FOXRED1, Encoding a FAD-Dependent Oxidoreductase Complex-I Specific Molecular Chaperone, Is Mutated in Infantile-Onset Mitochondrial Encephalopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

High-Throughput, Pooled Sequencing Identifies Mutations in NUBPL And
ARTICLES High-throughput, pooled sequencing identifies mutations in NUBPL and FOXRED1 in human complex I deficiency Sarah E Calvo1–3,10, Elena J Tucker4,5,10, Alison G Compton4,10, Denise M Kirby4, Gabriel Crawford3, Noel P Burtt3, Manuel Rivas1,3, Candace Guiducci3, Damien L Bruno4, Olga A Goldberger1,2, Michelle C Redman3, Esko Wiltshire6,7, Callum J Wilson8, David Altshuler1,3,9, Stacey B Gabriel3, Mark J Daly1,3, David R Thorburn4,5 & Vamsi K Mootha1–3 Discovering the molecular basis of mitochondrial respiratory chain disease is challenging given the large number of both mitochondrial and nuclear genes that are involved. We report a strategy of focused candidate gene prediction, high-throughput sequencing and experimental validation to uncover the molecular basis of mitochondrial complex I disorders. We created seven pools of DNA from a cohort of 103 cases and 42 healthy controls and then performed deep sequencing of 103 candidate genes to identify 151 rare variants that were predicted to affect protein function. We established genetic diagnoses in 13 of 60 previously unsolved cases using confirmatory experiments, including cDNA complementation to show that mutations in NUBPL and FOXRED1 can cause complex I deficiency. Our study illustrates how large-scale sequencing, coupled with functional prediction and experimental validation, can be used to identify causal mutations in individual cases. Complex I of the mitochondrial respiratory chain is a large ~1-MDa assembly factors are probably required, as suggested by the 20 factors macromolecular machine composed of 45 protein subunits encoded necessary for assembly of the smaller complex IV9 and by cohort by both the nuclear and mitochondrial (mtDNA) genomes. -

Analysis of the Impact of Silver Ions on Creatine Amidinohydrolase
ActaBIOMATERIALIA Acta Biomaterialia 1 (2005) 183–191 www.actamat-journals.com A stable three enzyme creatinine biosensor. 2. Analysis of the impact of silver ions on creatine amidinohydrolase Jason A. Berberich b,1, Lee Wei Yang a, Ivet Bahar a, Alan J. Russell b,* a Center for Computational Biology & Bioinformatics and Department of Molecular Genetics & Biochemistry, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA b Department of Surgery, McGowan Institute for Regenerative Medicine, University of Pittsburgh, Pittsburgh, PA 15219, USA Received 11 October 2004; received in revised form 26 November 2004; accepted 28 November 2004 Abstract The enzyme creatine amidinohydrolase is a clinically important enzyme used in the determination of creatinine in blood and urine. Continuous use biosensors are becoming more important in the clinical setting; however, long-use creatinine biosensors have not been commercialized due to the complexity of the three-enzyme creatinine biosensor and the lack of stability of its components. This paper, the second in a series of three, describes the immobilization and stabilization of creatine amidinohydrolase. Creatine amidinohydrolase modified with poly(ethylene glycol) activated with isocyanate retains significant activity after modification. The enzyme was successfully immobilized into hydrophilic polyurethanes using a reactive prepolymer strategy. The immobilized enzyme retained significant activity over a 30 day period at 37 °C and was irreversibly immobilized into the polymer. Despite being stabilized in the polymer, the enzyme remained highly sensitive to silver ions which were released from the amperometric electrodes. Computational analysis of the structure of the protein using the Gaussian network model suggests that the silver ions bind tightly to a cysteine residue preventing normal enzyme dynamics and catalysis. -

