Comparative Risks of Chronic Inhaled Corticosteroids and Macrolides for Bronchiectasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula Outside the ICU: a Case Series
International Journal of Environmental Research and Public Health Case Report Spontaneous Pneumothorax in COVID-19 Patients Treated with High-Flow Nasal Cannula outside the ICU: A Case Series Magdalena Nalewajska 1, Wiktoria Feret 1 , Łukasz Wojczy ´nski 1, Wojciech Witkiewicz 2 , Magda Wi´sniewska 1 and Katarzyna Kotfis 3,* 1 Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] (M.N.); [email protected] (W.F.); [email protected] (Ł.W.); [email protected] (M.W.) 2 Department of Cardiology, Pomeranian Medical University, 70–111 Szczecin, Poland; [email protected] 3 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70–111 Szczecin, Poland * Correspondence: katarzyna.kotfi[email protected] Abstract: The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a global pandemic and a burden to global health at the turn of 2019 and 2020. No targeted treatment for COVID-19 infection has been identified so far, thus supportive treatment, invasive and non-invasive oxygen support, and corticosteroids remain a common therapy. High-flow nasal cannula (HFNC), a non-invasive oxygen support method, has become a prominent treatment option for respiratory failure during the SARS-CoV-2 pandemic. Citation: Nalewajska, M.; Feret, W.; HFNC reduces the anatomic dead space and increases positive end-expiratory pressure (PEEP), Wojczy´nski,Ł.; Witkiewicz, W.; allowing higher concentrations and higher flow of oxygen. Some studies suggest positive effects of Wi´sniewska,M.; Kotfis, K. HFNC on mortality and avoidance of intubation. -

Legionnaires' Disease
epi TRENDS A Monthly Bulletin on Epidemiology and Public Health Practice in Washington Legionnaires’ disease Vol. 22 No. 11 Legionellosis is a bacterial respiratory infection which can result in severe pneumonia and death. Most cases are sporadic but legionellosis is an important public health issue because outbreaks can occur in hotels, communities, healthcare facilities, and other settings. Legionellosis Legionellosis was first recognized in 1976 when an outbreak affected 11.17 more than 200 people and caused more than 30 deaths, mainly among attendees of a Legionnaires’ convention being held at a Philadelphia hotel. Legionellosis is caused by numerous different Legionella species and serogroups but most epiTRENDS P.O. Box 47812 recognized infections are due to Olympia, WA 98504-7812 L. pneumophila serogroup 1. The extent to which this is due to John Wiesman, DrPH, MPH testing bias is unclear since only Secretary of Health L. pneumophila serogroup 1 is Kathy Lofy, MD identified via commonly used State Health Officer urine antigen tests; other species Scott Lindquist, MD, MPH Legionella pneumophila multiplying and serogroups must be identified in a human lung cell State Epidemiologist, through PCR or culture, tests Communicable Disease www.cdc.gov which are less commonly ordered. Jerrod Davis, P.E. Assistant Secretary The disease involves two clinically distinct syndromes: Pontiac fever, Disease Control and Health Statistics a self-limited flu-like illness without pneumonia; and Legionnaires’ disease, a potentially fatal pneumonia with initial symptoms of fever, Sherryl Terletter Managing Editor cough, myalgias, malaise, and sometimes diarrhea progressing to symptoms of pneumonia which can be severe. Health conditions that Marcia J. -

The Child with Altered Respiratory Status
