Relpax® Utilization Management Criteria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ERJ-01090-2018.Supplement
Shaheen et al Online data supplement Prescribed analgesics in pregnancy and risk of childhood asthma Seif O Shaheen, Cecilia Lundholm, Bronwyn K Brew, Catarina Almqvist. 1 Shaheen et al Figure E1: Data available for analysis Footnote: Numbers refer to adjusted analyses (complete data on covariates) 2 Shaheen et al Table E1. Three classes of analgesics included in the analyses ATC codes Generic drug name Opioids N02AA59 Codeine, combinations excluding psycholeptics N02AA79 Codeine, combinations with psycholeptics N02AA08 Dihydrocodeine N02AA58 Dihydrocodeine, combinations N02AC04 Dextropropoxyphene N02AC54 Dextropropoxyphene, combinations excluding psycholeptics N02AX02 Tramadol Anti-migraine N02CA01 Dihydroergotamine N02CA02 Ergotamine N02CA04 Methysergide N02CA07 Lisuride N02CA51 Dihydroergotamine, combinations N02CA52 Ergotamine, combinations excluding psycholeptics N02CA72 Ergotamine, combinations with psycholeptics N02CC01 Sumatriptan N02CC02 Naratriptan N02CC03 Zolmitriptan N02CC04 Rizatriptan N02CC05 Almotriptan N02CC06 Eletriptan N02CC07 Frovatriptan N02CX01 Pizotifen N02CX02 Clonidine N02CX03 Iprazochrome N02CX05 Dimetotiazine N02CX06 Oxetorone N02CB01 Flumedroxone Paracetamol N02BE01 Paracetamol N02BE51 Paracetamol, combinations excluding psycholeptics N02BE71 Paracetamol, combinations with psycholeptics 3 Shaheen et al Table E2. Frequency of analgesic classes prescribed to the mother during pregnancy Opioids Anti- Paracetamol N % migraine No No No 459,690 93.2 No No Yes 9,091 1.8 Yes No No 15,405 3.1 No Yes No 2,343 0.5 Yes No -

Antimigraine Agents, Triptans Review 07/21/2008
Antimigraine Agents, Triptans Review 07/21/2008 Copyright © 2004 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended -
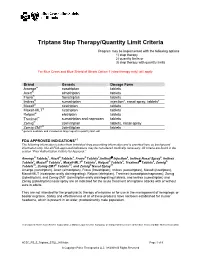
Triptans Step Therapy/Quantity Limit Criteria
Triptans Step Therapy/Quantity Limit Criteria Program may be implemented with the following options 1) step therapy 2) quantity limits or 3) step therapy with quantity limits For Blue Cross and Blue Shield of Illinois Option 1 (step therapy only) will apply. Brand Generic Dosage Form Amerge® naratriptan tablets Axert® almotriptan tablets Frova® frovatriptan tablets Imitrex® sumatriptan injection*, nasal spray, tablets* Maxalt® rizatriptan tablets Maxalt-MLT® rizatriptan tablets Relpax® eletriptan tablets Treximet™ sumatriptan and naproxen tablets Zomig® zolmitriptan tablets, nasal spray Zomig-ZMT® zolmitriptan tablets * generic available and included as target agent in quantity limit edit FDA APPROVED INDICATIONS1-7 The following information is taken from individual drug prescribing information and is provided here as background information only. Not all FDA-approved indications may be considered medically necessary. All criteria are found in the section “Prior Authorization Criteria for Approval.” Amerge® Tablets1, Axert® Tablets2, Frova® Tablets3,Imitrex® injection4, Imitrex Nasal Spray5, Imitrex Tablets6, Maxalt® Tablets7, Maxalt-MLT® Tablets7, Relpax® Tablets8, Treximet™ Tablets9, Zomig® Tablets10, Zomig-ZMT® Tablets10, and Zomig® Nasal Spray11 Amerge (naratriptan), Axert (almotriptan), Frova (frovatriptan), Imitrex (sumatriptan), Maxalt (rizatriptan), Maxalt-MLT (rizatriptan orally disintegrating), Relpax (eletriptan), Treximet (sumatriptan/naproxen), Zomig (zolmitriptan), and Zomig-ZMT (zolmitriptan orally disintegrating) tablets, and Imitrex (sumatriptan) and Zomig (zolmitriptan) nasal spray are all indicated for the acute treatment of migraine attacks with or without aura in adults. They are not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic or basilar migraine. Safety and effectiveness of all of these products have not been established for cluster headache, which is present in an older, predominantly male population. -

