New Zealand Data Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ergot Alkaloids Mycotoxins in Cereals and Cereal-Derived Food Products: Characteristics, Toxicity, Prevalence, and Control Strategies
agronomy Review Ergot Alkaloids Mycotoxins in Cereals and Cereal-Derived Food Products: Characteristics, Toxicity, Prevalence, and Control Strategies Sofia Agriopoulou Department of Food Science and Technology, University of the Peloponnese, Antikalamos, 24100 Kalamata, Greece; [email protected]; Tel.: +30-27210-45271 Abstract: Ergot alkaloids (EAs) are a group of mycotoxins that are mainly produced from the plant pathogen Claviceps. Claviceps purpurea is one of the most important species, being a major producer of EAs that infect more than 400 species of monocotyledonous plants. Rye, barley, wheat, millet, oats, and triticale are the main crops affected by EAs, with rye having the highest rates of fungal infection. The 12 major EAs are ergometrine (Em), ergotamine (Et), ergocristine (Ecr), ergokryptine (Ekr), ergosine (Es), and ergocornine (Eco) and their epimers ergotaminine (Etn), egometrinine (Emn), egocristinine (Ecrn), ergokryptinine (Ekrn), ergocroninine (Econ), and ergosinine (Esn). Given that many food products are based on cereals (such as bread, pasta, cookies, baby food, and confectionery), the surveillance of these toxic substances is imperative. Although acute mycotoxicosis by EAs is rare, EAs remain a source of concern for human and animal health as food contamination by EAs has recently increased. Environmental conditions, such as low temperatures and humid weather before and during flowering, influence contamination agricultural products by EAs, contributing to the Citation: Agriopoulou, S. Ergot Alkaloids Mycotoxins in Cereals and appearance of outbreak after the consumption of contaminated products. The present work aims to Cereal-Derived Food Products: present the recent advances in the occurrence of EAs in some food products with emphasis mainly Characteristics, Toxicity, Prevalence, on grains and grain-based products, as well as their toxicity and control strategies. -

Anti-Migraine Agents Reference Number: OH.PHAR.PPA.34 Effective Date: 01.01.21 Last Review Date: 11.20 Line of Business: Medicaid
Clinical Policy: Anti-Migraine Agents Reference Number: OH.PHAR.PPA.34 Effective Date: 01.01.21 Last Review Date: 11.20 Line of Business: Medicaid See Important Reminder at the end of this policy for important regulatory and legal information. Description • When using a preferred agent where applicable, the number of tablets/doses allowed per month will be restricted based on the manufacturer’s package insert and/or Buckeye Health plans quantity limits. CNS AGENTS: ANTI-MIGRAINE AGENTS – ACUTE MIGRANE TREATMENT NO PA REQUIRED “PREFERRED” STEP THERAPY REQUIRED PA REQUIRED “NON-PREFERRED” “PREFERRED” NARATRIPTAN (GENERIC OF AMERGE®) NURTEC™ ODT (rimegepant) ALMOTRIPTAN (generic of Axert®) RIZATRIPTAN TABLETS (GENERIC OF CAFERGOT® (ergotamine w/caffeine) MAXALT®) ELETRIPTAN (generic of Relpax®) RIZATRIPTAN ODT (GENERIC OF ERGOMAR® (ergotamine) MAXALT-MLT®) FROVA® (frovatriptan) SUMATRIPTAN TABLETS, NASAL SPRAY, MIGERGOT® (ergotamine w/caffeine) INJECTION (GENERIC OF MIGRANAL® (dihydroergotamine) IMITREX®) ONZETRA™ XSAIL™ (sumatriptan) REYVOW™ (lasmiditan) SUMAVEL DOSEPRO® (sumatriptan) TOSYMRA® (sumatriptan) TREXIMET® (sumatriptan/naproxen) UBRELVY™ (ubrogepant)* ZOLMITRIPTAN (generic of Zomig®) ZOLMITRIPTAN ODT (generic of Zomig ZMT®) ZOMIG® NASAL SPRAY (zolmitriptan) CNS AGENTS: ANTI-MIGRAINE AGENTS – CLUSTER HEADACHE TREATMENT NO PA REQUIRED “PREFERRED” PA REQUIRED “NON-PREFERRED” VERAPAMIL (Generic of Calan®) EMGALITY™ (galcanezumab) VERAPAMIL SR/ER (Generic of Calan SR®, Isoptin SR®, Verelan®) CNS AGENTS: ANTI-MIGRAINE AGENTS – PROPHYLAXIS TREATMENT NO PA REQUIRED “PREFERRED” STEP THERAPY REQUIRED PA REQUIRED “NON-PREFERRED” (Trials of at least 3 controller “PREFERRED” medications) Cardiovascular Agents: Beta-blockers AIMOVIG™ (erenumab-aooe) † EMGALITY™ (galcanezumab) CNS Agents: Anticonvulsants AJOVY™ (fremanezumab-vfrm) * CNS Agents: Serotonin-norepinephrine reuptake inhibitors CNS Agents: Tricyclic antidepressants †Initial Dose is limited to 70mg once monthly; may request dose increase if 70mg fails to provide adequate relief over two consecutive months. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

