Differential Diagnosis of Myotonic Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spectrum of CLCN1 Mutations in Patients with Myotonia Congenita in Northern Scandinavia
European Journal of Human Genetics (2001) 9, 903 ± 909 ã 2001 Nature Publishing Group All rights reserved 1018-4813/01 $15.00 www.nature.com/ejhg ARTICLE Spectrum of CLCN1 mutations in patients with myotonia congenita in Northern Scandinavia Chen Sun*,1, Lisbeth Tranebjñrg*,1, Torberg Torbergsen2,GoÈsta Holmgren3 and Marijke Van Ghelue1,4 1Department of Medical Genetics, University Hospital of Tromsù, Tromsù, Norway; 2Department of Neurology, University Hospital of Tromsù, Tromsù, Norway; 3Department of Clinical Genetics, University Hospital of UmeaÊ, UmeaÊ,Sweden;4Department of Biochemistry, Section Molecular Biology, University of Tromsù, Tromsù, Norway Myotonia congenita is a non-dystrophic muscle disorder affecting the excitability of the skeletal muscle membrane. It can be inherited either as an autosomal dominant (Thomsen's myotonia) or an autosomal recessive (Becker's myotonia) trait. Both types are characterised by myotonia (muscle stiffness) and muscular hypertrophy, and are caused by mutations in the muscle chloride channel gene, CLCN1. At least 50 different CLCN1 mutations have been described worldwide, but in many studies only about half of the patients showed mutations in CLCN1. Limitations in the mutation detection methods and genetic heterogeneity might be explanations. In the current study, we sequenced the entire CLCN1 gene in 15 Northern Norwegian and three Northern Swedish MC families. Our data show a high prevalence of myotonia congenita in Northern Norway similar to Northern Finland, but with a much higher degree of mutation heterogeneity. In total, eight different mutations and three polymorphisms (T87T, D718D, and P727L) were detected. Three mutations (F287S, A331T, and 2284+5C4T) were novel while the others (IVS1+3A4T, 979G4A, F413C, A531V, and R894X) have been reported previously. -

Paramyotonia Congenita
Paramyotonia congenita Description Paramyotonia congenita is a disorder that affects muscles used for movement (skeletal muscles). Beginning in infancy or early childhood, people with this condition experience bouts of sustained muscle tensing (myotonia) that prevent muscles from relaxing normally. Myotonia causes muscle stiffness that typically appears after exercise and can be induced by muscle cooling. This stiffness chiefly affects muscles in the face, neck, arms, and hands, although it can also affect muscles used for breathing and muscles in the lower body. Unlike many other forms of myotonia, the muscle stiffness associated with paramyotonia congenita tends to worsen with repeated movements. Most people—even those without muscle disease—feel that their muscles do not work as well when they are cold. This effect is dramatic in people with paramyotonia congenita. Exposure to cold initially causes muscle stiffness in these individuals, and prolonged cold exposure leads to temporary episodes of mild to severe muscle weakness that may last for several hours at a time. Some older people with paramyotonia congenita develop permanent muscle weakness that can be disabling. Frequency Paramyotonia congenita is an uncommon disorder; it is estimated to affect fewer than 1 in 100,000 people. Causes Mutations in the SCN4A gene cause paramyotonia congenita. This gene provides instructions for making a protein that is critical for the normal function of skeletal muscle cells. For the body to move normally, skeletal muscles must tense (contract) and relax in a coordinated way. Muscle contractions are triggered by the flow of positively charged atoms (ions), including sodium, into skeletal muscle cells. The SCN4A protein forms channels that control the flow of sodium ions into these cells. -

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

Experiences of Rare Diseases: an Insight from Patients and Families
Experiences of Rare Diseases: An Insight from Patients and Families Unit 4D, Leroy House 436 Essex Road London N1 3QP tel: 02077043141 fax: 02073591447 [email protected] www.raredisease.org.uk By Lauren Limb, Stephen Nutt and Alev Sen - December 2010 Web and press design www.raredisease.org.uk WordsAndPeople.com About Rare Disease UK Rare Disease UK (RDUK) is the national alliance for people with rare diseases and all who support them. Our membership is open to all and includes patient organisations, clinicians, researchers, academics, industry and individuals with an interest in rare diseases. RDUK was established by Genetic RDUK is campaigning for a Alliance UK, the national charity strategy for integrated service of over 130 patient organisations delivery for rare diseases. This supporting all those affected by would coordinate: genetic conditions, in conjunction with other key stakeholders | Research in November 2008 following the European Commission’s | Prevention and diagnosis Communication on Rare Diseases: | Treatment and care Europe’s Challenges. | Information Subsequently RDUK successfully | Commissioning and planning campaigned for the adoption of the Council of the European into one cohesive strategy for all Union’s Recommendation on patients affected by rare disease in an action in the field of rare the UK. As well as securing better diseases. The Recommendation outcomes for patients, a strategy was adopted unanimously by each would enable the most effective Member State of the EU (including use of NHS resources. the -

