The Role of Complement System and the Immune Response to Tuberculosis Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Blocking Properdin Prevents Complement-Mediated Hemolytic Uremic Syndrome and Systemic Thrombophilia
BASIC RESEARCH www.jasn.org Blocking Properdin Prevents Complement-Mediated Hemolytic Uremic Syndrome and Systemic Thrombophilia Yoshiyasu Ueda,1 Takashi Miwa,1 Damodar Gullipalli,1 Sayaka Sato,1 Daisuke Ito,1 Hangsoo Kim,1 Matthew Palmer,2 and Wen-Chao Song1 Departments of 1Systems Pharmacology and Translational Therapeutics and 2Pathology and Laboratory Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania ABSTRACT Background Properdin (P) is a positive regulator of the alternative pathway of complement activation. Although P inhibition is expected and has been shown to ameliorate the alternative pathway of comple- ment-mediated tissue injury in several disease models, it unexpectedly exacerbated renal injury in a murine model of C3 glomerulopathy. The role of P in atypical hemolytic uremic syndrome (aHUS) is uncertain. Methods We blocked P function by genetic deletion or mAb-mediated inhibition in mice carrying a factor H (FH) point mutation, W1206R (FHR/R), that causes aHUS and systemic thrombophilia with high mortality. Results Pdeficiency completely rescued FHR/R mice from premature death and prevented thrombocyto- penia, hemolytic anemia, and renal disease. It also eliminated macrovessel thrombi that were prevalent in FHR/R mice. All mice that received a function-blocking anti-P mAb for 8 weeks survived the experimental period and appeared grossly healthy. Platelet counts and hemoglobin levels were significantly improved in FHR/R mice after 4 weeks of anti-P mAb treatment. One half of the FHR/R mice treated with an isotype control mAb but none of the anti-P mAb-treated mice developed stroke-related neurologic disease. Anti-P mAb-treated FHR/R mice showed largely normal renal histology, and residual liver thrombi were detected in only three of 15 treated mice. -

Macrophage Activation Markers, CD163 and CD206, in Acute-On-Chronic Liver Failure
cells Review Macrophage Activation Markers, CD163 and CD206, in Acute-on-Chronic Liver Failure Marlene Christina Nielsen 1 , Rasmus Hvidbjerg Gantzel 2 , Joan Clària 3,4 , Jonel Trebicka 3,5 , Holger Jon Møller 1 and Henning Grønbæk 2,* 1 Department of Clinical Biochemistry, Aarhus University Hospital, 8200 Aarhus N, Denmark; [email protected] (M.C.N.); [email protected] (H.J.M.) 2 Department of Hepatology & Gastroenterology, Aarhus University Hospital, 8200 Aarhus N, Denmark; [email protected] 3 European Foundation for the Study of Chronic Liver Failure (EF-CLIF), 08021 Barcelona, Spain; [email protected] (J.C.); [email protected] (J.T.) 4 Department of Biochemistry and Molecular Genetics, Hospital Clínic-IDIBAPS, 08036 Barcelona, Spain 5 Translational Hepatology, Department of Internal Medicine I, Goethe University Frankfurt, 60323 Frankfurt, Germany * Correspondence: [email protected]; Tel.: +45-21-67-92-81 Received: 1 April 2020; Accepted: 4 May 2020; Published: 9 May 2020 Abstract: Macrophages facilitate essential homeostatic functions e.g., endocytosis, phagocytosis, and signaling during inflammation, and express a variety of scavenger receptors including CD163 and CD206, which are upregulated in response to inflammation. In healthy individuals, soluble forms of CD163 and CD206 are constitutively shed from macrophages, however, during inflammation pathogen- and damage-associated stimuli induce this shedding. Activation of resident liver macrophages viz. Kupffer cells is part of the inflammatory cascade occurring in acute and chronic liver diseases. We here review the existing literature on sCD163 and sCD206 function and shedding, and potential as biomarkers in acute and chronic liver diseases with a particular focus on Acute-on-Chronic Liver Failure (ACLF). -

In Sickness and in Health: the Immunological Roles of the Lymphatic System