Path: K:/LWW-BOWDEN-09-0101/Application/LWW-BOWDEN-09-0101-016.3d Date: 3rd July 2009 Time: 16:31 User ID: muralir 1BlackLining Disabled CHAPTER 16 The Child With Altered Respiratory Status Do you remember the Diaz fam- Case History leave Lela, the baby sister, ily from Chapter 9, in which with Claudia’s mother, Selma, Jose has trouble taking his asthma medication, and head to the hospital. and in Chapter 4, in which Jose’s little sister, At the hospital the emergency department Lela, expresses her personality even as a new- nurse observes Jose sitting cross-legged and born? Jose is 4 years old and was diagnosed leaning forward on his hands. His mouth is with asthma this past fall, about 6 months ago. open and he is breathing hard with an easily Since that time Claudia, his mother, has audible inspiratory wheeze. He is using his noticed several factors that trigger his asthma subclavicular accessory muscles with each including getting sick, pollen, and cold air. breath. His respiratory rate is 32 breaths per One evening following a warm early-spring minute, his pulse is 112 beats per minutes, day, Jose is outside playing as the sun sets and and he is afebrile. Claudia explains that he the air cools. When he comes inside he was fine; he was outside running and playing, begins to cough. Claudia sets up his nebulizer and then came in and began coughing and and gives him a treatment of albuterol, which wheezing, and she gave him an albuterol lessens his coughing. Within an hour, Jose is treatment. -

Pneumonia: Prevention and Care at Home
FACT SHEET FOR PATIENTS AND FAMILIES Pneumonia: Prevention and Care at Home What is it? On an x-ray, pneumonia usually shows up as Pneumonia is an infection of the lungs. The infection white areas in the affected part of your lung(s). causes the small air sacs in your lungs (called alveoli) to swell and fill up with fluid or pus. This makes it harder for you to breathe, and usually causes coughing and other symptoms that sap your energy and appetite. How common and serious is it? Pneumonia is fairly common in the United States, affecting about 4 million people a year. Although for many people infection can be mild, about 1 out of every 5 people with pneumonia needs to be in the heart hospital. Pneumonia is most serious in these people: • Young children (ages 2 years and younger) • Older adults (ages 65 and older) • People with chronic illnesses such as diabetes What are the symptoms? and heart disease Pneumonia symptoms range in severity, and often • People with lung diseases such as asthma, mimic the symptoms of a bad cold or the flu: cystic fibrosis, or emphysema • Fatigue (feeling tired and weak) • People with weakened immune systems • Cough, without or without mucus • Smokers and heavy drinkers • Fever over 100ºF or 37.8ºC If you’ve been diagnosed with pneumonia, you should • Chills, sweats, or body aches take it seriously and follow your doctor’s advice. If your • Shortness of breath doctor decides you need to be in the hospital, you will receive more information on what to expect with • Chest pain or pain with breathing hospital care. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Obliterative Bronchiolitis, Cryptogenic Organising Pneumonitis and Bronchiolitis Obliterans Organizing Pneumonia: Three Names for Two Different Conditions
Eur Reaplr J EDITORIAL 1991, 4, 774-775 Obliterative bronchiolitis, cryptogenic organising pneumonitis and bronchiolitis obliterans organizing pneumonia: three names for two different conditions R.M. du Bois, O.M. Geddes Over the last five years, increasing confusion has has been applied to conditions in which airflow obstruc developed over the use of the terms "bronchiolitis tion is prominent and in which response to treatment is obliterans" and "bronchiolitis obliterans organizing poor. pneumonia". The confusion stems largely from the common use of the term "bronchiolitis obliterans" or "obliterative bronchiolitis" in the diagnostic labels applied "Cryptogenic organizing pneumonitis" or "bronchi· to two entities which are quite distinct clinically but which otitis obliterans organizing pneumonia" (BOOP) bear certain resemblances histologically. Cryptogenic organizing pneumonitis was first described by DAVISON et al. [7] in 1983. The clinical syndrome ObUterative bronchiolitis consisted of breathlessness, malaise, fever, high erythrocyte sedimentation rate (ESR), pneumonic In 1977, GEODES et al. [1] reported the case histories shadowing on chest radiograph with a restrictive of six patients whose clinical condition was characterized pulmonary function defect and low gas transfer coeffi by airways obliteration in association with rheumatoid cient. On histological examination of lung biopsy mate· arthritis. The striking clinical features were of rapidly rial, the typical and distinguishing feature was the progressive breathlessness and the fmding on examination presence of connective tissue within the alveoli, alveolar of a high-pitched mid-inspiratory squeak heard over the ducts and, occasionally, in respiratory bronchioles. This lung fields. Chest radiographs showed hyperinflated lungs connective tissue consisted of "loosely woven fibres of but were otherwise normal. -

