Section 6 Nutritional Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Building a Better Breakfast
Building a Better Breakfast Most people have the best of intentions for breakfast. Ideally, weekday mornings would start with a handcrafted cold brew, good-for-you grain bowls, farm fresh eggs and an abundance of avocado. The kind of morning eats that will leave you well-nourished, perked up and ready to take on the day. Often life gets in the way of a healthy start, especially when you’re on the road. Yet instead of succumbing to carb-heavy or humdrum options, Re:fuel Pots from Aloft hotels puts a fresh—and flavorful—spin on instant-breakfast options. Redefining Breakfast on the Road For decades, heavy breakfasts such as doughnuts and bacon, egg and cheese sandwiches, dominated the on-the-go menu, with nary a vegetable or whole grain in sight. Toni Stoeckl, global brand leader and vice president of Distinctive Select Brands Marriott International, is ready to change that. He sees Aloft Hotels’ Re:fuel Pots as a way for guests to have an authentic café experience without having to leave the hotel. When developing the Pots, a global network of chefs came together to brainstorm ideas from more than 75 combinations, coming up with on-trend ideas and locally sourced eats. “We wanted to build something fast and efficient without sacrificing quality of ingredients,” Stoeckl says. By incorporating the most appealing elements of modern morning favorites like savory hashes, and classics like French toast and huevos rancheros, Re:fuel Pots are a fresh take on breakfast, neatly tucked into a well-designed package. Unlike a traditional dining room set up, these innovative Pots are ordered at sleek lobby kiosks and deliver a custom-built breakfast in a matter of minutes. -

Wellness Policies on Physical Activity and Nutrition
THE WHITNEY ACADEMY WELLNESS POLICIES ON PHYSICAL ACTIVITY AND NUTRITION INTRODUCTION As a standard of care, The Whitney Academy recognizes that children need access to healthful foods and opportunities to be physically active in order to grow, learn, and thrive; Good health fosters student attendance and educational progress. In designing the Whitney Academy’s Wellness Policies on Physical Activity and Nutrition, the following is taken into consideration: that obesity rates have doubled in children and tripled in adolescents over the last two decades, and that physical inactivity and excessive calorie intake are the predominant causes of obesity; that heart disease, cancer, stroke, and diabetes are responsible for two- thirds of deaths in the United States, and that the major risk factors for those diseases, including unhealthy eating habits, physical inactivity, and obesity are often are established in childhood. The Whitney Academy is committed to providing a school and residential environment that promotes and protects children's health, wellbeing, and ability to learn by supporting healthy eating and physical activity. Therefore, it is the policy of the Whitney Academy that: All students will have opportunities, support, and encouragement to be physically active on a regular basis. Foods and beverages served will meet the nutrition recommendations of the U.S. Dietary Guidelines for Americans. The Food Services Department / Cook / Registered Dietitian will provide students with access to a variety of nutritious and appealing foods that meet the health and nutrition needs of students. Whitney Academy will provide a clean, safe, and pleasant settings and adequate time for students to eat. The Medical, Residential, Education and Recreational Therapy staff will provide nutrition education and physical education to foster lifelong habits of healthy eating and physical activity, and will establish linkages between health education and the residential meal program. -

POST-OPERATIVE EXTRACTION INSTRUCTIONS Dr
POST-OPERATIVE EXTRACTION INSTRUCTIONS Dr. Scott Sahf’s Phone: 828-243-9121 Home care following Oral Surgery is important and recovery may be delayed, if this is neglected. Some swelling, stiffness and discomfort is to be expected after surgery. If this is greater than expected, please call or return for care. THE DAY OF SURGERY (first 24 hours) Bleeding: 1. Keep gauze pack in place for 30-60 minutes with constant, firm pressure. Do not chew on the gauze. 2. Replace gauze pack, as directed. 3. Keep head elevated and rest quietly. 4. Use an ice bag on the face, if so directed. 5. Some oozing of blood and discoloration of saliva is to be expected and is considered normal. You may want to use a dark towel over your pillow the first night to help prevent getting any blood on your pillow. Pain: 1. Take prescribed tablets for pain, or rest, if needed. Please see the other side of this paper for directions on Advil. General: 1. Your jaw may be sore for the first few days. 2. Place a dark towel on your pillow to prevent blood staining it. 3. Do not brush the areas where the teeth were removed. 4. If bleeding seems excessive, place a moist (not dripping) tea bag on extraction site for 30 minutes. 5. Do not eat any hard foods for the first 48 hours. Avoid: 1. Sucking on the wound. 2. Spitting. 3. Using a straw to drink with. 4. Smoking, dipping or chewing tobacco. 5. Strenuous exercising. 6. Rinsing with salt water or mouthwashes. -