FOXRED1 (D-4): Sc-377010
SANTA CRUZ BIOTECHNOLOGY, INC. FOXRED1 (D-4): sc-377010 BACKGROUND APPLICATIONS FOXRED1 (FAD-dependent oxidoreductase domain-containing protein 1), also FOXRED1 (D-4) is recommended for detection of FOXRED1 of human origin known as FP634, is a 486 amino acid single-pass membrane protein. Utilizing by Western Blotting (starting dilution 1:100, dilution range 1:100-1:1000), FAD as a cofactor, FOXRED1 may act as a chaperone protein essential for the immunoprecipitation [1-2 µg per 100-500 µg of total protein (1 ml of cell function of mitochondrial complex I. Mutations to FOXRED1 may result in lysate)], immunofluorescence (starting dilution 1:50, dilution range 1:50- mitochondrial complex I deficiency (MT-C1D), which results in a wide range 1:500), immunohistochemistry (including paraffin-embedded sections) of clinical maladies from lethal neonatal disease to adult onset neurodegen- (starting dilution 1:50, dilution range 1:50-1:500) and solid phase ELISA erative disorders. Common phenotypes of MT-C1D include cardiomyopathy, (starting dilution 1:30, dilution range 1:30-1:3000). liver disease, Leigh syndrome, Leber hereditary optic neuropathy, and some Suitable for use as control antibody for FOXRED1 siRNA (h): sc-96988, forms of Parkinson disease. FOXRED1 exists as three alternatively spliced FOXRED1 shRNA Plasmid (h): sc-96988-SH and FOXRED1 shRNA (h) isoforms and is encoded by a gene mapping to human chromosome 11q24.2. Lentiviral Particles: sc-96988-V. With approximately 135 million base pairs and 1,400 genes, chromosome 11 makes up around 4% of human genomic DNA and is considered a gene and Molecular Weight of FOXRED1 isoform 1: 54 kDa. -

Supplementary Materials
Supplementary Materials COMPARATIVE ANALYSIS OF THE TRANSCRIPTOME, PROTEOME AND miRNA PROFILE OF KUPFFER CELLS AND MONOCYTES Andrey Elchaninov1,3*, Anastasiya Lokhonina1,3, Maria Nikitina2, Polina Vishnyakova1,3, Andrey Makarov1, Irina Arutyunyan1, Anastasiya Poltavets1, Evgeniya Kananykhina2, Sergey Kovalchuk4, Evgeny Karpulevich5,6, Galina Bolshakova2, Gennady Sukhikh1, Timur Fatkhudinov2,3 1 Laboratory of Regenerative Medicine, National Medical Research Center for Obstetrics, Gynecology and Perinatology Named after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia 2 Laboratory of Growth and Development, Scientific Research Institute of Human Morphology, Moscow, Russia 3 Histology Department, Medical Institute, Peoples' Friendship University of Russia, Moscow, Russia 4 Laboratory of Bioinformatic methods for Combinatorial Chemistry and Biology, Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry of the Russian Academy of Sciences, Moscow, Russia 5 Information Systems Department, Ivannikov Institute for System Programming of the Russian Academy of Sciences, Moscow, Russia 6 Genome Engineering Laboratory, Moscow Institute of Physics and Technology, Dolgoprudny, Moscow Region, Russia Figure S1. Flow cytometry analysis of unsorted blood sample. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S2. Flow cytometry analysis of unsorted liver stromal cells. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S3. MiRNAs expression analysis in monocytes and Kupffer cells. Full-length of heatmaps are presented. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
Differential Gene Expression in Tomato Fruit and Colletotrichum
Barad et al. BMC Genomics (2017) 18:579 DOI 10.1186/s12864-017-3961-6 RESEARCH Open Access Differential gene expression in tomato fruit and Colletotrichum gloeosporioides during colonization of the RNAi–SlPH tomato line with reduced fruit acidity and higher pH Shiri Barad1,2, Noa Sela3, Amit K. Dubey1, Dilip Kumar1, Neta Luria1, Dana Ment1, Shahar Cohen4, Arthur A. Schaffer4 and Dov Prusky1* Abstract Background: The destructive phytopathogen Colletotrichum gloeosporioides causes anthracnose disease in fruit. During host colonization, it secretes ammonia, which modulates environmental pH and regulates gene expression, contributing to pathogenicity. However, the effect of host pH environment on pathogen colonization has never been evaluated. Development of an isogenic tomato line with reduced expression of the gene for acidity, SlPH (Solyc10g074790.1.1), enabled this analysis. Total RNA from C. gloeosporioides colonizing wild-type (WT) and RNAi– SlPH tomato lines was sequenced and gene-expression patterns were compared. Results: C. gloeosporioides inoculation of the RNAi–SlPH line with pH 5.96 compared to the WT line with pH 4.2 showed 30% higher colonization and reduced ammonia accumulation. Large-scale comparative transcriptome analysis of the colonized RNAi–SlPH and WT lines revealed their different mechanisms of colonization-pattern activation: whereas the WT tomato upregulated 13-LOX (lipoxygenase), jasmonic acid and glutamate biosynthesis pathways, it downregulated processes related to chlorogenic acid biosynthesis II, phenylpropanoid biosynthesis and hydroxycinnamic acid tyramine amide biosynthesis; the RNAi–SlPH line upregulated UDP-D-galacturonate biosynthesis I and free phenylpropanoid acid biosynthesis, but mainly downregulated pathways related to sugar metabolism, such as the glyoxylate cycle and L-arabinose degradation II. -