To Honeycombing in Idiopathic Pulmonary Fibrosis
Piciucchi et al. BMC Pulmonary Medicine (2016) 16:87 DOI 10.1186/s12890-016-0245-x CORRESPONDENCE Open Access From “traction bronchiectasis” to honeycombing in idiopathic pulmonary fibrosis: A spectrum of bronchiolar remodeling also in radiology? Sara Piciucchi1*, Sara Tomassetti2, Claudia Ravaglia2, Christian Gurioli2, Carlo Gurioli2, Alessandra Dubini3, Angelo Carloni4, Marco Chilosi5, Thomas V Colby6 and Venerino Poletti2,7 Abstract Background: The diagnostic and prognostic impact of traction bronchiectasis on high resolution CT scan (HRCT) in patients suspected to have idiopathic pulmonary fibrosis (IPF) is increasing significantly. Main body: Recent data demonstrated that cysts in honeycombing areas are covered by epithelium expressing bronchiolar markers. In IPF bronchiolization is the final consequence of a variety of pathogenic events starting from alveolar stem cell exhaustion, and ending in a abnormal/dysplastic proliferation of bronchiolar epithelium. CT scan features of traction bronchiectasis and honeycombing should be interpreted under the light of these new pathogenetic and morphologic considerations. Short conclusion: We suggest that in IPF subjects traction bronchiectasis and honeycombing -now defined as distinct entities on HRCT scan- are actually diverse aspects of a continuous spectrum of lung remodeling. Keywords: Traction bronchiectasis, Honeycombing, Fibroblastic Foci, Bronchiolar dysplastic proliferation Background Mechanical stress may contribute to the subpleural Histologically, Usual Interstitial Pneumonia (UIP) is and usually basilar localization of UIP changes [10, 11]. characterized by a combination of “patchy fibrosis” and The final stage of this “bronchiolization” process cor- fibroblastic foci displaying a “patchwork pattern”. Disease responds radiologically to honeycombing, typically seen progression is characterized by the appearance of air- first in the subpleural regions of the lower lobes [2, 3]. -
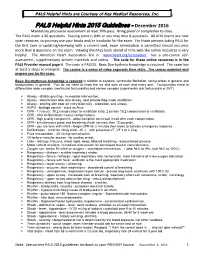
PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory Precourse Assessment at Least 70% Pass
PALSPALS Helpful Helpful Hints Courtesy Hints are of CourtesyKey Medical of Resources, Key Medical Inc. Resources, www.cprclassroom.com Inc. PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory precourse assessment at least 70% pass. Bring proof of completion to class. The PALS exam is 50 questions. Passing score is 84% or you may miss 8 questions. All AHA exams are now open resource, so you may use your books and/or handouts for the exam. For those persons taking PALS for the first time or updating/renewing with a current card, exam remediation is permitted should you miss more than 8 questions on the exam. Viewing the PALS book ahead of time with the online resources is very helpful. The American Heart Association link is www.heart.org/eccstudent has a pre-course self- assessment, supplementary written materials and videos. The code for these online resources is in the PALS Provider manual page ii. The code is PALS15. Basic Dysrhythmia knowledge is required. The exam has at least 5 strips to interpret. The course is a series of video segments then skills. The course materials well prepare you for the exam. Basic Dysrhythmias knowledge is required in relation to asystole, ventricular fibrillation, tachycardias in general and bradycardias in general. You do not need to know the ins and outs of each and every one. Tachycardias need to differentiate wide complex (ventricular tachycardia) and narrow complex (supraventricular tachycardia or SVT). Airway - child is grunting - immediate intervention. Airway - deteriorates after oral airway, next provide bag-mask ventilation. Airway - snoring with poor air entry bilaterally - reposition, oral airway. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS. -