Space Food and Nutrition
Educational Product National Aeronautics and Educators Grades K–8 Space Administration EG-1999-02-115-HQEG-1998-12-115-HQ SPACE FOOD AND NUTRITION An Educator’s Guide With Activities in Science and Mathematics Space and Food Nutrition—An Educator’s Guide With Activities in Science and Mathematics is available in electronic format through NASA Spacelink—one of the Agency’s electronic resources specifically developed for use by the educational community. The system may be accessed at the following address: http://spacelink.nasa.gov/products SPACE FOOD AND NUTRITION An Educator’s Guide With Activities in Science and Mathematics National Aeronautics and Space Administration This publication is in the Public Domain and is not protected by copyright. Permission is not required for duplication. EG-1999-02-115-HQ Space Food and Nutrition An Educator’s Guide With Activities in Science and Mathematics Acknowledgments National Aeronautics and Space Administration Special thanks to the following Office of Human Resources and Education contributors and reviewers Education Division Washington, D.C. Charles T. Bourland, Ph.D. System Manager, Space Station Food Education Working Group Flight Crew Support Division NASA Johnson Space Center NASA Johnson Space Center Houston, Texas Debbie A. Brown Writers ISS Education Liaison Angelo A. Casaburri Education Working Group Aerospace Education Services Program NASA Johnson Space Center NASA Johnson Space Center Houston, Texas Gregory L. Vogt, Ed.D. Crew Educational Affairs Liaison Cathy A. Gardner Education Working Group Dickinson Independent School District NASA Johnson Space Center Dickinson, Texas Karol L. Yeatts, Ed.D. Editor 1998 Einstein Fellow Jane A. George Miami Dade County Public Schools Teaching From Space Program Miami, Florida NASA Headquarters Washington, D.C. -
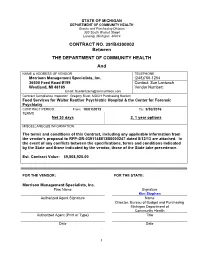
CONTRACT NO. 391B4300002 Between the DEPARTMENT OF
STATE OF MICHIGAN DEPARTMENT OF COMMUNITY HEALTH Grants and Purchasing Division 320 South Walnut Street Lansing, Michigan 48913 CONTRACT NO. 391B4300002 Between THE DEPARTMENT OF COMMUNITY HEALTH And NAME & ADDRESS OF VENDOR TELEPHONE Morrison Management Specialists, Inc. (248)760-1254 36500 Ford Road #199 Contact: Sue Lantzsch Westland, MI 48185 Vendor Number: Email: [email protected] Contract Compliance Inspector: Gregory Rivet, MDCH Purchasing Section Food Services for Walter Reuther Psychiatric Hospital & the Center for Forensic Psychiatry CONTRACT PERIOD: From: 10/01/2013 To: 9/30/2016 TERMS Net 30 days 2, 1 year options MISCELLANEOUS INFORMATION: The terms and conditions of this Contract, including any applicable information from the vendor's proposal to RFP-GR-0391148813B0000247 dated 8/12/13 are attached. In the event of any conflicts between the specifications, terms and conditions indicated by the State and those indicated by the vendor, those of the State take precedence. Est. Contract Value: $9,508,925.00 FOR THE VENDOR: FOR THE STATE: Morrison Management Specialists, Inc. Firm Name Signature Kim Stephen Authorized Agent Signature Name Director, Bureau of Budget and Purchasing Michigan Department of Community Health Authorized Agent (Print or Type) Title Date Date . 1 Table of Contents Contract Cover Page ................................................................................................................................................ 1 DEFINITIONS .................................................................................................................................... -

Victory for Democracy Movement in Czech. Christian Militias Join
VOL. XXIII NO. j)"9 THURSDAY, NOVEMBER 30, 1989 ... THE INDEPENDENT NEWSPAPER SERVING NOTRE DAME AND SAINT MARY'S Victory for democracy movement in Czech. PRAGUE, Czechoslovakia (AP) Monday in which millions of - The Communist-controlled workers participated. Parliament on Wednesday Parliament also eliminated swiftly ended the party's 40- the Communists' leading posi- year monopoly on power in a . tion in the National Front, an fran tic effort to satisfy the de umbrella organization embrac mands of the growing pro ing all political parties and so democracy movement. cial groups allowed in A member of the ruling Com Czechoslovakia. four deputies munist Politburo said the first opposed the measure and 16 fn~e elections in four decades abstained. could be held within a year. Shortly after the historic votes, state TV showed Slovak The 309 deputies present actor Milan Knazko announcing voted unanimously to scrap word of the changes to a Article 4 of the constitution. packed National Theater in which ensured the leading role Bratislava, capital of Slovakia. of the Communist Party, and The entire audience, which in change Article 16. whieh man cluded prominent dissident Va dated that all education be clav Havel, rose to its feet in bas1~d on Marxism-Leninism. thunderous, minute-long ap The changes were among his plause. toric concessions the opposi Parliament also planned to tion won from the Communist consider creating a constitu government on Tuesday when tional court and a commission Premier Ladislav Adamec also to investigate allegations of promised to form a new gov police brutality in a crackdown ernment. -