Ykt6 Membrane-To-Cytosol Cycling Regulates Exosomal Wnt Secretion
bioRxiv preprint doi: https://doi.org/10.1101/485565; this version posted December 3, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Ykt6 membrane-to-cytosol cycling regulates exosomal Wnt secretion Karen Linnemannstöns1,2, Pradhipa Karuna1,2, Leonie Witte1,2, Jeanette Kittel1,2, Adi Danieli1,2, Denise Müller1,2, Lena Nitsch1,2, Mona Honemann-Capito1,2, Ferdinand Grawe3,4, Andreas Wodarz3,4 and Julia Christina Gross1,2* Affiliations: 1Hematology and Oncology, University Medical Center Goettingen, Goettingen, Germany. 2Developmental Biochemistry, University Medical Center Goettingen, Goettingen, Germany. 3Molecular Cell Biology, Institute I for Anatomy, University of Cologne Medical School, Cologne, Germany 4Cluster of Excellence-Cellular Stress Response in Aging-Associated Diseases (CECAD), Cologne, Germany *Correspondence: Dr. Julia Christina Gross, Hematology and Oncology/Developmental Biochemistry, University Medical Center Goettingen, Justus-von-Liebig Weg 11, 37077 Goettingen Germany Abstract Protein trafficking in the secretory pathway, for example the secretion of Wnt proteins, requires tight regulation. These ligands activate Wnt signaling pathways and are crucially involved in development and disease. Wnt is transported to the plasma membrane by its cargo receptor Evi, where Wnt/Evi complexes are endocytosed and sorted onto exosomes for long-range secretion. However, the trafficking steps within the endosomal compartment are not fully understood. The promiscuous SNARE Ykt6 folds into an auto-inhibiting conformation in the cytosol, but a portion associates with membranes by its farnesylated and palmitoylated C-terminus. Here, we demonstrate that membrane detachment of Ykt6 is essential for exosomal Wnt secretion. -