International Journal of Molecular Sciences Review In Sickness and in Health: The Immunological Roles of the Lymphatic System Louise A. Johnson MRC Human Immunology Unit, MRC Weatherall Institute of Molecular Medicine, University of Oxford, John Radcliffe Hospital, Headington, Oxford OX3 9DS, UK; [email protected] Abstract: The lymphatic system plays crucial roles in immunity far beyond those of simply providing conduits for leukocytes and antigens in lymph fluid. Endothelial cells within this vasculature are dis- tinct and highly specialized to perform roles based upon their location. Afferent lymphatic capillaries have unique intercellular junctions for efficient uptake of fluid and macromolecules, while expressing chemotactic and adhesion molecules that permit selective trafficking of specific immune cell subsets. Moreover, in response to events within peripheral tissue such as inflammation or infection, soluble factors from lymphatic endothelial cells exert “remote control” to modulate leukocyte migration across high endothelial venules from the blood to lymph nodes draining the tissue. These immune hubs are highly organized and perfectly arrayed to survey antigens from peripheral tissue while optimizing encounters between antigen-presenting cells and cognate lymphocytes. Furthermore, subsets of lymphatic endothelial cells exhibit differences in gene expression relating to specific func- tions and locality within the lymph node, facilitating both innate and acquired immune responses through antigen presentation, lymph node remodeling and regulation of leukocyte entry and exit. This review details the immune cell subsets in afferent and efferent lymph, and explores the mech- anisms by which endothelial cells of the lymphatic system regulate such trafficking, for immune surveillance and tolerance during steady-state conditions, and in response to infection, acute and Citation: Johnson, L.A. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Cd1b Tetramers Bind T Cell Receptors to Identify a Mycobacterial
Published August 1, 2011 Brief Definitive Report CD1b tetramers bind T cell receptors to identify a mycobacterial glycolipid- reactive T cell repertoire in humans Anne G. Kasmar,1 Ildiko van Rhijn,1,2 Tan-Yun Cheng,1 Marie Turner,3 Chetan Seshadri,1 Andre Schiefner,4 Ravi C. Kalathur,4 John W. Annand,1 Annemieke de Jong,1 John Shires,5 Luis Leon,1 Michael Brenner,1 Ian A. Wilson,4 John D. Altman,5 and D. Branch Moody1 1Division of Rheumatology, Immunology and Allergy, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115 2Department of Infectious Diseases and Immunology, Faculty of Veterinary Medicine, Utrecht University, 3508 TD Utrecht, Netherlands 3Tuberculosis Treatment Unit, Lemuel Shattuck Hospital, Jamaica Plain, MA 02130 4Department of Molecular Biology and Skaggs Institute for Chemical Biology, the Scripps Research Institute, La Jolla, CA 92037 Downloaded from 5Emory Vaccine Center, Atlanta, GA 30329 Microbial lipids activate T cells by binding directly to CD1 and T cell receptors (TCRs) or by indirect effects on antigen-presenting cells involving induction of lipid autoantigens, CD1 transcription, or cytokine release. To distinguish among direct and indirect mechanisms, we developed fluorescent human CD1b tetramers and measured T cell staining. CD1b tetramer staining of T cells requires glucose monomycolate (GMM) antigens, is specific for TCR jem.rupress.org structure, and is blocked by a recombinant clonotypic TCR comprised of TRAV17 and TRBV4-1, proving that CD1b–glycolipid complexes bind the TCR. GMM-loaded tetramers brightly stain a small subpopulation of blood-derived cells from humans infected with Mycobacterium tuberculosis, providing direct detection of a CD1b-reactive T cell reper- toire. -
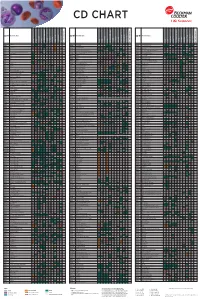
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Are Complement Deficiencies Really Rare?
