Dissociation: Defining the Concept in Criminal Forensic Psychiatry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paranoid – Suspicious; Argumentative; Paranoid; Continually on The
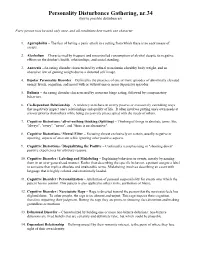
Disorder Gathering 34, 36, 49 Answer Keys A N S W E R K E Y, Disorder Gathering 34 1. Avital Agoraphobia – 2. Ewelina Alcoholism – 3. Martyna Anorexia – 4. Clarissa Bipolar Personality Disorder –. 5. Lysette Bulimia – 6. Kev, Annabelle Co-Dependant Relationship – 7. Archer Cognitive Distortions / all-of-nothing thinking (Splitting) – 8. Josephine Cognitive Distortions / Mental Filter – 9. Mendel Cognitive Distortions / Disqualifying the Positive – 10. Melvira Cognitive Disorder / Labeling and Mislabeling – 11. Liat Cognitive Disorder / Personalization – 12. Noa Cognitive Disorder / Narcissistic Rage – 13. Regev Delusional Disorder – 14. Connor Dependant Relationship – 15. Moira Dissociative Amnesia / Psychogenic Amnesia – (*Jason Bourne character) 16. Eylam Dissociative Fugue / Psychogenic Fugue – 17. Amit Dissociative Identity Disorder / Multiple Personality Disorder – 18. Liam Echolalia – 19. Dax Factitous Disorder – 20. Lorna Neurotic Fear of the Future – 21. Ciaran Ganser Syndrome – 22. Jean-Pierre Korsakoff’s Syndrome – 23. Ivor Neurotic Paranoia – 24. Tucker Persecutory Delusions / Querulant Delusions – 25. Lewis Post-Traumatic Stress Disorder – 26. Abdul Proprioception – 27. Alisa Repressed Memories – 28. Kirk Schizophrenia – 29. Trevor Self-Victimization – 30. Jerome Shame-based Personality – 31. Aimee Stockholm Syndrome – 32. Delphine Taijin kyofusho (Japanese culture-specific syndrome) – 33. Lyndon Tourette’s Syndrome – 34. Adar Social phobias – A N S W E R K E Y, Disorder Gathering 36 Adjustment Disorder – BERKELEY Apotemnophilia -

Psychogenic and Organic Amnesia. a Multidimensional Assessment of Clinical, Neuroradiological, Neuropsychological and Psychopathological Features
Behavioural Neurology 18 (2007) 53–64 53 IOS Press Psychogenic and organic amnesia. A multidimensional assessment of clinical, neuroradiological, neuropsychological and psychopathological features Laura Serraa,∗, Lucia Faddaa,b, Ivana Buccionea, Carlo Caltagironea,b and Giovanni A. Carlesimoa,b aFondazione IRCCS Santa Lucia, Roma, Italy bClinica Neurologica, Universita` Tor Vergata, Roma, Italy Abstract. Psychogenic amnesia is a complex disorder characterised by a wide variety of symptoms. Consequently, in a number of cases it is difficult distinguish it from organic memory impairment. The present study reports a new case of global psychogenic amnesia compared with two patients with amnesia underlain by organic brain damage. Our aim was to identify features useful for distinguishing between psychogenic and organic forms of memory impairment. The findings show the usefulness of a multidimensional evaluation of clinical, neuroradiological, neuropsychological and psychopathological aspects, to provide convergent findings useful for differentiating the two forms of memory disorder. Keywords: Amnesia, psychogenic origin, organic origin 1. Introduction ness of the self – and a period of wandering. According to Kopelman [33], there are three main predisposing Psychogenic or dissociative amnesia (DSM-IV- factors for global psychogenic amnesia: i) a history of TR) [1] is a clinical syndrome characterised by a mem- transient, organic amnesia due to epilepsy [52], head ory disorder of nonorganic origin. Following Kopel- injury [4] or alcoholic blackouts [20]; ii) a history of man [31,33], psychogenic amnesia can either be sit- psychiatric disorders such as depressed mood, and iii) uation specific or global. Situation specific amnesia a severe precipitating stress, such as marital or emo- refers to memory loss for a particular incident or part tional discord [23], bereavement [49], financial prob- of an incident and can arise in a variety of circum- lems [23] or war [21,48]. -