Biogenesis of NDUFS3-Less Complex I Indicates TMEM126A/OPA7 As an Assembly Factor of the ND4-Module
bioRxiv preprint doi: https://doi.org/10.1101/2020.10.22.350587; this version posted October 23, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Biogenesis of NDUFS3-less complex I indicates TMEM126A/OPA7 as an assembly factor of the ND4-module Running title: NDUFS3-dependent CI disassembly pathway Luigi D’Angelo,1* Elisa Astro,1* Monica De Luise,2 Ivana Kurelac,2 Nikkitha Umesh-Ganesh,2 Shujing Ding,3 Ian M. Fearnley,3 Massimo Zeviani,3,4 Giuseppe Gasparre,2,5 Anna Maria Porcelli,1,6# Erika Fernandez-Vizarra,3,7# and Luisa Iommarini1# 1Department of Pharmacy and Biotechnology (FABIT), University of Bologna, Bologna, Italy 2Department of Medical and Surgical Sciences (DIMEC), University of Bologna, Bologna, Italy 3Medical Research Council-Mitochondrial Biology Unit, University of Cambridge, Cambridge, UK 4Venetian Institute of Molecular Medicine, Via Orus 2, 35128 Padova, Italy; Department of Neurosciences, University of Padova, via Giustiniani 2, 35128 Padova, Italy 5Center for Applied Biomedical Research (CRBA), University of Bologna, Bologna, Italy 6Interdepartmental Center of Industrial Research (CIRI) Life Science and Health Technologies, University of Bologna, Ozzano dell'Emilia, Italy 7Institute of Molecular, Cell and Systems Biology, University of Glasgow, Glasgow, UK. *Co-first authors #Co-last authors To whom correspondence should be addressed: Luisa Iommarini Department of Pharmacy and Biotechnology (FABIT) University of Bologna Via Francesco Selmi 3, 40126 Bologna, Italy Tel. +39 051 2091282 e-mail [email protected] Erika Fernandez-Vizarra Institute of Molecular, Cell and Systems Biology University of Glasgow University Avenue Glasgow G12 8QQ, UK Tel. -
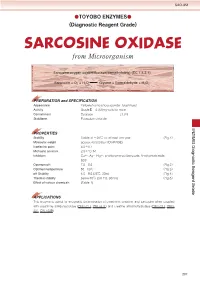
SARCOSINE OXIDASE from Microorganism
SAO-351 ●TOYOBO ENZYMES● (Diagnostic Reagent Grade) SARCOSINE OXIDASE from Microorganism Sarcosine:oxygen oxidoreductase(demethylating) (EC 1.5.3.1) Sarcosine + O2 + H2O Glycine + Formaldehyde + H2O2 PREPARATION and SPECIFICATION Appearance : Yellowish amorphous powder, lyophilized Activity : GradeⅢ 8.0U/mg-solid or more Contaminant : Catalase ≤1.0% Stabilizers : Potassium chloride PROPERTIES Stability : Stable at −20℃ for at least one year (Fig.1) Molecular weight : approx.43,000 (by SDS-PAGE) Isoelectric point : 4.8±0.1 Michaelis constant : 2.8×10-3M Inhibitors : Cu++, Ag+, Hg++, p-chloromercuribenzoate, N-ethylmaleimide, SDS Optimum pH : 7.5−8.5 (Fig.2) Optimum temperature : 55−60℃ (Fig.3) pH Stability : 6.0−9.5 (25℃, 20hr) (Fig.4) Thermal stability : below 60℃ (pH 7.5, 30min) (Fig.5) Effect of various chemicals : (Table.1) APPLICATIONS This enzyme is useful for enzymatic determination of creatinine, creatine, and sarcosine when coupled with creatinine amidohydrolase (CNH-211, CNH-311) and creatine amidinohydrolase (CRH-211, CRH- 221, CRH-229). 237 SAO-351 ASSAY Principle: sarcosine oxidase Sarcosine+O2+H2O Glycine+Formaldehyde+H2O2 peroxidase 2H2O2+4-Aminoantipyrine+Phenol Quinoneimine dye+4H2O Unit definition: One unit causes the formation of one micromole of hydrogen peroxide (half a micromole of quinoneimine dye) per minute under the conditions described below. Method: Reagents A. Sarcosine solution : 0.2M[Weight 1.78g of sarcosine (MW=89.09), dissolve in 80ml of 0.125M Tris- HCl buffer, pH8.0 containing 0.125% of Triton X-100 and, after adjusting pH 8.0 at 25℃ with 1.0N NaOH or 1.0N HCl, fill up to 100ml with H2O.](Stable for one week if stored at 0−5℃) B. -

Leigh Syndrome
Leigh syndrome What is Leigh syndrome? Leigh syndrome is an inherited progressive neurodegenerative disease characterized by developmental delays or regression, low muscle tone, neuropathy, and severe episodes of illness that can lead to early death.1,2 Individuals with Leigh syndrome have defects in one of many proteins involved in the mitochondrial respiratory chain complexes that produce energy in cells.1 These protein defects cause lesions in tissues that require large amounts of energy, including the brainstem, thalamus, basal ganglia, cerebellum, and spinal cord.1 Clinical symptoms depend on which areas of the central nervous system are involved.1,2 Leigh syndrome is also known as subacute necrotizing encephalomyelopathy.3 What are the symptoms of Leigh syndrome and what treatment is available? Leigh syndrome is a disease that varies in age at onset and rate of progression. Signs of Leigh syndrome can be seen before birth, but are usually noticed soon after birth. Signs and symptoms may include: 2,3,4 • Hypotonia (low muscle tone) • Intellectual and physical developmental delay and regression • Digestive problems and failure to thrive • Cerebellar ataxia (difficulty coordinating movements) • Peripheral neuropathy (disease affecting nerves) • Hypertrophic cardiomyopathy • Breathing problems, leading to respiratory failure • Metabolic or neurological crisis (serious episode of illness) often triggered by an infection During a crisis, symptoms can progress to respiratory problems, seizures, coma, and possibly death. There is no cure for Leigh syndrome. Treatment is supportive. Approximately 50% of affected individuals die by three years of age, although some patients may survive beyond childhood.4 How is Leigh Syndrome inherited? Autosomal recessive Leigh syndrome is caused by mutations in at least 36 different genes,3 including FOXRED1, NDUFAF2, NDUFS4, NDUFS7, NDUFV1, COX15, SURF1 and LRPPRC. -