Difference in Allelic Expression of the CLCN1 Gene and the Possible Influence on the Myotonia Congenita Phenotype
European Journal of Human Genetics (2004) 12, 738–743 & 2004 Nature Publishing Group All rights reserved 1018-4813/04 $30.00 www.nature.com/ejhg ARTICLE Difference in allelic expression of the CLCN1 gene and the possible influence on the myotonia congenita phenotype Morten Dun1*, Eskild Colding-Jrgensen2, Morten Grunnet3,5, Thomas Jespersen3, John Vissing4 and Marianne Schwartz1 1Department of Clinical Genetics, 4062, University Hospital, Rigshospitalet, Blegdamsvej 9, DK-2100 Copenhagen, Denmark; 2Department of Clinical Neurophysiology 3063,University Hospital, Rigshospitalet, Blegdamsvej 9, DK- 2100 Copenhagen, Denmark; 3Department of Medical Physiology, The Panum Institute, University of Copenhagen, Blegdamsvej 3, DK-2200 Copenhagen N, Denmark; 4Department of Neurology and The Copenhagen Muscle Research Center, University Hospital, Rigshospitalet, Blegdamsvej 9, DK-2100 Copenhagen, Denmark Mutations in the CLCN1 gene, encoding a muscle-specific chloride channel, can cause either recessive or dominant myotonia congenita (MC). The recessive form, Becker’s myotonia, is believed to be caused by two loss-of-function mutations, whereas the dominant form, Thomsen’s myotonia, is assumed to be a consequence of a dominant-negative effect. However, a subset of CLCN1 mutations can cause both recessive and dominant MC. We have identified two recessive and two dominant MC families segregating the common R894X mutation. Real-time quantitative RT-PCR did not reveal any obvious association between the total CLCN1 mRNA level in muscle and the mode of inheritance, but the dominant family with the most severe phenotype expressed twice the expected amount of the R894X mRNA allele. Variation in allelic expression has not previously been described for CLCN1, and our finding suggests that allelic variation may be an important modifier of disease progression in myotonia congenita. -

Current and Emerging Therapies in Becker Muscular Dystrophy (BMD)
Acta Myologica • 2019; XXXVIII: p. 172-179 OPEN ACCESS © Gaetano Conte Academy - Mediterranean Society of Myology Current and emerging therapies in Becker muscular dystrophy (BMD) Corrado Angelini, Roberta Marozzo and Valentina Pegoraro Neuromuscular Center, IRCCS San Camillo Hospital, Venice, Italy Becker muscular dystrophy (BMD) has onset usually in child- tients with a deletion in the dystrophin gene that have nor- hood, frequently by 11 years. BMD can present in several ways mal muscle strength and endurance, but present high CK, such as waddling gait, exercise related cramps with or with- and so far their follow-up and treatment recommenda- out myoglobinuria. Rarely cardiomyopathy might be the pre- senting feature. The evolution is variable. BMD is caused by tions are still a matter of debate. Patients with early cardi- dystrophin deficiency due to inframe deletions, mutations or omyopathy are also a possible variant of BMD (4, 5) and duplications in dystrophin gene (Xp21.2) We review here the may be susceptible either to specific drug therapy and/or evolution and current therapy presenting a personal series of to cardiac transplantation (6-8). Here we cover emerging cases followed for over two decades, with multifactorial treat- therapies considering follow-up, and exemplifying some ment regimen. Early treatment includes steroid treatment that phenotypes and treatments by a few study cases. has been analized and personalized for each case. Early treat- ment of cardiomyopathy with ACE inhibitors is recommended and referral for cardiac transplantation is appropriate in severe cases. Management includes multidisciplinary care with physi- Pathophysiology and rationale of otherapy to reduce joint contractures and prolong walking. -

Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

This Letter Is for Families with Variant(S) in the Titin Gene, Also
This letter is for families with variant(s) in the Titin gene , also abbreviated as TTN . Changes in the Titin protein may cause muscle weakness as well as heart problems . You will need to discuss with your doctor if and how your Titin variant affects your health. What is Titin? Titin is a very large protein. It’s huge! In fact, Titin is the largest protein in the human body. The Titin protein is located in each of the individual muscle cells in our bodies. It is also found in the heart, which is a very specialized muscle. Muscles need Titin in order to work and move. You can learn more about Titin here: http://titinmyopathy.com . What is a Titin Myopathy? In medical terms, “Myo” refers to muscle and “-opathy” at the end of a word means that the word describes a medical disease or condition. So “myopathy” is a medical illness involving muscles. Myopathies result in muscle weakness and muscle fatigue. “Titin Myopathy” is a specific category of myopathy where the muscle problem is caused by a change in the Titin gene and subsequently the protein. What is a Titin-related Dystrophy? A Titin dystrophy is a muscle disorder where muscle cells break down. Dystrophies generally result in weakness that gets worse over time. A common heart problem caused by variants in the Titin gene is known as dilated cardiomyopathy. Sometimes other heart issues are also present in people with changes in their Titin gene. It is a good idea to have a checkup from a heart doctor if you have even a single variant in the Titin gene. -
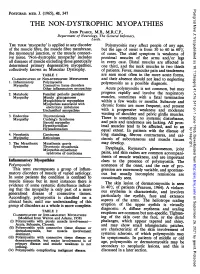
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Periodic Paralysis
Periodic Paralysis In Focus Dear Readers Fast Facts This “In Focus” report is the third in a series of MDA’s three-year commitment for all Hypokalemic periodic paralysis MDA comprehensive reports about the latest in periodic paralysis research as of March Hypokalemic PP can begin anywhere from neuromuscular disease research and manage- 2009 is $1,938,367. The Association’s early childhood to the 30s, with periodic ment. allocation for research on hyperkalemic attacks of severe weakness lasting hours This report focuses on the periodic and hypokalemic periodic paralysis to days. The frequency of attacks gener- paralyses, a group of disorders that result from research since 1950 is $8,125,341. ally lessens in the 40s or 50s. Permanent malfunctions in so-called ion channels, micro- MDA’s allocation for the recently weakness may persist between attacks, scopic tunnels that make possible high-speed identified Andersen-Tawil syndrome usually beginning in middle age and pro- movement of electrically charged particles is $515,430 since 2001. MDA is cur- gressing slowly over years. across barriers inside cells and between cells rently funding 11 grants in the periodic The most common underlying cause and their surroundings. paralyses. is any of several genetic mutations in When ion channels fail to open or close The periodic paralyses are gener- a gene on chromosome 1 that carries according to an exquisitely fine-tuned program, ally divided into hyperkalemic periodic instructions for a calcium channel protein episodes of paralysis of the skeletal muscles paralysis, hypokalemic periodic paralysis in skeletal muscle fibers. When this chan- and even temporary irregularities in the heart- and Andersen-Tawil syndrome. -

Neuromyotonia in Hereditary Motor Neuropathy J Neurol Neurosurg Psychiatry: First Published As 10.1136/Jnnp.54.3.230 on 1 March 1991
230 Journal ofNeurology, Neurosurgery, and Psychiatry 1991;54:230-235 Neuromyotonia in hereditary motor neuropathy J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.54.3.230 on 1 March 1991. Downloaded from A F Hahn, A W Parkes, C F Bolton, S A Stewart Abstract Case II2 Two siblings with a distal motor This 15 year old boy had always been clumsy. neuropathy experienced cramping and Since the age of 10, he had noticed generalised difficulty in relaxing their muscles after muscle stiffness which increased with physical voluntary contraction. Electromyogra- activity such as walking upstairs, running and phic recordings at rest revealed skating. For some time, he was aware of repetitive high voltage spontaneous elec- difficulty in releasing his grip and his fingers trical discharges that were accentuated tended to cramp on writing. He had noticed after voluntary contraction and during involuntary twitching of his fingers, forearm ischaemia. Regional neuromuscular muscles and thighs at rest and it was more blockage with curare indicated hyperex- pronounced after a forceful voluntary con- citability of peripheral nerve fibres and traction. Muscle cramping and spontaneous nerve block suggested that the ectopic muscle activity were particularly unpleasant activity originated in proximal segments when he re-entered the house in the winter, of the nerve. Symptoms were improved for example, after a game of hockey. Since the with diphenylhydantoin, carbamazepine age of twelve, he had noticed a tendency to and tocainide. trip. Subsequently he developed bilateral foot drop and weakness of his hands. He denied sensory symptoms and perspired only with The term "neuromyotonia" was coined by exertion.