and continuously recirculate in large number between the blood and the lymph by way of the secondary lymphoid tissues… where antigens and antigen-presenting cells are selectively localized.” -Masayuki, Nat Rev Immuno. May 2004 Not all who wander are lost….. Tolkien Lord of the Rings …..some are searching Overview of the Immune System Immune System • Cells – Innate response- several cell types – Adaptive (specific) response- lymphocytes • Organs – Primary where lymphocytes develop/mature – Secondary where mature lymphocytes and antigen presenting cells interact to initiate a specific immune response • Circulatory system- blood • Lymphatic system- lymph Cells= Leukocytes= white blood cells Plasma- with anticoagulant Granulocytes Serum- after coagulation 1. -
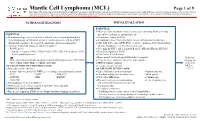
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

Divergent Clonal Evolution of a Common Precursor to Mantle Cell Lymphoma and Classic Hodgkin Lymphoma
Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Divergent clonal evolution of a common precursor to mantle cell lymphoma and classic Hodgkin lymphoma Hammad Tashkandi1, Kseniya Petrova-Drus1, Connie Lee Batlevi2, Maria Arcila1, Mikhail Roshal1, Filiz Sen1, Jinjuan Yao1, Jeeyeon Baik1, Ashley Bilger2, Jessica Singh2, Stephanie de Frank2, Anita Kumar2, Ruth Aryeequaye1, Yanming Zhang1, Ahmet Dogan1, Wenbin Xiao1,* 1Department of Pathology, 2Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY *Correspondence: Wenbin Xiao, MD, PhD Department of Pathology Memorial Sloan Kettering Cancer Center 1275 York Avenue New York, NY 10065 [email protected] Running title: Clonally related mantle cell lymphoma and classic Hodgkin lymphoma Words: 1771 Figures: 2 Tables: 1 Reference: 14 Supplemental materials: Figure S1-S2, Table S1-S4 Downloaded from molecularcasestudies.cshlp.org on September 23, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract: Clonal heterogeneity and evolution of mantle cell lymphoma (MCL) remain unclear despite the progress in our understanding of its biology. Here we report a 71 years old male patient with an aggressive MCL and depict the clonal evolution from initial diagnosis of typical MCL to relapsed blastoid MCL. During the course of disease, the patient was diagnosed with Classic Hodgkin lymphoma (CHL), and received CHL therapeutic regimen. Molecular analysis by next generation sequencing of both MCL and CHL demonstrated clonally related CHL with characteristic immunophenotype and PDL1/2 gains. Moreover, our data illustrate the clonal heterogeneity and acquisition of additional genetic aberrations including a rare fusion of SEC22B-NOTCH2 in the process of clonal evolution. -

Centers Differentiation Stages in Human Germinal Patterns Reflect
Cutting Edge: Polycomb Gene Expression Patterns Reflect Distinct B Cell Differentiation Stages in Human Germinal Centers This information is current as of September 27, 2021. Frank M. Raaphorst, Folkert J. van Kemenade, Elly Fieret, Karien M. Hamer, David P. E. Satijn, Arie P. Otte and Chris J. L. M. Meijer J Immunol 2000; 164:1-4; ; doi: 10.4049/jimmunol.164.1.1 Downloaded from http://www.jimmunol.org/content/164/1/1 References This article cites 22 articles, 11 of which you can access for free at: http://www.jimmunol.org/ http://www.jimmunol.org/content/164/1/1.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 27, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. c Cutting Edge: Polycomb Gene Expression Patterns Reflect Distinct B Cell Differentiation Stages in Human Germinal Centers Frank M. Raaphorst,1* Folkert J. van Kemenade,* Elly Fieret,* Karien M. -

1 | Page: Immune Cells and Tissues Swailes Cells and Tissues of The
Cells and Tissues of the Immune System N. Swailes, Ph.D. Department of Anatomy and Cell Biology Rm: B046A ML Tel: 5-7726 E-mail: [email protected] Required reading Mescher AL, Junqueira’s Basic Histology Text and Atlas, 12th Edition, Chapter 20: pp226-2480 Ross MH and Pawlina W, Histology: A text and Atlas, 6th Edition, Chapter 21: pp396-429 Learning objectives 1) Identify the major cells of the immune system and briefly outline their function 2) Describe the general structure of lymphoid tissue 3) Differentiate between primary and secondary immune organs 4) Identify the thymus and discuss the role of its cells in ‘educating’ immature T-cells 5) Identify a lymph node and outline how an immune response is triggered here 6) Identify the spleen and describe the role of red and white pulp in filtering the blood and reacting to blood borne antigens 7) Differentiate between MALT in the oral cavity (tonsils) 8) Know where to find and how to identify examples of BALT and GALT Major Take Home Points A. Lymphoid tissues are composed of different types of lymphocytes and supporting cells within a scaffold of Type III collagen/reticular fibers B. The major primary lymphoid organs are encapsulated organs where immature lymphocytes are born (bone marrow) and become immunocompetent (thymus) C. The major secondary lymphoid organs are encapsulated organs where immunocompetent lymphocytes differentiate into effector cells after exposure to antigen in the blood (spleen) or lymph (nodes) D. Mucosa Associated Lymphoid Tissues (MALT) are un-encapsulated areas of lymphoid tissue within the mucosa of organs that can be identified by their lining epithelium (tonsils, GALT: ileum and appendix, BALT) 1 | Page: Immune Cells and Tissues Swailes A1: Organization of the immune system 5a A. -