Meals for Easy Swallowing
1 INTRODUCTION Swallowing can become a significant problem for patients with ALS; and the joys and pleasures of eating become replaced with discomfort and anxiety. At an early stage patients may begin to have difficulty with foods such as popcorn, cornbread or nuts, and choking episodes may occur. Subsequently other foods cannot be swallowed readily, and the effort of chewing and swallowing turns a pleasurable experience into a burden. For the patient, the act of swallowing becomes compromised and the ordeal of eating becomes more time consuming. For the spouse, the task of preparing edible and appetizing foods poses an increasing challenge. The following collection of recipes is derived from our patients and their creative spouses who translated their caring into foods that look good, taste good, are easy to chew and to swallow, and minimize discomfort. Included are recipes for meats and other protein containing foods, fruits or fruit drinks, vegetables or dishes containing vegetables, as well as breads. Selections of beverages, desserts, and sauces are provided to add needed fat and calories to the diet. A balanced diet normally supplies enough nutrients for daily needs plus some extra. It is recommended that daily menu plans be made using the Basic Four Food Groups as the backbone. The suggested amounts are: Food GrouD Amount Per Dav Eauivalent to One Serving Milk 2 servings 1 cup pudding 1 cup milk or yogurt 1-3/4 cups ice cream 1-1/2 02. cheese 2 cups cottage cheese Meat 2 servings 2 02. lean meat, fish, poultry 2 eggs 4 Tbsps. -

Eating Hints: Before, During and After Cancer Treatment
Support for People with Cancer Eating Hints: Before, during, and after Cancer Treatment U.S. Department of Health & Human Services | National Institutes of Health The Use of Product or Brand Names Product or brand names that appear in this booklet are for example only. The U.S. Government does not endorse any specific product or brand. If products or brands are not mentioned, it does not mean or imply that they are not satisfactory. 1-800-4-CANCER (1-800-422-6237) About this Book Eating Hints is written for you—someone who is about to get, or is now getting, cancer treatment. Your family, friends, and others close to you may also want to read this book. You can use this book before, during, and after cancer treatment. It has hints about common types of eating problems, along with ways to manage them. This book covers: Î What you should know about cancer treatment, eating well, and eating problems Î How feelings can affect appetite Î Hints to manage eating problems Î How to eat well after cancer treatment ends Î Foods and drinks to help with certain eating problems Î Ways to learn more Talk with your doctor, nurse, or dietitian about any eating problems that might affect you during cancer treatment. He or she may suggest that you read certain sections or follow some of the tips. Rather than read this book from beginning to end, look at just those sections you need now. Later, you can always read more. www.cancer.gov i Table of Contents What You Should Know about Cancer Treatment, Eating Well, and Eating Problems .......................................................................................................................1 Feelings Can Affect Your Appetite ..............................................................................................7 List of Eating Problems ....................................................................................................................9 Appetite Loss .......................................................................................................................................... -

Sports Snacks: Food Options for Hungry Athletes | Active.Com Sports Snacks: Food Options for Hungry Athletes by Nancy Clark, MS RD CSSD • for Active.Com
Sports Snacks: Food Options for Hungry Athletes | Active.com Sports Snacks: Food Options for Hungry Athletes By Nancy Clark, MS RD CSSD • For Active.com "What should I eat before I exercise?" That’s a key question—as well as what to eat during extended exercise— that athletes commonly ask me. While they know the words carbs, proteins and fats, they often don't know how to translate those words into food choices. The goal of this article is to offer specific food suggestions to fit a variety of sports situations. This is far from a complete list. Please be sure to experiment with new pre- and during exercise foods to learn which ones settle best in your gut, don’t “talk back,” and enhance your performance. Pre-Event Carbo-Loading Dinner: • Pasta with tomato sauce, meatballs, green beans, French bread, low fat/skim milk, frozen yogurt with strawberries • Turkey with potato, stuffing, low fat gravy, winter squash, cranberry sauce, dinner rolls, apple crisp with reduced-fat ice cream Pre-Game Breakfast For example, 1 to 2 hours before a 9 a.m. cross-country meet or soccer game • Wheaties (or other dry cereal) with low fat milk and banana • Oatmeal with applesauce and brown sugar • Cream of Wheat with raisins • Bagel or English muffin with peanut butter • Poached eggs with two slices of toast • Yogurt and granola Liquid “Meals” If you have trouble digesting solid food • Fruit smoothie (milk, yogurt or juice blended with frozen berries, banana chunks) • Carnation Instant Breakfast • Boost • Ensure • Low fat chocolate milk • Vanilla pudding • Pureed peaches Brunch 4 hours before a 1 p.m. -