G Model MIMM-4432; No. of Pages 8 ARTICLE IN PRESS Molecular Immunology xxx (2014) xxx–xxx Contents lists available at ScienceDirect Molecular Immunology j ournal homepage: www.elsevier.com/locate/molimm Review Are complement deficiencies really rare? Overview on prevalence, ଝ clinical importance and modern diagnostic approach a,∗ b Anete Sevciovic Grumach , Michael Kirschfink a Faculty of Medicine ABC, Santo Andre, SP, Brazil b Institute of Immunology, University of Heidelberg, Heidelberg, Germany a r a t b i c s t l e i n f o r a c t Article history: Complement deficiencies comprise between 1 and 10% of all primary immunodeficiencies (PIDs) accord- Received 29 May 2014 ing to national and supranational registries. They are still considered rare and even of less clinical Received in revised form 18 June 2014 importance. This not only reflects (as in all PIDs) a great lack of awareness among clinicians and gen- Accepted 23 June 2014 eral practitioners but is also due to the fact that only few centers worldwide provide a comprehensive Available online xxx laboratory complement analysis. To enable early identification, our aim is to present warning signs for complement deficiencies and recommendations for diagnostic approach. The genetic deficiency of any Keywords: early component of the classical pathway (C1q, C1r/s, C2, C4) is often associated with autoimmune dis- Complement deficiencies eases whereas individuals, deficient of properdin or of the terminal pathway components (C5 to C9), are Warning signs Prevalence highly susceptible to meningococcal disease. Deficiency of C1 Inhibitor (hereditary angioedema, HAE) Meningitis results in episodic angioedema, which in a considerable number of patients with identical symptoms Infections also occurs in factor XII mutations. -

Objectives Complement (C') Complement Proteins Functions Of
Complement Objectives Foundations of Public Health Identify functions of complement Immunology Recognize the similarities and differences of the three complement pathways Complement Identify important complement components & their functions Identify deleterious effects of complement activation and deficiency 1 2 Complement (C’) Complement Proteins Synthesized in the liver and by several Series of approximately 30 heat-labile proteins cells types (splenic macrophages) Normally inactive in the serum Plays an essential role in Inactive complement proteins known as zymogens inflammation and in facilitating Can be sequentially activated in a antibody effectiveness controlled sequence Amplification of the reaction occurs at each step Severe infections or autoimmune Production of biologically active fragments diseases can result from complement for lysis or killing of the target deficiencies (rare in the population) 3 4 Functions of Complement Functions of Complement Essential role in inflammation Assists antibodies in effector functions (Antibody Dependent Cell- mediated Cytotoxicity- ADCC) Assist in clearing immune complexes Opsonization and facilitation of phagocytosis No antigen specificity 5 6 1 Complement 3 Pathways of Activation Complement Activators Classical Triggered when IgM or certain IgG subclasses bind antigens Alternative (Properdin) Triggered by the deposition of complement protein, C3b, onto microbial surfaces No antibodies required for activation Lectin Triggered by the attachment of plasma mannose-binding lectin (MBL) to microbes No antibodies required for Activators start the domino effect… activation 7 8 Early Steps Late Steps The initial steps vary between pathways Dependent on activating substance C3 convertase quickly forms in all paths to cleave C3 Watch this well-done animation on the activation of complement, the Late steps (after C5 convertase) are same in all pathways steps in the complement pathways, Lead to formation of MAC & the functions of complement. -
Understanding the Complement System