Diagnostic and Management Guidelines for Mental Disorders in Primary Care
Diagnostic and Management Guidelines for Mental Disorders in Primary Care ICD-10 Chapter V ~rimary Care Version Published on behalf of the World Health Organization by Hogrefe & Huber Publishers World Health Organization Hogrefe & Huber Publishers Seattle . Toronto· Bern· Gottingen Library of Congress Cataloging-in-Publication Data is available via the Library of Congress Marc Database under the LC Catalog Card Number 96-77394 Canadian Cataloguing in Publication Data Main entry under title: Diagnostic and management guidelines for mental disorders in primary care: ICD-lO chapter V, primary care version ISBN 0-88937-148-2 1. Mental illness - Classification. 2. Mental illness - Diagnosis. 3. Mental illness - Treatment. I. World Health Organization. 11. Title: ICD-ten chapter V, primary care version. RC454.128 1996 616.89 C96-931353-5 The correct citation for this book should be as follows: Diagnostic and Management Guidelines for Mental Disorders in Primary Care: ICD-lO Chapter V Primary Care Version. WHO/Hogrefe & Huber Publishers, Gottingen, Germany, 1996. © Copyright 1996 by World Health Organization All rights reserved. Hogrefe & Huber Publishers USA: P.O. Box 2487, Kirkland, WA 98083-2487 Phone (206) 820-1500, Fax (206) 823-8324 CANADA: 12 Bruce Park Avenue, Toronto, Ontario M4P 2S3 Phone (416) 482-6339 SWITZERLAND: Langgass-Strasse 76, CH-3000 Bern 9 Phone (031) 300-4500, Fax (031) 300-4590 GERMANY: Rohnsweg 25,0-37085 Gottingen Phone (0551) 49609-0, Fax (0551) 49609-88 No part of this book may be translated, reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, microfilming, recording or otherwise, without the written permission from the copyright holder. -

Guidelines for Treating Dissociative Identity Disorder in Adults, Third
This article was downloaded by: [208.78.151.82] On: 21 October 2011, At: 09:20 Publisher: Routledge Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered office: Mortimer House, 37-41 Mortimer Street, London W1T 3JH, UK Journal of Trauma & Dissociation Publication details, including instructions for authors and subscription information: http://www.tandfonline.com/loi/wjtd20 Guidelines for Treating Dissociative Identity Disorder in Adults, Third Revision International Society for the Study of Trauma and Dissociation Available online: 03 Mar 2011 To cite this article: International Society for the Study of Trauma and Dissociation (2011): Guidelines for Treating Dissociative Identity Disorder in Adults, Third Revision, Journal of Trauma & Dissociation, 12:2, 115-187 To link to this article: http://dx.doi.org/10.1080/15299732.2011.537247 PLEASE SCROLL DOWN FOR ARTICLE Full terms and conditions of use: http://www.tandfonline.com/page/terms-and-conditions This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden. The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae, and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand, or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material. -

Does Amnesia Specifically Predict Alzheimer's Pathology?