Mantle Cell Lymphoma Stefano A
Editorials and Perspectives ers in myeloproliferative diseases: relationships with JAK2 Pascutto C, et al. Relation between JAK2 (V617F) mutation V617 F status, clonality, and antiphospholipid antibodies. J status, granulocyte activation, and constitutive mobilization Thromb Haemost 2007;5:1679-85. of CD34+ cells into peripheral blood in myeloproliferative 17. Falanga A, Marchetti M, Vignoli A, Balducci D, Russo L, disorders. Blood 2006;107:3676-82. Guerini V, et al. V617F JAK-2 mutation in patients with 23. Alvarez-Larrán A, Arellano-Rodrigo E, Reverter JC, essential thrombocythemia: relation to platelet, granulo- Domingo A, Villamor N, Colomer D, et al. Increased cyte, and plasma hemostatic and inflammatory molecules. platelet, leukocyte, and coagulation activation in primary Exp Hematol 2007;35:702-11. myelofibrosis. Ann Hematol 2008;87:269-76. 18. Arellano-Rodrigo E, Alvarez-Larran A, Reverter JC, 24. Leibundgut EO, Horn MP, Brunold C, Pfanner-Meyer B, Colomer D, Villamor N, Bellosillo B, et al. Platelet turnover, Marti D, Hirsiger H, et al. Hematopoietic and endothelial coagulation factors, and soluble markers of platelet and progenitor cell trafficking in patients with myeloprolifera- endothelial activation in essential thrombocythemia: rela- tive diseases. Haematologica 2006;91:1465-72. tionship with thrombosis occurrence and JAK2 V617F allele 25. Sozer S, Fiel MI, Schiano T, Xu M, Mascarenhas J, Hoffman burden. Am J Hematol 2009;84:102-8. R. The presence of JAK2V617F mutation in the liver 19. Trappenburg MC, van Schilfgaarde M, Marchetti M, Spronk endothelial cells of patients with Budd-Chiari syndrome. HM, ten Cate H, Leyte A, et al. Elevated procoagulant Blood 2009;113:5246-9. -

Relapsed Mantle Cell Lymphoma: Current Management, Recent Progress, and Future Directions
Journal of Clinical Medicine Review Relapsed Mantle Cell Lymphoma: Current Management, Recent Progress, and Future Directions David A Bond 1,*, Peter Martin 2 and Kami J Maddocks 1 1 Division of Hematology, The Ohio State University, Columbus, OH 43210, USA; [email protected] 2 Division of Hematology and Oncology, Weill Cornell Medical College, New York, NY 11021, USA; [email protected] * Correspondence: [email protected] Abstract: The increasing number of approved therapies for relapsed mantle cell lymphoma (MCL) provides patients effective treatment options, with increasing complexity in prioritization and se- quencing of these therapies. Chemo-immunotherapy remains widely used as frontline MCL treatment with multiple targeted therapies available for relapsed disease. The Bruton’s tyrosine kinase in- hibitors (BTKi) ibrutinib, acalabrutinib, and zanubrutinib achieve objective responses in the majority of patients as single agent therapy for relapsed MCL, but differ with regard to toxicity profile and dosing schedule. Lenalidomide and bortezomib are likewise approved for relapsed MCL and are active as monotherapy or in combination with other agents. Venetoclax has been used off-label for the treatment of relapsed and refractory MCL, however data are lacking regarding the efficacy of this approach particularly following BTKi treatment. Anti-CD19 chimeric antigen receptor T-cell (CAR-T) therapies have emerged as highly effective therapy for relapsed MCL, with the CAR-T treatment brexucabtagene autoleucel now approved for relapsed MCL. In this review the authors summarize evidence to date for currently approved MCL treatments for relapsed disease including Citation: Bond, D.A; Martin, P.; sequencing of therapies, and discuss future directions including combination treatment strategies Maddocks, K.J Relapsed Mantle Cell and new therapies under investigation. -

Mantle Cell Lymphoma
Leukemia (1998) 12, 1281–1287 1998 Stockton Press All rights reserved 0887-6924/98 $12.00 http://www.stockton-press.co.uk/leu Mantle cell lymphoma: a retrospective study of 121 cases H Samaha1, C Dumontet1, N Ketterer1, I Moullet1, C Thieblemont1, F Bouafia1, E Callet-Bauchu2, P Felman2, F Berger3, G Salles1 and B Coiffier1 1Service d’He´matologie, Centre Hospitalier Lyon-Sud, Hospices Civils de Lyon, and UPRES-JE 1879 ‘He´mopathies Lymphoides malignes’, Universite´ Claude Bernard, Pierre-Be´nite; 2Laboratoire d’He´matologie, Centre Hospitalier Lyon-Sud, Hospices Civils de Lyon, Pierre-Be´nite; and 3Laboratoire d’Anatomie Pathologique, Hoˆpital Edouard-Herriot, Hospices Civils de Lyon, France Mantle cell lymphoma (MCL) patients represent a difficult prob- phoma usually begins as a disseminated disease with wide- lem, sometimes to establish the diagnosis but mostly because spread involvement of lymph nodes, spleen, bone marrow of their refractoriness to standard lymphoma treatments. Which treatments to apply and to whom is not yet defined. In this and other extranodal sites, specially the gastrointestinal tract study, we attempted to analyze the clinical features, to identify and Waldeyer ring. However, patients usually present a good the major prognostic factors, and to evaluate the outcome of performance status (PS) at diagnosis although adverse prog- 121 MCL patients treated in our institution between 1979 and nostic factors, such as high serum lactic dehydrogenase (LDH) 1997. Clinical data, treatment modalities, and International and 2-microglobulin levels, may be present. Initially, these Prognostic Index (IPI) score were evaluated. Median age was 63 patients usually respond to different types of therapy, but years.