ERJ-01090-2018.Supplement
Shaheen et al Online data supplement Prescribed analgesics in pregnancy and risk of childhood asthma Seif O Shaheen, Cecilia Lundholm, Bronwyn K Brew, Catarina Almqvist. 1 Shaheen et al Figure E1: Data available for analysis Footnote: Numbers refer to adjusted analyses (complete data on covariates) 2 Shaheen et al Table E1. Three classes of analgesics included in the analyses ATC codes Generic drug name Opioids N02AA59 Codeine, combinations excluding psycholeptics N02AA79 Codeine, combinations with psycholeptics N02AA08 Dihydrocodeine N02AA58 Dihydrocodeine, combinations N02AC04 Dextropropoxyphene N02AC54 Dextropropoxyphene, combinations excluding psycholeptics N02AX02 Tramadol Anti-migraine N02CA01 Dihydroergotamine N02CA02 Ergotamine N02CA04 Methysergide N02CA07 Lisuride N02CA51 Dihydroergotamine, combinations N02CA52 Ergotamine, combinations excluding psycholeptics N02CA72 Ergotamine, combinations with psycholeptics N02CC01 Sumatriptan N02CC02 Naratriptan N02CC03 Zolmitriptan N02CC04 Rizatriptan N02CC05 Almotriptan N02CC06 Eletriptan N02CC07 Frovatriptan N02CX01 Pizotifen N02CX02 Clonidine N02CX03 Iprazochrome N02CX05 Dimetotiazine N02CX06 Oxetorone N02CB01 Flumedroxone Paracetamol N02BE01 Paracetamol N02BE51 Paracetamol, combinations excluding psycholeptics N02BE71 Paracetamol, combinations with psycholeptics 3 Shaheen et al Table E2. Frequency of analgesic classes prescribed to the mother during pregnancy Opioids Anti- Paracetamol N % migraine No No No 459,690 93.2 No No Yes 9,091 1.8 Yes No No 15,405 3.1 No Yes No 2,343 0.5 Yes No -

Summary of Product Characteristics
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [Invented name] 12.5 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains almotriptan 12.5 mg (as almotriptan malate 17.5 mg). For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet. Description: white to off-white, round, biconvex film-coated tablets, diameter of tablets max.6.2 mm. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Acute treatment of the headache phase of migraine attacks with or without aura. 4.2 Posology and method of administration Almotriptan should be taken with liquids as early as possible after the onset of migraine- associated headache but it is also effective when taken at a later stage. Almotriptan should not be used for migraine prophylaxis. The tablets can be taken with or without food. Adults (18-65 years of age) The recommended dose is one tablet containing 12.5 mg of almotriptan. A second dose may be taken if the symptoms reappear within 24 hours. This second dose may be taken provided that there is a minimum interval of two hours between the two doses. The efficacy of a second dose for the treatment of the same attack when an initial dose is ineffective has not been examined in controlled trials. Therefore if a patient does not respond to the first dose, a second dose should not be taken for the same attack. The maximum recommended dose is two doses in 24 hours. Children and adolescents (under 18 years of age) There are no data concerning the use of almotriptan in children and adolescents, therefore its use in this age group is not recommended. -