RELPAX® (Eletriptan Hydrobromide) Tablets
RELPAX® (eletriptan hydrobromide) Tablets DESCRIPTION RELPAX® (eletriptan) Tablets contain eletriptan hydrobromide, which is a selective 5 hydroxytryptamine 1B/1D (5-HT1B/1D) receptor agonist. Eletriptan is chemically designated as (R)-3-[(1-Methyl-2-pyrrolidinyl)methyl]-5-[2-(phenylsulfonyl)ethyl]-1H indole monohydrobromide, and it has the following chemical structure: CH OO OO 3 N S . HBr N H The empirical formula is C22H26N2O2S . HBr, representing a molecular weight of 463.40. Eletriptan hydrobromide is a white to light pale colored powder that is readily soluble in water. Each RELPAX Tablet for oral administration contains 24.2 or 48.5 mg of eletriptan hydrobromide equivalent to 20 mg or 40 mg of eletriptan, respectively. Each tablet also contains the inactive ingredients microcrystalline cellulose NF, lactose NF, croscarmellose sodium NF, magnesium stearate NF, titanium dioxide USP, hypromellose, triacetin USP and FD&C Yellow No. 6 aluminum lake. CLINICAL PHARMACOLOGY Mechanism of Action: Eletriptan binds with high affinity to 5-HT1B, 5-HT1D and 5-HT1F receptors, has modest affinity for 5-HT1A, 5-HT1E, 5-HT2B and 5-HT7 receptors, and little or no affinity for 5-HT2A, 5-HT2C, 5-HT3, 5-HT4, 5-HT5A and 5-HT6 receptors. Eletriptan has no significant affinity or pharmacological activity at adrenergic alpha1, alpha2, or beta; dopaminergic D1 or D2; muscarinic; or opioid receptors. Two theories have been proposed to explain the efficacy of 5-HT receptor agonists in migraine. One theory suggests that activation of 5-HT1 receptors located on intracranial blood vessels, including those on the arteriovenous anastomoses, leads to vasoconstriction, which is correlated with the relief of migraine headache. -

Ergomar (Ergotamine) P&T Approval Date 4/2017, 6/2017, 3/2018, 3/2019, 1/2020, 1/2021 Effective Date 4/1/2021; Oxford Only: 4/1/2021
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 2125-6 Program Prior Authorization/Medical Necessity Medication Dihyroergotamine nasal spray (Migranal)*, Ergomar (ergotamine) P&T Approval Date 4/2017, 6/2017, 3/2018, 3/2019, 1/2020, 1/2021 Effective Date 4/1/2021; Oxford only: 4/1/2021 1. Background: Migranal (dihydroergotamine) nasal spray is indicated for the acute treatment of migraine headaches with or without aura. Migranal nasal spray is not intended for the prophylactic therapy of migraine or for the management of hemiplegic or basilar migraine. Ergomar is indicated to abort or prevent vascular headache, for example, migraine, migraine variants or a so-called "histaminic cephalalgia”. Ergomar should not be used for chronic daily administration. The U.S. Headache Consortium guidelines offer a general strategy based on expert consensus. Nonsteroidal anti-inflammatory drugs (NSAIDs) or caffeine-containing combination analgesics may be first-line treatment for mild to moderate migraine, or severe migraine that has previously responded to these agents. Triptans are considered first-line abortive treatment of moderate to severe migraine, or mild attacks that have not responded to nonprescription medicines. Ergotamine-containing compounds may also be reasonable in this situation. This program requires a member to try one oral triptan and one nasal triptan prior to receiving coverage for brand or generic Migranal or two oral triptans prior to receiving coverage of Ergomar. 2. Coverage Criteriaa: A. Dihydroergotamine Nasal Spray (Migranal*) will be approved based on all of the following criteria: 1. Diagnosis of moderate to severe migraine headaches with or without aura. -AND- 2. History of failure, contraindication, or intolerance to one of the following oral triptans (Document duration of trial): a. -
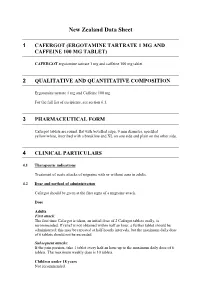
New Zealand Data Sheet
New Zealand Data Sheet 1 CAFERGOT (ERGOTAMINE TARTRATE 1 MG AND CAFFEINE 100 MG TABLET) CAFERGOT ergotamine tartrate 1 mg and caffeine 100 mg tablet 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Ergotamine tartrate 1 mg and Caffeine 100 mg For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Cafergot tablets are round, flat with bevelled edge, 9 mm diameter, speckled yellow/white, inscribed with a breakline and XL on one side and plain on the other side. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of acute attacks of migraine with or without aura in adults. 4.2 Dose and method of administration Cafergot should be given at the first signs of a migraine attack. Dose Adults First attack: The first time Cafergot is taken, an initial dose of 2 Cafergot tablets orally, is recommended. If relief is not obtained within half an hour, a further tablet should be administered; this may be repeated at half-hourly intervals, but the maximum daily dose of 6 tablets should not be exceeded. Subsequent attacks: If the pain persists, take 1 tablet every half an hour up to the maximum daily dose of 6 tablets. The maximum weekly dose is 10 tablets. Children under 18 years Not recommended. Maximum dose per attack or per day Adults: 6 mg ergotamine tartrate = 6 tablets. Maximum weekly dose Adults: 10 mg ergotamine tartrate = 10 tablets. Special populations Renal impairment Cafergot is contraindicated in patients with severe renal impairment (see Contraindications). Hepatic impairment Cafergot is contraindicated in patients with severe hepatic impairment (see Contraindications). -