Does amnesia specifically predict Alzheimer’s pathology? A neuropathological study Maxime Bertoux, Pascaline Cassagnaud, Thibaud Lebouvier, Florence Lebert, Marie Sarazin, Isabelle Le Ber, Bruno Dubois, Brain Bank, Sophie Auriacombe, Didier Hannequin, et al. To cite this version: Maxime Bertoux, Pascaline Cassagnaud, Thibaud Lebouvier, Florence Lebert, Marie Sarazin, et al.. Does amnesia specifically predict Alzheimer’s pathology? A neuropathological study. Neurobiology of Aging, Elsevier, In press. hal-02898941 HAL Id: hal-02898941 https://hal.archives-ouvertes.fr/hal-02898941 Submitted on 14 Jul 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Amnesia/AD pathology 1 Does amnesia specifically predict Alzheimer’s pathology? A neuropathological study. Maxime Bertoux*1a, Pascaline Cassagnaud*b, Thibaud Lebouvier*c, Florence Leberta, Marie Sarazinde, Isabelle Le Berfg, Bruno Duboisfg, NeuroCEB Brain Bank, Sophie Auriacombeh, Didier Hannequini, David Walloni, Mathieu Ceccaldij, Claude-Alain Mauragek, Vincent Deramecourtc, Florence Pasquiera a Univ Lille, Lille Neuroscience & Cognition (Inserm UMRS1172) Degenerative and vascular cognitive disorders, CHU Lille, Laboratory of Excellence Distalz (Development of Innovative Strategies for a Transdisciplinary approach to ALZheimer’s disease). F-59000, Lille, France.F-59000, Lille, France. b Univ Lille, CHU Lille, Laboratory of Excellence Distalz (Development of Innovative Strategies for a Transdisciplinary approach to ALZheimer’s disease). -
Dissociative Identity Disorder: Adaptive Deception of Self and Others
Dissociative Identity Disorder: Adaptive Deception of Self and Others John 0. Beahrs, MD Dissociative identity disorder (multiple personality) is increasingly diagnosed, often follows childhood trauma. and is characterized bv riqidification of phenomena that resemble hypnosis. To inteipret dissociated aspeck of selfhood as autonomous entities is a useful heuristic; but when taken too literally, it leads to three kinds of anomaly: (1) legal: dissociators remain culpable for misdeeds carried out beyond apparent awareness or control; (2) clinical: legitimization sometimes leads not to relief, but to escalating cycles of regressive dependency; and (3) scientific: the form of dissociated entities varies with how they are defined, in ways that are intrinsically motivated and clinically manipulable. These anomalies yield to an evolutionary perspective that views dissociative identity disorder as an evolved strategy of adaptive deception of self and others; e.g., a beaten subordinate avoids further retribution by "pleading illness." Such a deceit best avoids detection when fully experienced; through its intensity and persistence, it becomes real at a new level. One's basic competencies remain intact, however, and are the source of the anomalies described. They can be clinically accessed and empowered, providing the key to therapeutic change when dissociative processes are problematic. Overall, despite clear impairment in subjective awareness and volition, dissociative-disor- dered individuals are best held fully accountable for the consequences of their actions. When deviant behavior becomes unac- ately excused and "treated."' To be held ceptable, society classifies the offending liable for retribution, transgressors must agents in two groups. Those defined as (1) know what they are doing and why, "bad" (culpable, blameworthy) are sub- and (2) be able to choose otherwise. -

When the Mind Falters: Cognitive Losses in Dementia
T L C When the Mind Falters: Cognitive Losses in Dementia by L Joel Streim, MD T Associate Professor of Psychiatry C Director, Geriatric Psychiatry Fellowship Program University of Pennsylvania VISN 4 Mental Illness Research Education and Clinical Center Philadelphia VA Medical Center Delaware Valley Geriatric Education Center The goal of this module is to teach direct staff about the syndrome of dementia and its clinical effects on residents. It focuses on the ways that the symptoms of dementia affect persons’ functional ability and behavior. We begin with an overview of the symptoms of cognitive impairment. We continue with a description of the causes, epidemiology, and clinical course (stages) of dementia. We then turn to a closer look at the specific areas of cognitive impairment, and examine how deficits in different areas of cognitive function can interfere with the person’s daily functioning, causing disability. The accompanying videotape illustrates these principles, using the example of a nursing home resident whose cognitive impairment interferes in various ways with her eating behavior and ability to feed herself. 1 T L Objectives C At the end of this module you should be able to: Describe the stages of dementia Distinguish among specific cognitive impairments from dementia L Link specific cognitive impairments with the T disabilities they cause C Give examples of cognitive impairments and disabilities Describe what to do when there is an acute change in cognitive or functional status Delaware Valley Geriatric Education Center At the end of this module you should be able to • Describe the stages of dementia. These are early, middle and late, and we discuss them in more detail. -