Klebsiella Pneumoniae in Diffuse Panbronchiolitis
※ 附來的圖四解析度和原來一樣哦 , 應該不是原始檔案 , 如沒有原圖印刷就是字不漂亮 DOI:10.6314/JIMT.202012_31(6).07 內科學誌 2020:31:432-436 Klebsiella Pneumoniae in Diffuse Panbronchiolitis Hwee-Kheng Lim1, Sho-Ting Hung2, and Shih-Yi Lee3,4 1Division of Infectious Diseases, Department of Medicine, 2Department of Radiology, 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Taitung MacKay Memorial Hospital, Taitung, Taiwan; 4MacKay Medicine, Nursing & Management College Abstract Diffuse panbronchiolitis (DPB) is a chronic, idiopathic, rare but lethal inflammatory airway disease resulting in distal airway dilation, obstructive lung disease, hypoxemia, and increased in the susceptibility of bacteria colonization. The case reports that a patient with destructive lung gets pneumonia by Klebsiella pneu- moniae cured by bactericidal antibiotics, but K. pneumoniae in the airway is eradicated with erythromycin, which therefore highlights not only the importance to the testing for DPB in suspicious patients, but also the therapeutic strategies in managing DPB with K. pneumoniae in the airways. (J Intern Med Taiwan 2020; 31: 432-436) Key Words: Klebsiella pneumoniae, Panbronchiolitis Introduction the survival of the patients with DPB in the literature also reduces P. aeruginosa isolated from the sputum. Diffuse panbronchiolitis (DPB) is a chronic P. aeruginosa in sputum appears to accelerate the inflammatory disease of the airways, and the diag- destructive process3. However, the role of Klebsiella nosis depends on the clinical symptoms, physical pneumoniae in DPB has never been reported. We signs, typical chest radiographic findings, low FEV1 present a patient with DPB and K. pneumoniae iso- (< 70%) in pulmonary function tests, low arterial lated from sputum, refractory to ampicillin/sulbac- partial pressure (< 80 mmHg), elevated cold hem- tam, but eradicated by erythromycin. -

Legionellosis: Legionnaires' Disease/ Pontiac Fever
Legionellosis: Legionnaires’ Disease/ Pontiac Fever What is legionellosis? Legionellosis is an infection caused by the bacterium Legionella pneumophila, which acquired its name in 1976 when an outbreak of pneumonia caused by this newly recognized organism occurred among persons attending a convention of the American Legion in Philadelphia. The disease has two distinct forms: • Legionnaires' disease, the more severe form of infection which includes pneumonia, and • Pontiac fever, a milder illness. How common is legionellosis in the United States? An estimated 8,000 to 18,000 people get Legionnaires' disease in the United States each year. Some people can be infected with the Legionella bacterium and have mild symptoms or no illness at all. Outbreaks of Legionnaires' disease receive significant media attention. However, this disease usually occurs as a single isolated case not associated with any recognized outbreak. When outbreaks do occur, they are usually recognized in the summer and early fall, but cases may occur year-round. About 5% to 30% of people who have Legionnaires' disease die. What are the usual symptoms of legionellosis? Patients with Legionnaires' disease usually have fever, chills, and a cough. Some patients also have muscle aches, headache, tiredness, loss of appetite, and, occasionally, diarrhea. Chest X-rays often show pneumonia. It is difficult to distinguish Legionnaires' disease from other types of pneumonia by symptoms alone; other tests are required for diagnosis. Persons with Pontiac fever experience fever and muscle aches and do not have pneumonia. They generally recover in 2 to 5 days without treatment. The time between the patient's exposure to the bacterium and the onset of illness for Legionnaires' disease is 2 to 10 days; for Pontiac fever, it is shorter, generally a few hours to 2 days.