Triptan Therapy for Acute Migraine
Triptan Therapy for Acute Migraine Headache John Farr Rothrock, MD University of Alabama at Birmingham, Birmingham, AL Deborah I. Friedman, MD, MPH University of Texas Southwestern, Dallas, TX The “triptans” are 5HT-1B/1D receptor agonists that were developed to treat acute migraine and acute cluster headache. Sumatriptan, the original triptan preparation, has been in general use since 1993, so there has been considerable experience with triptans over time. There are currently seven oral triptans on the market in the United States: sumatriptan (Imitrex™), naratriptan (Amerge™), zolmitriptan (Zomig™), rizatriptan (Maxalt™), almotriptan (Axert™), frovatriptan (Frova™), and eletriptan (Relpax™); brand names may differ by country. There is also a combination preparation of oral sumatriptan/naproxen (Treximet™). Two triptans (sumatriptan, zolmitriptan) are marketed as nasal sprays, and sumatriptan is available for subcutaneous injection, including a needle-free subcutaneous delivery system (Sumavel™). Sumatriptan suppositories are marketed in Europe but not in North America. Zolmitriptan and rizatriptan are sold in an oral disintegrating tablet or “melt” formulation as well as in tablet form; while the “melt” formulations may be more convenient (no liquid is required to propel them into the stomach), they are absorbed similarly to regular tablets and there is no evidence to suggest that they work faster than the tablet formulations. Some patients with migraine-associated nausea prefer the disintegrating tablets while others cannot tolerate their taste. Although all of the triptans initially were investigated for the treatment of migraine headache of moderate to severe intensity and were superior to placebo in those pivotal trials, they appear to be more consistently effective when used to treat migraine earlier in the attack, when the headache is still mild to moderate. -

Headache Treatment in Children, Menstruation, Pregnancy and Lactation, Elderly, Renal Disease
Headache Treatment in Children, Menstruation, Pregnancy and Lactation, Elderly, Renal Disease Andrew D. Hershey, MD, PhD Director, Headache Center Cincinnati Children’s Hospital Medical Center Professor of Pediatrics and Neurology University of Cincinnati, College of Medicine Objectives • Discuss unique aspects of headache treatment in special populations –Children –Menstruation – Pregnancy and Lactation –Elderly – Renal Disease Children • Unique aspects of headache treatment in children – Developmentally appropriate intervention – Integration of family and school •Treatment – Acute pediatric issues – ED and inpatient management – Preventative therapy –Biobehavioral therapy ® American Headache Society “Unique” aspects of children • Family-centered interview – Child is the patient • “Only you know what the headache feels like” • Parental observation without parental interpretation – Unified treatment plan • Patient and parent to agree – Young child – parent provides the treatment – Teenager – resistant to parental pressure “Unique” aspects of children • Family-centered interview – Tools to utilize • Questionnaire • Disability assessments – PedMIDAS, PedsQL •Drawings • School letters • Calendars and diaries – Expectations discussed • Headache gone within 1 hour and back to normal • 1-2 headaches per month without missing activities • Limited long-term use of medication Diagnosis ® American Headache Society Classification of Headache International Classification of Headache Disorders – 2nd Edition, Cephalalgia, 2004 • Primary headache disorders -