PAVOL JOZEF ŠAFARIK UNIVERSITY in KOŠICE Dissociative Amnesia: a Clinical and Theoretical Reconsideration DEGREE THESIS
PAVOL JOZEF ŠAFARIK UNIVERSITY IN KOŠICE FACULTY OF MEDICINE Dissociative amnesia: a clinical and theoretical reconsideration Paulo Alexandre Rocha Simão DEGREE THESIS Košice 2017 PAVOL JOZEF ŠAFARIK UNIVERSITY IN KOŠICE FACULTY OF MEDICINE FIRST DEPARTMENT OF PSYCHIATRY Dissociative amnesia: a clinical and theoretical reconsideration Paulo Alexandre Rocha Simão DEGREE THESIS Thesis supervisor: Mgr. MUDr. Jozef Dragašek, PhD., MHA Košice 2017 Analytical sheet Author Paulo Alexandre Rocha Simão Thesis title Dissociative amnesia: a clinical and theoretical reconsideration Language of the thesis English Type of thesis Degree thesis Number of pages 89 Academic degree M.D. University Pavol Jozef Šafárik University in Košice Faculty Faculty of Medicine Department/Institute Department of Psychiatry Study branch General Medicine Study programme General Medicine City Košice Thesis supervisor Mgr. MUDr. Jozef Dragašek, PhD., MHA Date of submission 06/2017 Date of defence 09/2017 Key words Dissociative amnesia, dissociative fugue, dissociative identity disorder Thesis title in the Disociatívna amnézia: klinické a teoretické prehodnotenie Slovak language Key words in the Disociatívna amnézia, disociatívna fuga, disociatívna porucha identity Slovak language Abstract in the English language Dissociative amnesia is a one of the most intriguing, misdiagnosed conditions in the psychiatric world. Dissociative amnesia is related to other dissociative disorders, such as dissociative identity disorder and dissociative fugue. Its clinical features are known -

The Diagnosis of Ganser Syndrome in the Practice of Forensic Psychology
Drob, S., & Meehan, K. (2000). The diagnosis of Ganser Syndrome in the practice of forensic psychology. American Journal of Forensic Psychology, 18(3), 37-62. The Diagnosis of Ganser Syndrome in the Practice of Forensic Psychology Sanford L. Drob, Ph.D. and Kevin Meehan Forensic Psychiatry Service, New York University—Bellevue Medical Center The authors gratefully acknowledge the contributions of Robert H. Berger, M.D., Alexander Bardey, M.D., David Trachtenberg, M.D., Ruth Jonas, Ph.D. and Arthur Zitrin, M.D. for their assistance in helping to formulate the case example presented herein. 1 Drob, S., & Meehan, K. (2000). The diagnosis of Ganser Syndrome in the practice of forensic psychology. American Journal of Forensic Psychology, 18(3), 37-62. Abstract Ganser syndrome, which is briefly described as a Dissociative Disorder NOS in the DSM-IV is a poorly understood and often overlooked clinical phenomenon. The authors review the literature on Ganser syndrome, offer proposed screening criteria, and propose a model for distinguishing Ganser syndrome from malingering. The “SHAM LIDO” model urges clinicians to pay close attention to Subtle symptoms, History of dissociation, Abuse in childhood, Motivation to malinger, Lying and manipulation, Injury to the brain, Diagnostic testing, and longitudinal Observations, in the assessment of forensic cases that present with approximate answers, pseudo-dementia, and absurd psychiatric symptoms. A case example illustrating the application of this model is provided. 2 Drob, S., & Meehan, K. (2000). The diagnosis of Ganser Syndrome in the practice of forensic psychology. American Journal of Forensic Psychology, 18(3), 37-62. In this paper we propose a model for diagnosing the Ganser syndrome and related dissociative/hysterical presentations and evaluating this syndrome in connection with forensic assessments. -
Paranoid Or Bizarre Delusions, Or Disorganized Speech and Thinking, and It Is Accompanied by Significant Social Or Occupational Dysfunction