Understanding the Complement System WHAT IS THE IMMUNE SYSTEM? The immune system is a complex network of organs, cells and proteins which work together to protect the body against infection and disease. WHAT IS THE COMPLEMENT SYSTEM? The complement system is a part of the immune system and is essential to the body’s defense against infection. Classical Pathway Lectin Pathway Alternative Pathway Made up of 3 UNIQUE PATHWAYS (Classical, Lectin and Alternative) Each pathway can become activated to trigger a cascade of protein reactions that initiate an immune response Inflammation Marks pathogen/damaged to detect and eliminate: cells for elimination Bacteria Viruses Inflammation Targeted destruction of damaged cells Dead cells When the complement system is working properly, it is a strong and powerful tool that protects the body against harmful invaders. • brain But when the system is thrown out of • nervous system balance, or dysregulated, the proteins can trigger a dangerous, uncontrolled cascade • blood stream of reactions that attack cells and tissues. • kidneys UNLOCKING THE POTENTIAL OF THE COMPLEMENT SYSTEM Alexion’s pioneering legacy in rare diseases is rooted in being the first to translate the complex biology of the complement system into transformative medicines. 3 DECADES 20 YEARS of complement of real-world evidence demonstrating the safety inhibition research and power of targeted complement inhibitors Dysregulation of the complement system is a key driver of many devastating diseases. Alexion has paved the way for a new class of medicines that inhibit the complement system, prevent further damage and reduce disease symptoms. Alexion is committed to continue unlocking the potential of the complement system and accelerating the discovery and development of new life-changing therapies for even more patients. -
Widely Used Commercial Elisa Does Not Detect Precursor of Haptoglobin2, but Recognizes Properdin As a Potential Second Member of the Zonulin Family
ORIGINAL RESEARCH published: 05 February 2018 doi: 10.3389/fendo.2018.00022 Widely Used Commercial ELISA Does Not Detect Precursor of Haptoglobin2, but Recognizes Properdin as a Potential Second Member of the Zonulin Family Lucas Scheffler1, Alyce Crane1, Henrike Heyne1, Anke Tönjes2, Dorit Schleinitz1, Christian H. Ihling3, Michael Stumvoll2, Rachel Freire4, Maria Fiorentino4, Alessio Fasano4, Peter Kovacs1* and John T. Heiker5* 1 Leipzig University Medical Center, IFB Adiposity Diseases, Leipzig, Germany, 2 Divisions of Endocrinology and Nephrology, University of Leipzig, Leipzig, Germany, 3 Department of Pharmaceutical Chemistry and Bioanalytics, Institute of Pharmacy, Martin-Luther-University Halle-Wittenberg, Halle, Germany, 4 Mucosal Immunology And Biology Research Center, Massachusetts General Hospital––Harvard Medical School, Boston, MA, United States, 5 Faculty of Biosciences, Pharmacy and Psychology, Institute of Biochemistry, University of Leipzig, Leipzig, Germany Background: There is increasing evidence for the role of impaired intestinal permeability Edited by: in obesity and associated metabolic diseases. Zonulin is an established serum marker for Dr Saumen Kumar Maitra, Visva-Bharati University, India intestinal permeability and identical to pre-haptoglobin2. Here, we aimed to investigate Reviewed by: the relationship between circulating zonulin and metabolic traits related to obesity. Yicong Li, Johns Hopkins Medicine, Methods: Serum zonulin was measured by using a widely used commercial ELISA kit in United States 376 subjects from the metabolically well-characterized cohort of Sorbs from Germany. In Asamanja Chattoraj, addition, haptoglobin genotype was determined in DNA samples from all study subjects. Institute of Bio-Resources and Sustainable Development, India Results: As zonulin concentrations did not correlate to the haptoglobin genotypes, *Correspondence: we investigated the specificity of the zonulin ELISA assay using antibody capture John T. -

O) 2 Platelets Mediated by Properdin and C3(H Complement Activation on Stimulated Identification of a Novel Mode Of
Identification of a Novel Mode of Complement Activation on Stimulated Platelets Mediated by Properdin and C3(H2 O) This information is current as of October 1, 2021. Gurpanna Saggu, Claudio Cortes, Heather N. Emch, Galia Ramirez, Randall G. Worth and Viviana P. Ferreira J Immunol 2013; 190:6457-6467; Prepublished online 15 May 2013; doi: 10.4049/jimmunol.1300610 Downloaded from http://www.jimmunol.org/content/190/12/6457 Supplementary http://www.jimmunol.org/content/suppl/2013/05/17/jimmunol.130061 Material 0.DC1 http://www.jimmunol.org/ References This article cites 72 articles, 37 of which you can access for free at: http://www.jimmunol.org/content/190/12/6457.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on October 1, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Identification of a Novel Mode of Complement Activation on Stimulated Platelets Mediated by Properdin and C3(H2O) Gurpanna Saggu,*,1 Claudio Cortes,*,†,1 Heather N.