(12) United States Patent (10) Patent No.: US 6,867,012 B2 Kishimoto Et Al
USOO6867O12B2 (12) United States Patent (10) Patent No.: US 6,867,012 B2 Kishimoto et al. (45) Date of Patent: Mar. 15, 2005 (54) DETERMINATION METHOD OF FOREIGN PATENT DOCUMENTS BIOLOGICAL COMPONENT AND REAGENT EP O 437 373 A 7/1991 KIT USED THEREFOR EP O 477 OO1 A 3/1992 JP P2001-17198 A 1/2001 (75) Inventors: Takahide Kishimoto, Tsuruga (JP); WO WO 99/47559 A 9/1999 Atsushi Sogabe, Tsuruga (JP); Shizuo WO WO OO/28071 A 5/2000 Hattori, Tsuruga (JP); Masanori Oka, Tsuruga (JP); Yoshihisa Kawamura, OTHER PUBLICATIONS Tsuruga (JP) van Dijken et al (Archives of microbiol, V.111(1-2), pp (73) Assignee: Toyo Boseki Kabushiki Kaisha, Osaka 77-83,(Dec. 1976)(Abstract Only).* (JP) (List continued on next page.) (*) Notice: Subject to any disclaimer, the term of this Primary Examiner Louise N. Leary patent is extended or adjusted under 35 (74) Attorney, Agent, or Firm-Kenyon & Kenyon U.S.C. 154(b) by 330 days. (57) ABSTRACT The present invention provides novel glutathione-dependent (21) Appl. No.: 09/998,130 formaldehyde dehydrogenase that makes possible quantita (22) Filed: Dec. 3, 2001 tive measurement of formaldehyde by cycling reaction, and a determination method of formaldehyde and biological (65) Prior Publication Data components, Such as creatinine, creatine, and homocysteine, US 2002/0119507 A1 Aug. 29, 2002 which produces formaldehyde as a reaction intermediate. In addition, the present invention provides a reagent kit for the (30) Foreign Application Priority Data above-mentioned determination method. The present inven tion provides a novel determination method of a homocys Dec. -

Produktinformation
Produktinformation Diagnostik & molekulare Diagnostik Laborgeräte & Service Zellkultur & Verbrauchsmaterial Forschungsprodukte & Biochemikalien Weitere Information auf den folgenden Seiten! See the following pages for more information! Lieferung & Zahlungsart Lieferung: frei Haus Bestellung auf Rechnung SZABO-SCANDIC Lieferung: € 10,- HandelsgmbH & Co KG Erstbestellung Vorauskassa Quellenstraße 110, A-1100 Wien T. +43(0)1 489 3961-0 Zuschläge F. +43(0)1 489 3961-7 [email protected] • Mindermengenzuschlag www.szabo-scandic.com • Trockeneiszuschlag • Gefahrgutzuschlag linkedin.com/company/szaboscandic • Expressversand facebook.com/szaboscandic SANTA CRUZ BIOTECHNOLOGY, INC. FOXRED1 siRNA (m): sc-145230 BACKGROUND STORAGE AND RESUSPENSION FOXRED1 (FAD-dependent oxidoreductase domain-containing protein 1), also Store lyophilized siRNA duplex at -20° C with desiccant. Stable for at least known as FP634, is a 486 amino acid single-pass membrane protein. Utilizing one year from the date of shipment. Once resuspended, store at -20° C, FAD as a cofactor, FOXRED1 may act as a chaperone protein essential for the avoid contact with RNAses and repeated freeze thaw cycles. function of mitochondrial complex I. Mutations to FOXRED1 may result in Resuspend lyophilized siRNA duplex in 330 µl of the RNAse-free water mitochondrial complex I deficiency (MT-C1D), which results in a wide range provided. Resuspension of the siRNA duplex in 330 µl of RNAse-free water of clinical maladies from lethal neonatal disease to adult onset neurodegen- makes a 10 µM solution in a 10 µM Tris-HCl, pH 8.0, 20 mM NaCl, 1 mM erative disorders. Common phenotypes of MT-C1D include cardiomyopathy, EDTA buffered solution. liver disease, Leigh syndrome, Leber hereditary optic neuropathy, and some forms of Parkinson disease.