Personality Disturbance Gathering, nr.34 (key to possible disturbances) Every person may be used only once, and all conditions best match one character. 1. Agoraphobia – The fear of having a panic attack in a setting from which there is no easy means of escape. 2. Alcoholism – Characterized by frequent and uncontrolled consumption of alcohol despite its negative effects on the drinker's health, relationships, and social standing. 3. Anorexia –An eating disorder characterized by refusal to maintain a healthy body weight, and an obsessive fear of gaining weight due to a distorted self image. 4. Bipolar Personality Disorder – Defined by the presence of one or more episodes of abnormally elevated energy levels, cognition, and mood with or without one or more depressive episodes. 5. Bulimia – An eating disorder characterized by recurrent binge eating, followed by compensatory behaviors. 6. Co-Dependant Relationship – A tendency to behave in overly passive or excessively caretaking ways that negatively impact one's relationships and quality of life. It often involves putting one's own needs at a lower priority than others while being excessively preoccupied with the needs of others. 7. Cognitive Distortions / all-of-nothing thinking (Splitting) – Thinking of things in absolute terms, like "always", "every", "never", and "there is no alternative". 8. Cognitive Distortions / Mental Filter – Focusing almost exclusively on certain, usually negative or upsetting, aspects of an event while ignoring other positive aspects. 9. Cognitive Distortions / Disqualifying the Positive – Continually reemphasizing or "shooting down" positive experiences for arbitrary reasons. 10. Cognitive Disorder / Labeling and Mislabeling – Explaining behaviors or events, merely by naming them in an over-generalized manner. -

Ganser's Syndrome : a Report of Two Unusual Presentations
Indian Journal of Psychiatry, 2001, 43 (3),273-275 GANSER'S SYNDROME : A REPORT OF TWO UNUSUAL PRESENTATIONS HARPREET S. DUGGAL, SUBHASH C. GUPTA, SOUMYA BASU, VINOD K. SINHA & CHRISTODAY. R. J. KHESS ABSTRACT Ganser's syndrome is a rare and controversial entity in psychiatric nosology. We report two cases ofGS, one developing in a 12-year-old boy, which had their onset during an episode of mania. After recovery from Ganser's syndrome, these cases were followed-up for two and five years, respectively. Interestingly both these patients evolved into bipolar disorder with one patient showing recurrence of Ganser symptoms with each subsequent episode. The importance of following-up and relevance of affective symptoms in GS is discussed. ' Keywords: Ganser's syndrome, bipolar disorder, child, follow-up. Perhaps no other psychiatric syndrome is CASE REPORT shrouded in so much confusion and controversy as regards to its nosological status and Case-1 : Patient, PK, a 12-year-old boy studying mechanism as is Ganser's syndrome (GS). It has in eighth standard, presented to us with complaints been viewed as a form of malingering, a variety of of acute onset and 15 days duration characterized histrionic personality disorder, a psychotic illness, by failure to recognize family members, tearfulness, a dissociative disorder, a factitious disorder, and irritability, talkativeness, reading and writing in an organic illness (Lishman, 1998). The present opposite direction, hearing voices and seeing classificatory systems classify it under images. Family history and past history were dissociative disorders. Though GS has been unremarkable. Physical examination was within reported to occur with other comorbid conditions normal limits. -

The Effect of Depersonalization and Derealization Symptoms
THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Thesis Submitted to The College of Arts and Sciences of the UNIVERSITY OF DAYTON In Partial Fulfillment of the Requirements for The Degree of Master of Arts in Psychology By Rhiannon A. Gibbs UNIVERSITY OF DAYTON Dayton, Ohio May 2018 THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Name: Gibbs, Rhiannon A. APPROVED BY: _______________________________________ Julie Walsh-Messinger, Ph.D. Faculty Advisor ______________________________________ Roger R. Reeb, Ph.D. Committee Member ______________________________________ Jackson A. Goodnight, Ph.D. Committee Member Concurrence: _______________________________________ Lee Dixon, Ph.D. Chair, Department of Psychology ii © Copyright by Rhiannon A. Gibbs All rights reserved 2018 ABSTRACT THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Name: Gibbs, Rhiannon A. University of Dayton Advisor: Dr. Julie Walsh-Messinger. Depersonalization and derealization symptoms affect sensation, perception, and emotion, producing subjective experiences of unreality and affective numbing (Simeon, 2004). Abnormalities in the amygdala, which is associated with emotional reactions such as anxiety and fear (LeDoux, 1993), have been observed in depersonalization and derealization and other psychiatric disorders, such as anxiety and depression (Sierra & Berrios, 1998). Olfactory deficits have been posited as a potential marker for psychiatric