US8074644.Pdf
USOO8074644B2 (12) United States Patent (10) Patent No.: US 8,074,644 B2 Hale et al. (45) Date of Patent: *Dec. 13, 2011 (54) METHOD OF FORMING AN AEROSOL FOR (56) References Cited NHALATION DELVERY (75) Inventors: Ron L. Hale, Sandia Park, NM (US); U.S. PATENT DOCUMENTS Craig C. Hodges, Walnut Creek, CA 1,239,634 A 9, 1917 Stuart (US); Peter M. Lloyd, Walnut Creek, CA (US); Daniel Mufson, Napa, CA (Continued) (US); Daniel D. Rogers, Oakland, CA (US); Soonho Song, Hillsborough, CA FOREIGN PATENT DOCUMENTS (US); Martin J. Wensley, Los Gatos, CA 2152684 1, 1996 CA (US); Daniel J. Myers, Mountain (Continued) View, CA (US); Jeffrey A. McKinney, Lafayette, CA (US); Reynaldo J. OTHER PUBLICATIONS Quintana, Redwood City, CA (US); U.S. Appl. No. 1 1/687,466, filed Mar. 16, 2007, Zaffaroni et al. Joshua D. Rabinowitz, Princeton, NJ (US) (Continued) (73) Assignee: Alexza Pharmaceuticals, Inc., Primary Examiner — Steven Douglas Mountain View, CA (US) (74) Attorney, Agent, or Firm — Swanson & Bratschun, (*) Notice: Subject to any disclaimer, the term of this L.L.C. patent is extended or adjusted under 35 (57) ABSTRACT U.S.C. 154(b) by 272 days. The present invention relates to the inhalation delivery of This patent is Subject to a terminal dis aerosols containing Small particles. Specifically, it relates to a claimer. method of forming an aerosol for use in inhalation therapy. In (21) Appl. No.: 12/471,070 a method aspect of the present invention, a method of forming (22) Filed: May 22, 2009 an aerosol for use in inhalation therapy is provided. -

How Do I Choose Acute Treatment Medication Options for Migraine Patients?
How Do I Choose Acute Treatment Medication Options for Migraine Patients? Laura Xanders, FNP-BC Maureen Moriarty, DNP, APRN, FAHS, FAANP Step 1: Conduct a history of present illness (HPI) What is their migraine frequency? • What is the frequency of the paent’s moderate to severe migraine aacks? • What associated symptoms do they experience with their migraine aacks? • Are their migraine aacks rapid or gradual in onset? What do they currently take? • Do they get complete relief? • How oSen do they take it? • Can they tolerate oral medicaon during a migraine aack? What have they tried in the past that has or has not worked? Step 2: Determine any comorbid condiIons or concurrent medicaons that may be a contraindicaon to an acute migraine medicaon. A patient with a history of stomach A patient with a history of Pregnancy/lactation status ulcer may not be a good candidate cardiovascular disease or could impact safe or approved for an oral NSAID uncontrolled hypertension use of a medication may not be a good candidate for a triptan Step 3: Review the available acute medicaon opIons. 1. NSAIDs • Faster onset: diclofenac powder, ketorolac IM, ketorolac NS • Slower onset: naproxen, ibuprofen, diclofenac, indomethacin 2. Triptans • Short half life: sumatriptan, rizatriptan, eletriptan, almotriptan, zolmitriptan • Long half life: naratriptan, frovatriptan • Non-PO: sumatriptan NS, zolmitriptan NS, sumatriptan SQ 3. Acute CGRP antagonists (gepants) • ubrogepant • rimegepant 4. Ditans • lasmiditan 5. An-emecs* • metoclopramide • prochlorperazine • promethazine • ondansetron * Metoclopramide, prochlorperazine and promethazine have addiIonal direct anI-migraine effect but may be sedang, and ondansetron has no direct anI-migraine effect but is not sedang. -