The Notification of Injuries from Hazardous Substances
The Notification of Injuries from Hazardous Substances Draft Guidelines and Reference Material for Public Health Services To be used to assist in a pilot study from July – December 2001 April 2001 Jeff Fowles, Ph.D. Prepared by the Institute of Environmental Science and Research, Limited Under contract by the New Zealand Ministry of Health DISCLAIMER This report or document ("the Report") is given by the Institute of Environmental Science and Research Limited ("ESR") solely for the benefit of the Ministry of Health, Public Health Service Providers and other Third Party Beneficiaries as defined in the Contract between ESR and the Ministry of Health, and is strictly subject to the conditions laid out in that Contract. Neither ESR nor any of its employees makes any warranty, express or implied, or assumes any legal liability or responsibility for use of the Report or its contents by any other person or organisation. Guidelines for the Notification of Injuries from Hazardous Substances April 2001 Acknowledgements The author wishes to thank Dr Michael Bates and Melissa Perks (ESR), Sally Gilbert and Helen Saba (Ministry of Health), Dr Donald Campbell (Midcentral Health), Dr Deborah Read (ERMANZ), and Dr Nerida Smith (National Poisons Centre) for useful contributions and helpful suggestions on the construction of these guidelines. Guidelines for the Notification of Injuries from Hazardous Substances April 2001 TABLE OF CONTENTS SUMMARY ........................................................................................................................1 -

Antimigraine Agents, Triptans Review 07/21/2008
Antimigraine Agents, Triptans Review 07/21/2008 Copyright © 2004 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended -

Frovatriptan Versus Zolmitriptan for the Acute Treatment of Migraine: a Double-Blind, Randomized, Multicenter, Italian Study
Neurol Sci (2010) 31 (Suppl 1):S51–S54 DOI 10.1007/s10072-010-0273-x SYMPOSIUM: NEWS IN TREATMENT OF MIGRAINE ATTACK Frovatriptan versus zolmitriptan for the acute treatment of migraine: a double-blind, randomized, multicenter, Italian study Vincenzo Tullo • Gianni Allais • Michel D. Ferrari • Marcella Curone • Eliana Mea • Stefano Omboni • Chiara Benedetto • Dario Zava • Gennaro Bussone Ó The Author(s) 2010. This article is published with open access at Springerlink.com Abstract The objective of this study is to assess patients’ of PF episodes at 2 h was 26% with F and 31% with Z satisfaction with migraine treatment with frovatriptan (F) (p = NS). PR episodes at 2 h were 57% for F and 58% for or zolmitriptan (Z), by preference questionnaire. 133 sub- Z(p = NS). Rate of recurrence was 21 (F) and 24% jects with a history of migraine with or without aura (IHS (Z; p = NS). Time to recurrence within 48 h was better for criteria) were randomized to F 2.5 mg or Z 2.5 mg. The F especially between 4 and 16 h (p \ 0.05). SPF episodes study had a multicenter, randomized, double-blind, cross- were 18 (F) versus 22% (Z; p = NS). Drug-related adverse over design, with each of the two treatment periods lasting events were significantly (p \ 0.05) less under F (3 vs. 10). no more than 3 months. At the end of the study, patients In conclusion, our study suggests that F has a similar were asked to assign preference to one of the treatments efficacy of Z, with some advantage as regards tolerability (primary endpoint). -
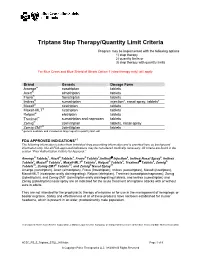
Triptans Step Therapy/Quantity Limit Criteria
Triptans Step Therapy/Quantity Limit Criteria Program may be implemented with the following options 1) step therapy 2) quantity limits or 3) step therapy with quantity limits For Blue Cross and Blue Shield of Illinois Option 1 (step therapy only) will apply. Brand Generic Dosage Form Amerge® naratriptan tablets Axert® almotriptan tablets Frova® frovatriptan tablets Imitrex® sumatriptan injection*, nasal spray, tablets* Maxalt® rizatriptan tablets Maxalt-MLT® rizatriptan tablets Relpax® eletriptan tablets Treximet™ sumatriptan and naproxen tablets Zomig® zolmitriptan tablets, nasal spray Zomig-ZMT® zolmitriptan tablets * generic available and included as target agent in quantity limit edit FDA APPROVED INDICATIONS1-7 The following information is taken from individual drug prescribing information and is provided here as background information only. Not all FDA-approved indications may be considered medically necessary. All criteria are found in the section “Prior Authorization Criteria for Approval.” Amerge® Tablets1, Axert® Tablets2, Frova® Tablets3,Imitrex® injection4, Imitrex Nasal Spray5, Imitrex Tablets6, Maxalt® Tablets7, Maxalt-MLT® Tablets7, Relpax® Tablets8, Treximet™ Tablets9, Zomig® Tablets10, Zomig-ZMT® Tablets10, and Zomig® Nasal Spray11 Amerge (naratriptan), Axert (almotriptan), Frova (frovatriptan), Imitrex (sumatriptan), Maxalt (rizatriptan), Maxalt-MLT (rizatriptan orally disintegrating), Relpax (eletriptan), Treximet (sumatriptan/naproxen), Zomig (zolmitriptan), and Zomig-ZMT (zolmitriptan orally disintegrating) tablets, and Imitrex (sumatriptan) and Zomig (zolmitriptan) nasal spray are all indicated for the acute treatment of migraine attacks with or without aura in adults. They are not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic or basilar migraine. Safety and effectiveness of all of these products have not been established for cluster headache, which is present in an older, predominantly male population. -

Hallucinogens: a Cause of Convulsive Ergot Psychoses
Loma Linda University TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works Loma Linda University Electronic Theses, Dissertations & Projects 6-1976 Hallucinogens: a Cause of Convulsive Ergot Psychoses Sylvia Dahl Winters Follow this and additional works at: https://scholarsrepository.llu.edu/etd Part of the Psychiatry Commons Recommended Citation Winters, Sylvia Dahl, "Hallucinogens: a Cause of Convulsive Ergot Psychoses" (1976). Loma Linda University Electronic Theses, Dissertations & Projects. 976. https://scholarsrepository.llu.edu/etd/976 This Thesis is brought to you for free and open access by TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. It has been accepted for inclusion in Loma Linda University Electronic Theses, Dissertations & Projects by an authorized administrator of TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. For more information, please contact [email protected]. ABSTRACT HALLUCINOGENS: A CAUSE OF CONVULSIVE ERGOT PSYCHOSES By Sylvia Dahl Winters Ergotism with vasoconstriction and gangrene has been reported through the centuries. Less well publicized are the cases of psychoses associated with convulsive ergotism. Lysergic acid amide a powerful hallucinogen having one.-tenth the hallucinogenic activity of LSD-25 is produced by natural sources. This article attempts to show that convulsive ergot psychoses are mixed psychoses caused by lysergic acid amide or similar hallucinogens combined with nervous system -