Nutrition In
Diane Javelli, RDCD Clinical Dietitian University of Washington Medical Ctr. Today’s Objectives Understand the importance of diet and nutrition in inflammatory bowel disease (IBD) Review the effects of IBD on nutritional state Outline dietary strategies that are helpful in controlling IBD symptoms Review what type of diet is best during a flare Identify key elements of nutrition support therapy Discuss alternative nutritional therapies Answer questions Nutrition for the IBD Patient: Nutritional Goals are the same for both Crohn’s and Ulcerative Colitis. Goal: Reduce inflammation and bowel irritation through nutritionally rich foods that nourish and heal the bowel. Importance of Diet & Nutrition Diet and nutrition are important parts of IBD management Diet is the actual food that is consumed Nutrition refers to properly absorbing food and staying healthy Incorporating good nutrition into your diet is essential According to the Crohn’s and Colitis Foundation of America: “Food does not cause IBD to develop or worsen inflammation, but some foods may aggravate the symptoms of IBD.” Complications: Nutrient deficiencies due to malabsorption. Strictures of the bowel leading to need for very soft or liquid diet. Dehydration. Weight loss. Need for surgery/ostomies. Nutritional Deficiencies: IBD is associated with decreased digestion and malabsorption of carbohydrates, protein, fat, water, and a variety of vitamins and minerals. Limited diet and low appetite can also lead to poor nutrition. Most common deficiencies: - Vitamin B12 - calcium - Vitamin D - iron - protein - folate/zinc Effects of IBD on Digestion/Absorption Crohn’s Disease: -Inflammation or surgical resection of small intestine makes patients less able to absorb nutrients. -

F.E.A.S.T. Family Recipes
F.E.A.S.T. Family Recipes Families Empowered and Supporting Treatment of Eating Disorders Welcome to the F.E.A.S.T. Family Recipe book! The parents of F.E.A.S.T. have a lot of experience with feeding their children during recovery from an eating disorder. What once seemed the most natural thing in the world can become a confusing and strange experience when anorexia or bulimia are at the dinner table as well. The recipes in this book are of two types: recipes for foods, and recipes for recovery. These recipes represent the experience, the wisdom, the work, and the joy of families struggling toward recovery. For more of the wisdom and humor of the F.E.A.S.T. community, please visit our website at FEAST-ED.org and and our online forum at AroundTheDinnerTable.org [email protected] F.E.A.S.T. Family Recipes Copyright © 2009 by Families Empowered and Supporting Treatment of Eating Disorders Acknowledgment To all the F.E.A.S.T. families and the Around the Dinner Table online forum. All rights reserved. No part of this book may be reproduced in any form or by any electronic or mechanical means including storage and retrieval systems without permission in writing from Families Empowered and Supporting Treatment of Eating Disorders Powered By Bookemon. www.bookemon.com [email protected] We Believe * Eating disorders are biologically based mental illnesses and fully treatable with a combination of nutritional, medical, and therapeutic supports. * Parents do not cause eating disorders, and patients do not choose eating disorders. -

Power Up! Food = FUEL
Power Up! Food = FUEL Gym America Nutrition Presentation Christy Hoban, MS RD As a high level athlete, a significant time is spent in the gym on skill, strength, conditioning and power work. This is all done of course to perform to the best of abilities. One factor that is often overlooked and that plays a huge part in this equation is nutrition. Without a doubt, nutrition can positively or negatively impact performance. Nutrition as a vital part of training can: 1. Enhance performance – speed, strength, stamina and power 2. Delay fatigue and enhance energy levels during exercise and throughout the day 3. Optimize body composition 4. Lead to better and faster recovery 5. Decrease soreness and inflammation 6. Reduce injury risk 7. Enhance immunity and reduce risk of illness 8. And outside the gym - improve academic performance There are a lot of great ways for gymnasts to get the right nutrition but it all takes a little planning. Gymnasts should make their eating plan a commitment just like any other part of training. Nutrition Keys to Success: 1. Take time to plan a strategic eating routine to improve performance 2. Fuel well all day long—especially before, during, and after workouts 3. Include POWER foods for all day long eating that are jam-packed with great nutrients 4. Implement a recovery nutrition program after workouts and competitions Book end workouts with good nutrition! Power Up! Food = FUEL The Right Fuel MIx A high performance racecar needs just the right fuel mix for peak performance. Peak athletic performance requires plenty of high quality nutrition in the same way.