Triptans: Almotriptan, Amerge®, Axert®, Frova®, Imitrex® and Sumatriptan Tablets/Nasal Spray/Injection, Maxalt/MLT®, Naratriptan, Onzetra™
Drug Therapy Guidelines Triptans: almotriptan, Amerge®, Axert®, Frova®, Imitrex® and sumatriptan tablets/nasal spray/injection, Maxalt/MLT®, naratriptan, Onzetra™ Xsail™, Relpax® and eletriptan tablets, rizatriptan/ODT, Sumavel®, Tosymra™, Treximet®, Zembrace™ SymTouch™, zolmitriptan/ODT tablets, Applicable Zomig/ZMT® tablets/nasal spray Medical Benefit Effective: 5/28/2021 Pharmacy- Formulary 1 x Next Review: 3/22 Pharmacy- Formulary 2 x Date of Origin: 8/29/06 Pharmacy- Formulary 3/Exclusive x Review Dates: 8/06, 11/07, 12/08, 12/09, 6/10, 3/11, 3/12, 3/13, Pharmacy- Formulary 4/AON x 3/14, 3/15, 3/16, 3/17, 3/18, 3/19, 3/20, 2/21, 3/21 I. Medication Description Serotonin receptor agonists are used to treat (not prevent) acute attacks of migraine headaches. These medications work by binding to specific serotonin receptors in the brain which in turn decreases the release of chemicals responsible for the vasodilation of cerebral blood vessels, decreases the activity of pain signaling neurons, and reduces inflammation. II. Position Statement For all lines of business, coverage is provided immediately, without requiring prior authorization, for preferred/formulary medications with associated quantity limit restrictions. Quantity limitations criteria do not apply when the medication is requested by a neurologist. Coverage is determined through a prior authorization process with supporting clinical evidence for all other requests for members aged 18 and older. III. Policy Formulary 1: See Sections B and C Formulary 2: See Sections A and C Formulary 3/Exclusive: See Sections A and C Formulary 4/AON: See Sections A and C A. Non-preferred medications: Amerge, Axert, Frova, Imitrex, Maxalt, Onzetra, Relpax, Tosymra, Treximet, Zembrace, Zomig, Zolmitriptan nasal spray Plan-preferred medications: eletriptan, naratriptan, rizatriptan, sumatriptan, zolmitriptan tablets, zolmitriptan oral disintegrating tablets B. -

Eletriptan in the Management of Acute Migraine
TAN0010.1177/1756285616650619Therapeutic Advances in Neurological DisordersM Capi, M Curto View metadata, citation and similar650619research-article2016 papers at core.ac.uk brought to you by CORE provided by Archivio della ricerca- Università di Roma La Sapienza Therapeutic Advances in Neurological Disorders Review Ther Adv Neurol Disord Eletriptan in the management of acute 2016, Vol. 9(5) 414 –423 DOI: 10.1177/ migraine: an update on the evidence for 1756285616650619 © The Author(s), 2016. Reprints and permissions: efficacy, safety, and consistent response http://www.sagepub.co.uk/ journalsPermissions.nav Matilde Capi, Martina Curto, Luana Lionetto, Fernando de Andrés, Giovanna Gentile, Andrea Negro and Paolo Martelletti Abstract: Migraine is a multifactorial, neurological and disabling disorder, also characterized by several autonomic symptoms. Triptans, selective serotonin 5-HT1B/1D agonists, are the first-line treatment option for moderate-to-severe headache attacks. In this paper, we review the recent data on eletriptan clinical efficacy, safety, and tolerability, and potential clinically relevant interactions with other drugs. Among triptans, eletriptan shows a consistent and significant clinical efficacy and a good tolerability profile in the treatment of migraine, Correspondence to: especially for patients with cardiovascular risk factors without coronary artery disease. It Martina Curto, MD Sapienza University shows the most favorable clinical response, together with sumatriptan injections, zolmitriptan of Rome, Azienda and rizatriptan. Additionally, eletriptan shows the most complex pharmacokinetic/dynamic Ospedaliera Sant’Andrea Via di Grottarossa 1035- profile compared with the other triptans. It is metabolized primarily by the CYP3A4 hepatic 1039, Rome 00189, Italy enzyme and therefore the concomitant administration of CYP3A4-potent inhibitors should [email protected] Matilde Capi, MSc be carefully evaluated.