615.9Barref.Pdf
INDEX Abortifacient, abortifacients bees, wasps, and ants ginkgo, 492 aconite, 737 epinephrine, 963 ginseng, 500 barbados nut, 829 blister beetles goldenseal blister beetles, 972 cantharidin, 974 berberine, 506 blue cohosh, 395 buckeye hawthorn, 512 camphor, 407, 408 ~-escin, 884 hypericum extract, 602-603 cantharides, 974 calamus inky cap and coprine toxicity cantharidin, 974 ~-asarone, 405 coprine, 295 colocynth, 443 camphor, 409-411 ethanol, 296 common oleander, 847, 850 cascara, 416-417 isoxazole-containing mushrooms dogbane, 849-850 catechols, 682 and pantherina syndrome, mistletoe, 794 castor bean 298-302 nutmeg, 67 ricin, 719, 721 jequirity bean and abrin, oduvan, 755 colchicine, 694-896, 698 730-731 pennyroyal, 563-565 clostridium perfringens, 115 jellyfish, 1088 pine thistle, 515 comfrey and other pyrrolizidine Jimsonweed and other belladonna rue, 579 containing plants alkaloids, 779, 781 slangkop, Burke's, red, Transvaal, pyrrolizidine alkaloids, 453 jin bu huan and 857 cyanogenic foods tetrahydropalmatine, 519 tansy, 614 amygdalin, 48 kaffir lily turpentine, 667 cyanogenic glycosides, 45 lycorine,711 yarrow, 624-625 prunasin, 48 kava, 528 yellow bird-of-paradise, 749 daffodils and other emetic bulbs Laetrile", 763 yellow oleander, 854 galanthamine, 704 lavender, 534 yew, 899 dogbane family and cardenolides licorice Abrin,729-731 common oleander, 849 glycyrrhetinic acid, 540 camphor yellow oleander, 855-856 limonene, 639 cinnamomin, 409 domoic acid, 214 rna huang ricin, 409, 723, 730 ephedra alkaloids, 547 ephedra alkaloids, 548 Absorption, xvii erythrosine, 29 ephedrine, 547, 549 aloe vera, 380 garlic mayapple amatoxin-containing mushrooms S-allyl cysteine, 473 podophyllotoxin, 789 amatoxin poisoning, 273-275, gastrointestinal viruses milk thistle 279 viral gastroenteritis, 205 silibinin, 555 aspartame, 24 ginger, 485 mistletoe, 793 Medical Toxicology ofNatural Substances, by Donald G. -

Biased Ligands Differentially Shape the Conformation of The
International Journal of Molecular Sciences Article Biased Ligands Differentially Shape the Conformation of the Extracellular Loop Region in 5-HT2B Receptors Katrin Denzinger, Trung Ngoc Nguyen, Theresa Noonan, Gerhard Wolber and Marcel Bermudez * Institute of Pharmacy, Freie Universität Berlin, Königin-Luise-Strasse 2-4, 14195 Berlin, Germany; [email protected] (K.D.); [email protected] (T.N.N.); [email protected] (T.N.); [email protected] (G.W.) * Correspondence: [email protected] Received: 22 November 2020; Accepted: 18 December 2020; Published: 20 December 2020 Abstract: G protein-coupled receptors are linked to various intracellular transducers, each pathway associated with different physiological effects. Biased ligands, capable of activating one pathway over another, are gaining attention for their therapeutic potential, as they could selectively activate beneficial pathways whilst avoiding those responsible for adverse effects. We performed molecular dynamics simulations with known β-arrestin-biased ligands like lysergic acid diethylamide and ergotamine in complex with the 5-HT2B receptor and discovered that the extent of ligand bias is directly connected with the degree of closure of the extracellular loop region. Given a loose allosteric coupling of extracellular and intracellular receptor regions, we delineate a concept for biased signaling at serotonin receptors, by which conformational interference with binding pocket closure restricts the signaling repertoire of the receptor. Molecular docking studies of biased ligands gathered from the BiasDB demonstrate that larger ligands only show plausible docking poses in the ergotamine-bound structure, highlighting the conformational constraints associated with bias. This emphasizes the importance of selecting the appropriate receptor conformation on which to base virtual screening workflows in structure-based drug design of biased ligands.